Translate this page into:
Basidiobolomycosis mistaken for cutaneous tuberculosis
2 Department of Microbiology, Venereology and Leprosy, Kasturba Medical College, Manipal University, Manipal, Karnataka, India
3 Department of Pathology, Venereology and Leprosy, Kasturba Medical College, Manipal University, Manipal, Karnataka, India
Correspondence Address:
Gnana Kireeti Gummadi
Department of Dermatology, Venereology and Leprosy, Kasturba Medical College, Manipal University, Manipal, Karnataka
India
| How to cite this article: Gummadi GK, Pai B S, Nayak U K, Prakash P Y, Pai K. Basidiobolomycosis mistaken for cutaneous tuberculosis. Indian J Dermatol Venereol Leprol 2019;85:236 |
Sir,
A 44-year-old immunocompetent male patient presented to the department of dermatology, Kasturba Medical College, Manipal, with itching and progressive hardening and pigmentation of the right thigh since 8 months. The lesion started initially as a firm swelling over the upper, medial aspect of the right thigh. He was seen initially at another hospital, where excision biopsy was done, and subsequently treated with 6 months of anti-tubercular therapy; as his histopathology report was suggestive of cutaneous tuberculosis. He reported subsequent increase in size of the lesion on treatment, and when he presented to us, a large indurated plaque was present over the right thigh extending up to the right side of the scrotum and finally reaching the mid-inguinal point [Figure - 1]. Insinuation sign was positive. Differential diagnoses of deep fungal infection and cutaneous tuberculosis (lupus vulgaris and