Translate this page into:
Basal cell carcinoma in the North Indian population: Clinicopathologic review and immunohistochemical analysis
2 Department of Dermatology, Safdarjang Hospital Campus, Post Box 4909, New Delhi - 110 029, India
Correspondence Address:
Avninder Singh
Institute of Pathology, Safdarjang Campus, Post Box 4909, New Delhi - 110 029
India
| How to cite this article: Malhotra P, Singh A, Ramesh V. Basal cell carcinoma in the North Indian population: Clinicopathologic review and immunohistochemical analysis. Indian J Dermatol Venereol Leprol 2011;77:328-330 |
Sir,
Basal cell carcinoma (BCC) is the most common malignant cutaneous neoplasm worldwide. Gross differences are noted in the percentage of skin cancer in the Asians (2-4%) and Blacks (1-2%) as compared to the Caucasians (35-40%). [1] The existing literature on clinicopathologic features of BCC in India is scant and does not explore the pathogenesis of the tumor. [2],[3],[4]
Clinical parameters and histomorphology were studied in 34 consecutive cases of clinically diagnosed BCC (from January 2007 to December 2009). There was no history of retinoids or imiquimod therapy in any of the patients. Immunohistochemical expression of p53, Bcl-2, and Bax in >10% cells and PCNA in > 5% cells was considered positive. Biopsies from patients of melasma were used as controls.
The male-to-female ratio was 1.6:1 with the highest prevalence (44%) in 40-60 years of age. The age of patients ranged from 28 to 102 years. A total of 91.2% lesions occurred on sun-exposed areas of head and neck. The most common location was the medial/lateral canthus of the eye. The three lesions on nonexposed sites included thigh, vulva, and trunk. A total of 35.2% (12/34) of the lesions were clinically pigmented [[Figure - 1]a]. A fair proportion of patients presented with advanced lesions [[Figure - 1]b] some of which generated a clinical diagnosis of squamous cell carcinoma.
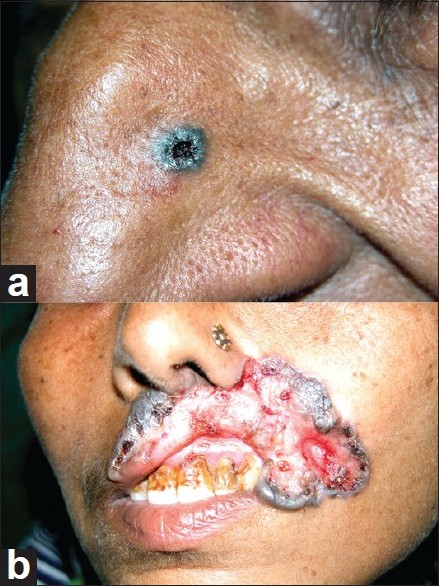 |
| Figure 1: (a) Pigmented lesion on the lateral border of the nose. (b) A large ulcerated lesion on the lip |
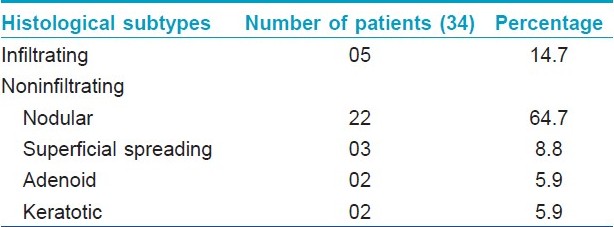
The duration of lesions ranged from 6 months to 25 years. The lesions ranged in size from small pearly papules measuring 0.5 Χ 0.5 cm to large hyperpigmented lesions measuring 8 Χ 5 cm. A solid-nodular variant was the most common histological subtype ([[Figure - 2]a]; 64.7%) followed by infiltrating (14.7%; [Table - 1]). Four of five (80%) cases of the infiltrating variant had positive surgical margins. The pigmentation of tumor cells was noted in 15 of 34 (44.2%) of cases as against nonpigmented (55.8%). The patients presenting with advanced lesions tended to show infiltrative morphology.
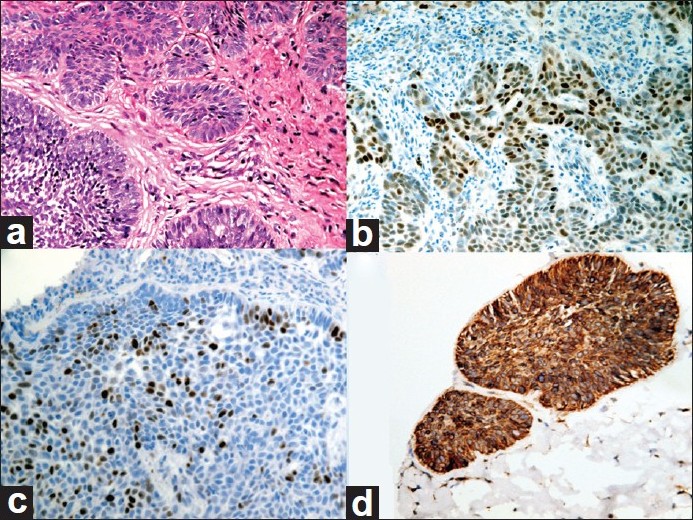 |
| Figure 2: (a) Basal cell carcinoma, solid-nodular variant (H and E, ×400). (b) Nuclear immunoreactivity against p53 (×400). (c) Nuclear immunoreactivity against PCNA (×400). (d) Diffuse cytoplasmic immunoreactivity against Bcl-2 (×400) |
P53 positivity was seen in 17.6% (6/34) cases. Five of these were the infiltrating variant and one was a recurrent nodular BCC [[Figure - 2]b]. The mean age of this group was 70 years compared to 55 years in the non-p53 expressing group (P<0.0001). P53 staining was also noted in the epithelium adjacent to the tumor in 14.7% (5/34) cases.
