Translate this page into:
Bipolar aphthosis presenting as mutilating genital ulcers in women
2 Department of Obstetrics and Gynecology, PGIMER, Chandigarh, India
Correspondence Address:
Bhushan Kumar
Dept. of Dermatology, Venereology and Leprology, PGIMER, Chandigarh - 12
India
| How to cite this article: Gupta S, Ajith C, Malhotra S, Kumar B. Bipolar aphthosis presenting as mutilating genital ulcers in women. Indian J Dermatol Venereol Leprol 2004;70:357-360 |
Abstract
Three women with large, mutilating genital ulcers of long duration, destroying almost the lower half of the external genitalia, are reported. They had a history of recurrent oral ulcers as well. All patients had been diagnosed as having 'genital ulcer syndrome' in the past and had been treated with antimicrobials. Histopathology of the biopsy from the margin of the ulcer revealed features of leukocytoclastic vasculitis. Considering the history, clinical features and histology, a diagnosis of bipolar aphthosis was made in all patients. All patients responded well to immunosuppressive therapy. The cases are reported because of the presence of genital ulcers of an unusually large size, mutilating character and their close similarity to genital ulcers due to sexually transmitted diseases, especially genital herpes and donovanosis. |
 |
 |
 |
 |
 |
INTRODUCTION
Aphthae are localized, painful, shallow, round to oval ulcers often covered by a gray fibro-membranous slough and surrounded by an erythematous halo. Complex aphthosis involves almost constant, multiple ( 3), oral or oral and genital aphthae.[1] Those involving both oral and genital aphthae are termed as bipolar aphthosis (BA) of Neumann. Most specialists consider bipolar aphthosis to be a forme fruste of Behçet′s disease (BD).[1],[2],[3] The prevalence of genital aphthae in BD varies from 60% to 90% in various reports.
Genital aphthae are most commonly seen in male patients on the scrotum and in female patients on the vulva. In females, genital aphthae tend to be larger and deeper, sometimes even leading to perforations.[4] Genital aphthae, especially those which are larger, may be confused with sexually transmitted diseases (STDs); a common misdiagnosis is genital herpes or donovanosis. We report 3 female patients of bipolar aphthosis (BA) with large mutilating genital ulcerations who were misdiagnosed as having STDs.
CASE REPORTS
Case 1: A 26-year-old married woman presented with a single large painful vulval ulcer of 10 months′ duration. It had initially started as a painful pustule near the introitus, which ulcerated one week later and gradually enlarged to erode and mutilate the lower half of the vulva. She was diagnosed as a case of genital ulcer syndrome and was treated with a combination of antimicrobials, but with no improvement. Later, a surgeon attempted excision with primary closure. One week after excision, an indolent ulcer developed in the closure line, leading to gaping of the wound. The patient gave a history of recurrent oral and genital ulcerations 3 times during the past 10 years, which had healed spontaneously in variable periods of time. There were periods of complete remission ranging from 1-4 years.