scrofuloderma) were considered. An incisional biopsy was done, and the tissue was sent for both histopathology and fungal culture. Histopathological examination showed dermal and subcutis granulomatous infiltration with Langhans and multinucleated giant cells, lymphocytes, plasma cells, and eosinophils along with dense fibrosis [Figure - 2] and [Figure - 3]. Periodic Acid-Schiff [Figure - 4] and silver staining [Figure - 5] showed few fungal elements. Culture identified the fungus as Basidiobolus ranarum [Figure - 6] and [Figure - 7]. In view of financial constraints, itraconazole could not be started. The patient was treated with oral super-saturated solution of potassium iodide starting at five drops thrice daily which was increased by one drop daily to a maximum of forty drops per day. Monthly follow up showed a progressive reduction in size of the plaque with complete recovery seen after 5 months of therapy.
 |
| Figure 1: Indurated plaque was present over right thigh extending up to right side of scrotum and pubis crossing the inguinal ligament |
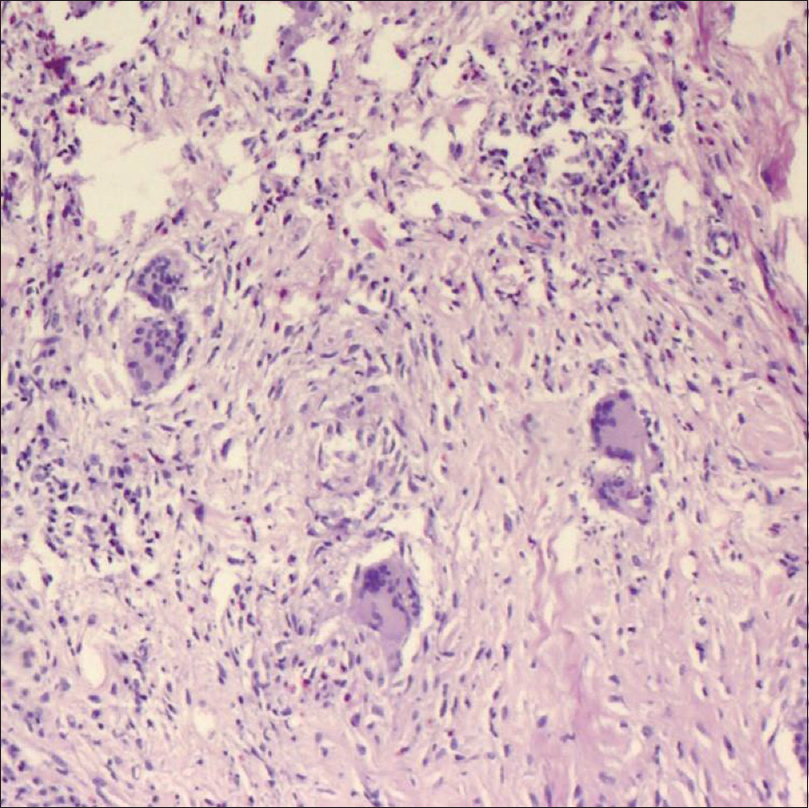 |
| Figure 2: Ill-formed granulomas and numerous foreign body giant cells, Langhans giant cells, eosinophils, lymphocytes, and plasma cells (H and E, ×100) |
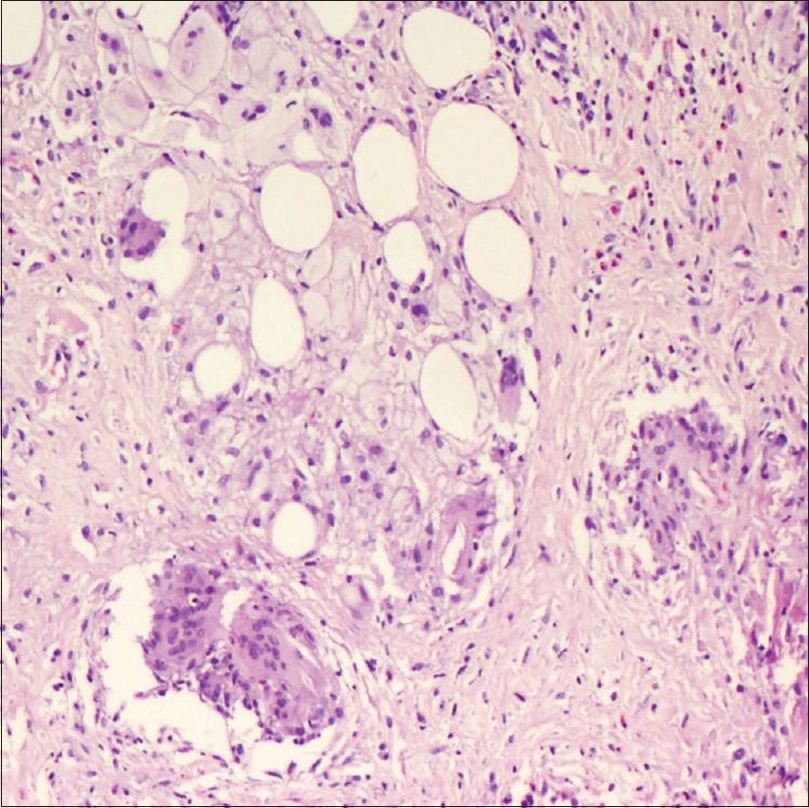 |
| Figure 3: Subcutaneous fat replaced by fibrous tissue (H and E, ×100) |
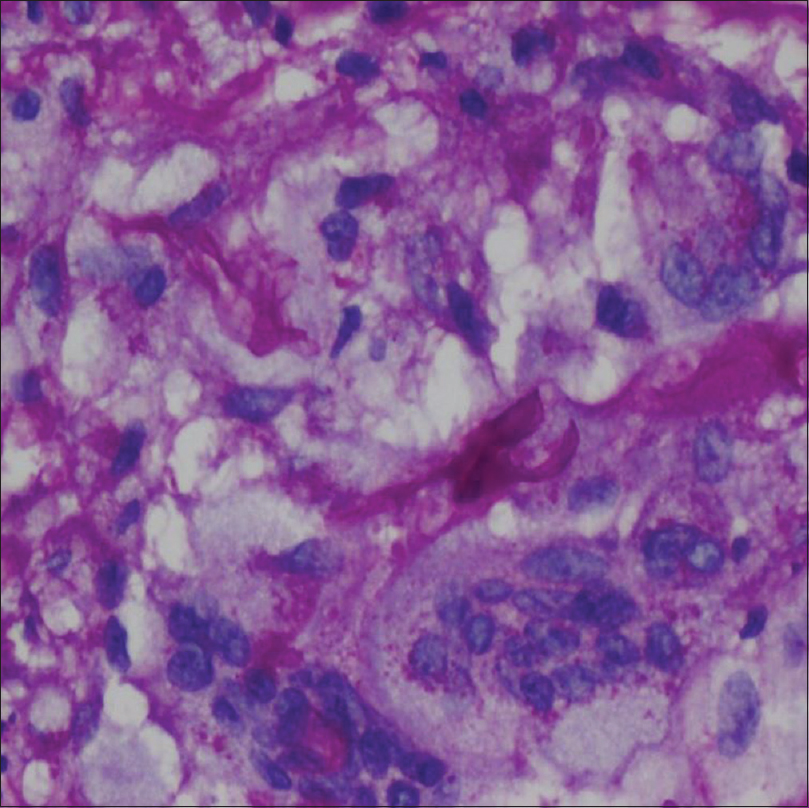 |
| Figure 4: Periodic acid Schiff stain showing broad irregular fungal hyphae with thick walls |
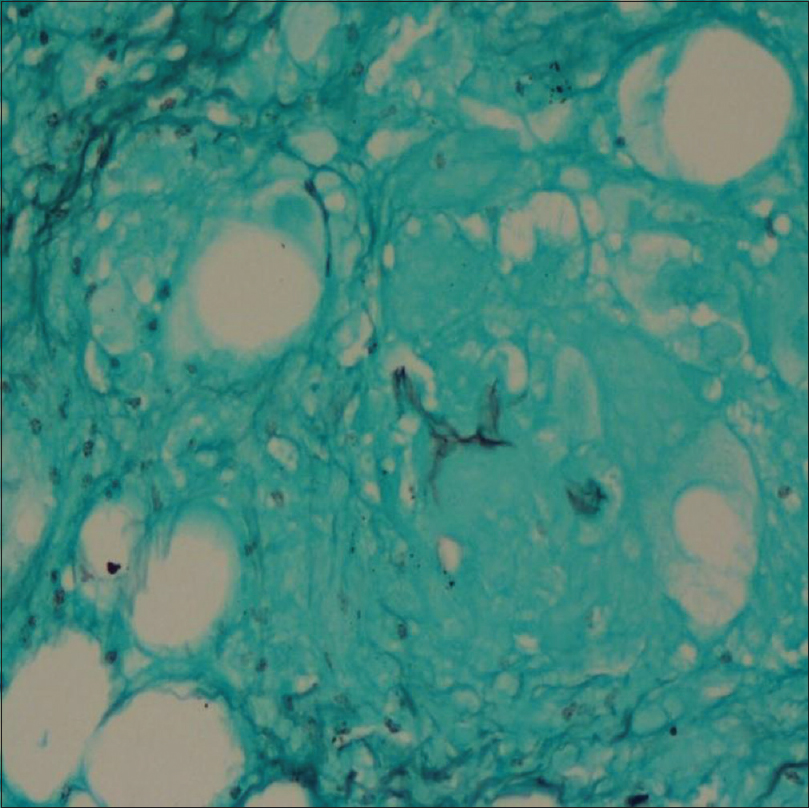 |
| Figure 5: Silver stain showing fungal elements within granuloma |
