Translate this page into:
Bilateral madarosis due to papular mucinosis
2 Department of Dermatology, Venkat Charmalaya, Institute for Advanced Dermatology and Postgraduate Training, Bangalore, Karnataka, India
Correspondence Address:
Vani Vasanth
19, 'Skanda', Rajahamsa Road, Ittamadu, BSK 3rd Stage, Bangalore - 560 085, Karnataka
India
| How to cite this article: Vasanth V, Shivanna CB, Mysore V. Bilateral madarosis due to papular mucinosis . Indian J Dermatol Venereol Leprol 2014;80:458-459 |
Sir,
Madarosis is a window to diagnosis for several diseases. Usually, the patient with madarosis consults a dermatologist for cosmetic reasons. Thorough investigation is warranted to arrive at an accurate diagnosis of the underlying condition. We report a patient with papular mucinosis who presented to us with bilateral madarosis as the only complaint.
A 46-year-old woman reported with the chief complaint of loss of eyebrows. She had first noticed diffuse thinning of her eyebrows about 10 years ago that had gradually progressed to complete loss. There was no history of itching, redness, or eruptions at the site. There was no history of patchy loss of eyebrows or loss of hair from any other body area. She had no systemic complaints and sought consultation for cosmetic reasons.
On examination, there was diffuse loss of hair from the eyebrows with no associated erythema [Figure - 1]a. Facial skin was thickened and hard to pinch. Tiny, yellowish to skin-colored papules were scattered all over the face; these were more closely set on the forehead [Figure - 1]b. The helices were involved bilaterally, whereas the neck was spared. The patient had not noticed these skin lesions earlier. There were no similar lesions elsewhere on the body. There was no thickening of skin over the shins and the patient was not overweight.
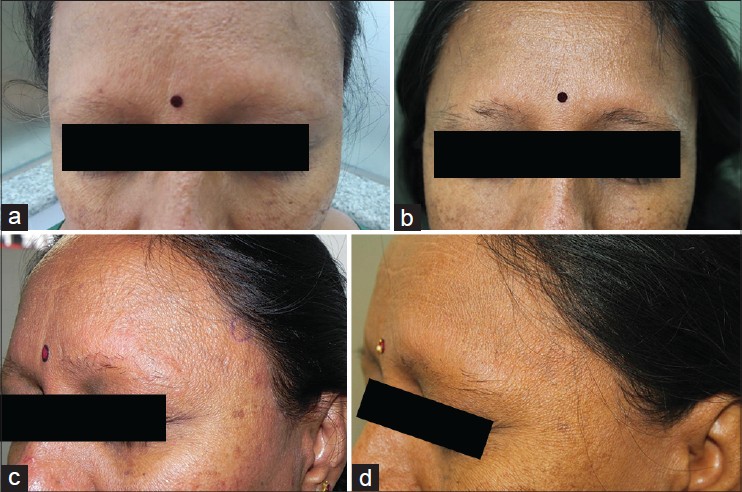 |
| Figure 1: (a) Diffuse loss of bilateral eyebrows with thickening of facial skin (b) Multiple yellowish to skin colored papules with thickening of skin seen over the forehead (c) Re-growth of eyebrow hair following three months of treatment (d) Resolution of papules following three months of treatment |
A provisional diagnosis of localized mucinosis was made. Complete blood counts, peripheral smear, liver function test, thyroid function test, fasting lipid profile, fasting and post-prandial blood glucose were all within normal limits.
Histopathology showed epidermal hyperkeratosis and follicular plugging. The papillary and upper reticular dermis showed deposits of homogenous pinkish material. There was a perifollicular lymphocytic infiltrate [Figure - 2]a. PAS and Congo Red stains were negative, while Alcian blue staining was positive [Figure - 2]b and revealed mucin deposition in the upper and mid dermis confirming the diagnosis of localized papular mucinosis.
The patient was treated with oral isotretinoin 20 mg/day along with topical retinoic acid and a sunscreen. Following this, she showed good improvement with regrowth of eyebrow hair in about three months along with disappearance of the waxy papules and regression of facial thickening[Figure - 1]c and d. Later, the patient was non-compliant with medication because of which there was a recurrence of eyebrow loss though there was no thickening of skin or papules. She has been re-started on oral isotretinoin.