PCNA showed intense nuclear staining in 20-30% cells in all cases of infiltrating BCC. In contrast, the expression was restricted to the periphery of the tumor nests in 5-20% nuclei of the noninfiltrating cases [[Figure - 2]c]. The proliferative activity was significantly higher in infiltrating BCC (P<0.0001).
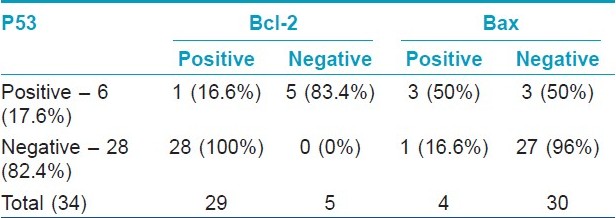
Bcl-2 expression was seen in 85.3% (29/34; [[Figure - 2]d]). All except one of these were negative for p53. There was a statistically significant inverse relationship between the expression of p53 and Bcl-2 (P<0.00002; [Table - 2]). Weak focal expression of Bax was noted in 11.8% (4/34) of cases.
About 20% of BCCs in black patients are reported to develop in less exposed areas. [5] However, the age incidence and distribution of tumors in the present study is comparable to that in the Western literature. Only 9% of the tumors were found in nonexposed sites suggesting an active role of UV radiation as in the Western population. It was noted that BCC in patients with dark skin presents at an advanced stage due to difficulty in the detection of telangiectasias and pearly tumor borders. One striking feature was the high frequency of pigmented tumors found in colored skin (44.2%) as against an average of 5% in the Caucasian population. The pigmentation was a frequent cause of misdiagnosis of these lesions as seborrheic keratoses, malignant melanoma, or nevus sebaceus.
The incidence of p53 gene mutations in the present study (17.6%) is low relative to most studies in the Western literature. There was a strong association between p53 expression and infiltrative BCC as found by the Chi-square test. P53 staining noted in the epithelium adjoining the tumor could possibly represent an early stage of carcinogenesis or lateral spread of the tumor cells outside the clinical borders of the neoplasm. P53 showed a higher expression in elderly patients with longer duration of sun exposure and could be an early event in tumorigenesis.
Being an antiapoptotic gene, Bcl-2 promotes cell survival even in the absence of a high rate of cell proliferation. Our study supports this observation in that high Bcl-2 was noted in cells with a lower proliferation index. A mutually exclusive pattern of p53 and Bcl-2 expression was noted with a statistically significant negative correlation between the two. Being a proapoptotic protein, the weak focal Bax expression correlated with the diffuse Bcl-2 expression.
We conclude that a higher percentage of pigmented lesions and delayed diagnosis in dark-colored skin is noted in BCC of the Indian population. P53 immunoexpression is low compared to Caucasians and an inverse relationship between p53 and the apoptotic inhibitor, Bcl-2, exists. Although the number of cases in this group is small, screening for the p53 protein may be further evaluated for the prognostic evaluation of these tumors.
| 1. |
Bradford PT. Skin Cancer in Skin of Color. Dermatol Nurs 2009;21:170-8.
[Google Scholar]
|
| 2. |
Budhraja SN, Pillai VC, Periyanayagam WJ, Kaushik SP, Bedi BM. Malignant neoplasms of the skin in Pondicherry (a study of 102 cases). Indian J Cancer 1972;9:284-95.
[Google Scholar]
|
| 3. |
Paymaster JC, Talwalkar GV, Gangadharan P. Carcinomas and malignant melanomas of the skin in Western India. J R Coll Surg Edinb 1971;16:166-73.
[Google Scholar]
|
| 4. |
Deo SV, Hazarika S, Shukla NK, Kumar S, Kar M, Samaiya A. Surgical management of skin cancers: Experience from a regional cancer centre in North India. Indian J Cancer 2005;42:145-50.
[Google Scholar]
|
| 5. |
Mora RG, Burris R. Cancer of the skin in African Americans: A review of 128 patients with basal cell cancer. Cancer 1981;47:1436-8.
[Google Scholar]
|
Fulltext Views
4,776
PDF downloads
2,532