 |
| Figure 6: A 7-day-old culture grown on Sabourauds Dextrose Agar at 28°C showing raised, cerebriform, radiating, glabrous colonies with pale to tan obverse and no characteristic reverse pigmentation |
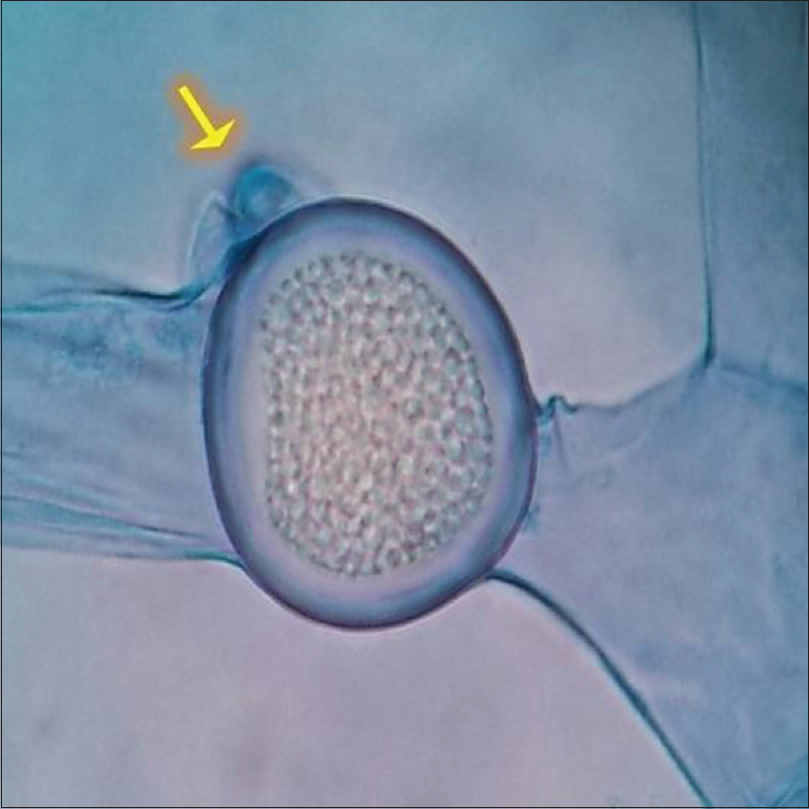 |
| Figure 7: Lactophenol cotton blue mount preparation showing characteristic broad, sparsely septate, hyaline, filamentous hyphae with thick walled, sub hyaline, intercalary zygospores having prominent beak like projection (×400) |
Basidiobolomycosis, a chronic deep fungal infection, is characterized by woody induration of the subcutaneous tissue. This is commonly seen in children (80%) as compared to conidiobolomycosis, which is seen more in adults.[1] The mode of transmission is not exactly known, though minor trauma and insect bites have been reported prior to the onset of the lesions. Clinically, it is characterized by a firm, well-circumscribed and painless swelling, which may involve the whole shoulder, arm, entire leg, or buttocks. It may have a smooth, rounded edge where the fingers can be insinuated underneath and the swelling lifted off the underlying tissues, the insinuation sign.[2] The overlying skin may be normal, pigmented, scaly, and edematous. Ulceration and regional lymphadenopathy are rare.[1] Deeper extension into muscle and viscera are possible complications.[3] Visceral basidiobolomycosis requires a high degree of clinical suspicion to make the diagnosis. The symptoms are vague and the diagnosis is based on histopathological findings of fungal elements and culture of B. ranarum from tissue specimen.