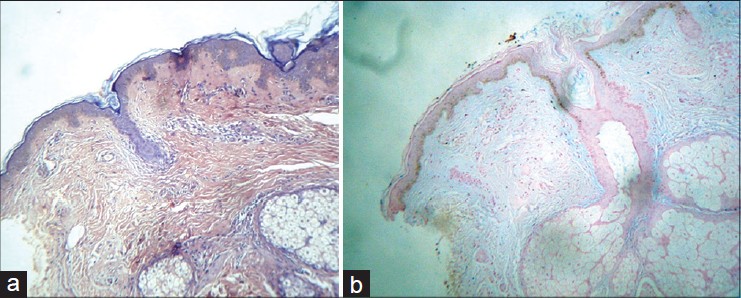 |
| Figure 2: (a) H and E, stain showing pinkish mucin deposits in the upper and mid-dermis with clefts (b) Alcian blue staining showing mucin deposits in the upper and mid-dermis |
The term madarosis is derived from the Greek word " madaros" meaning "pulpy or bald." Ciliary madarosis refers to loss of eyelashes while superciliary madarosis refers to loss of eyebrows. Madarosis can be either scarring or non-scarring. Some of the common causes of madarosis include infections like staphylococccal blepharitis and leprosy, endocrine disorders like hypothyroidism, drugs, auto-immune conditions like alopecia areata and trauma. [1]
Papular mucinosis is an idiopathic, cutaneous condition. The term papular mucinosis has been used synonymously with lichen myxedematosus and scleromyxedema, but as a general rule, scleromyxedema refers to a generalized distribution of lesions. [2] Papular mucinosis affects both sexes equally and commonly occurs beyond 30 years of age. It manifests with asymptomatic waxy, flat-topped, confluent, skin-colored papules. The commonest sites involved in localized papular mucinosis are the acral areas: dorsal aspect of hands, feet, elbows and face, ears, and neck.
Serum electrophoresis may show an abnormal paraprotein of IgG type. Histology shows mucin deposition in between collagen bundles in the upper dermis. There is dermal fibrosis with increase in the number of fibroblasts. The mucinous material is glycosaminoglycan which stains with Alcian blue.
Treatment of this condition remains unsatisfactory. Melphalan is the drug of choice for generalized scleromyxedema. Localized lichen myxedematosus has been treated with tacrolimus ointment. Systemic steroids alone may be ineffective. [3] Both isotretinoin [4] and etretinate have been associated with improvement. Other options include cyclophosphamide alone or in combination with prednisone, interferon-alpha, cyclosporine, PUVA photochemotherapy, electron- beam therapy, and IVIg. [5]
The management of madarosis requires identification and treatment of the underlying condition. Though rare, papular mucinosis should be considered in the differential diagnosis of madarosis. It causes non-scarring type of madarosis and as seen in our case, hair regrowth does occur with treatment of the disease.
| 1. |
Sachdeva S, Prasher P. Madarosis: A dermatological marker. Indian J Dermatol Venereol Leprol 2008;74: 74-6.
[Google Scholar]
|
| 2. |
Rongioletti F, Rebora A. Updated classification of papularmucinosis, lichen myxedematosus, and scleromyxedema. J Am Acad Dermatol 2001;44:273-81.
[Google Scholar]
|
| 3. |
Sarkany RP, Breathnach SM, Morris AA. Metabolic and nutritional disorders. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology, 8 th ed. Oxford: Wiley-Blackwell; 2010. p. 59.21-3.
th ed. Oxford: Wiley-Blackwell; 2010. p. 59.21-3.'>[Google Scholar]
|
| 4. |
Hisler BM, Savoy LB, Hashimoto K. Improvement of scleromyxedema associated with Isotretinoin therapy. J Am Acad Dermatol 1991;24:854-7.
[Google Scholar]
|
| 5. |
Rothfleisch JE. Papularmucinosis. Dermatol Online J 2001;7:13.
[Google Scholar]
|
Fulltext Views
3,684
PDF downloads
2,090