The combination of surgical resection of infected tissue and prolonged itraconazole/posaconazole therapy is preferred. Surgical procedures often lead to the spread of lesion, a feature noticed in our patient.[4]
While trauma and insect bites are proposed as etiological factors, surgical procedures like biopsy and excision tend to cause progression of lesions.[4] Clinically, it has to be differentiated from conditions like lupus vulgaris and scrofuloderma. Lupus vulgaris has varied presentations. The most common presentation is that of a nodule developing into a plaque. Gradually, it becomes infiltrated and progresses relentlessly, but insinuation sign will be absent. In India, thigh, the site of involvement in our case, is one of the common sites of occurrence for lupus vulgaris. Scrofuloderma can also be considered in the initial stages but late lesions will show sinus or ulcer formation.
Diagnosis often requires both histopathology and fungal culture. Histopathology often shows dermal and sub-cuticular granulomatous mixed infiltrate with eosinophils, lymphocytes, plasma cells, giant cells, histiocytes and neutrophils with Splendore–Hoeppli-like phenomenon and fibrosis.[3],[5] Special stains such as PAS and Gomori–Grocott are often required for identifying fungal elements.[3] Culture is required to identify the fungus.
Itraconazole is the drug of choice in the treatment of basidiobolomycosis. Prolonged therapy is needed and can be given in a dose of 200 mg twice daily for 4–6 months. Other antifungals such as amphotericin B, terbinafine, ketoconazole, and fluconazole have also been successfully tried.[3] Oral potassium iodide has also been favored in the treatment of this condition.[1],[3] Our patient was treated with oral supersaturated solution of potassium iodide. The lesions resolved completely after 5 months of therapy and he did not suffer from any side effects.
This case report is presented to highlight the following notable points. The patient had an older age of onset, compared to the usual age groups affected. Basidiobolomycosis was mistaken for cutaneous tuberculosis and treated erroneously. Thus, it is necessary to perform biopsy for histopathology and culture to confirm the diagnosis, prior to the commencement of therapy. Revision of diagnosis needs to be considered when the patient is not responding to anti-tubercular therapy. Potassium iodide is an economical and effective option in the management of basidiobolomycosis, especially in India with patients having financial constraints.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hay RJ, Ashbee HR. Fungal infection In: Griffiths CE, Barker J, Bleiker T, Chalmers R, Creamer D, editors. Rook's Textbook of Dermatology. Vol. 32. 9th ed. Singapore: Wiley Blackwell; 2016. p. 80-1.
[Google Scholar]
|
| 2. |
Arora P, Sardana K, Bansal S, Garg VK, Rao S. Entomophthoromycosis (basidiobolomycosis) presenting with “saxophone” penis and responding to potassium iodide. Indian J Dermatol Venereol Leprol 2015;81:616-8.
[Google Scholar]
|
| 3. |
Ramesh V, Seshadri D, Ramam M, Habib ST. Deep fungal infections. In: Sacchidanand S, editor. IADVL Textbook of Dermatology. 4th ed. Mumbai: Bhalani Publishing House; 2015. p. 534-8.
[Google Scholar]
|
| 4. |
Prasad PV, Paul EK, George RV, Ambujam S, Viswanthan P. Subcutaneous phycomycosis in a child. Indian J Dermatol Venereol Leprol 2002;68:303-4.
[Google Scholar]
|
| 5. |
Weedon D. Mycoses and algal infection. In: Weedon D editor. Skin Pathology. 2nd ed. China: Churchill Livingstone; 2002. p. 678.
[Google Scholar]
|
Fulltext Views
3,298
PDF downloads
2,182