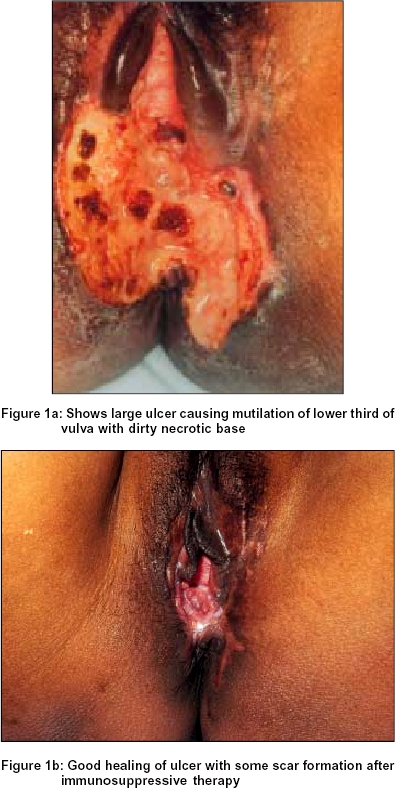
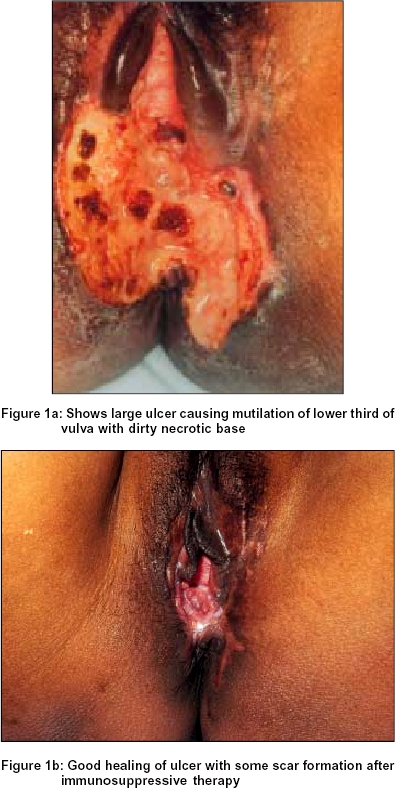
Examination revealed a well-defined deep ulcer 4x4 cm in size with blackish, irregular, indurated margins and an unhealthy necrotic base. The ulcer had eroded almost half of the vulva and a part of the perineum [Figure - 1]a. The base was non-friable. There was no regional lymphadenopathy.
The patient was treated initially with oral prednisolone 40 mg daily, but since the response was very slow azathioprine 100 mg daily and colchicine 1.5 mg daily were added. This resulted in complete healing with scar formation in about 4 months [Figure - 1]b.
Case 2: A 23-year-old married woman presented with a large painful ulcer on the lower half of her external genitalia for the last 8 months. She had a history of recurrent oral and genital ulcers 1-2 cm in size about 3-4 times during the past 4-5 years, which healed with or without treatment in 2-3 weeks. In the present episode, she developed a small papule on the lower half of the vulva, which ulcerated and gradually destroyed the lower half of the vulva. She had been diagnosed as having a genital ulcer due to sexually transmitted pathogen(s) and had been treated with various antimicrobials. However the ulcer gradually increased in size.
Examination revealed a large ulcer 4x1 cm in size with a necrotic base and a foul smelling discharge [Figure - 2]. It had tender, indurated edges and had eroded almost half of the vulva. Inguinal lymphadenopathy, with discrete, firm, nontender lymph nodes, was present.
The patient was treated orally with colchicine 1.5 mg daily and prednisolone 20 mg daily. The lesion healed completely with some scarring in about 10 weeks. The drugs were tapered off over about 6 months.
Case 3: A 31-year-old married woman presented with a single large ulcer on the external genitalia for the last 6 months. It had started as a tiny ulcer on the lower pole of the vulva and had gradually enlarged to involve almost half of the genitalia and perineum. She had a history of small, recurrent, oral and genital ulcers that tended to heal spontaneously in 1-3 weeks.
Examination revealed a large ulcer 5 x 4 cm in size on the lower half of the vulva and perineum [Figure - 3]. It was covered with dirty, necrotic debris and a foul smelling discharge. The edges were indurated and the ulcer was extremely tender. Inguinal lymphadenopathy, with discrete, firm, tender lymph nodes, was present.
The patient was treated with oral prednisolone 40 mg daily and colchicine 1.5 mg daily, which resulted in complete healing of the ulcer in about 12 weeks. The drugs were tapered off slowly and there were no recurrences over the next 2 months of follow-up.
All patients denied any extramarital sexual contact. There was no history of any disease in the husband in any of the patients. There was no history of vaginal or urethral discharge, skin rash, and joint pain or eye symptoms in any of the patients. Systemic examination, including ophthalmologic check up, was within normal limits.
The hemoglobin, total and differential counts, peripheral smear, blood biochemistry, urine examination, and chest X-ray were normal in all the 3 patients. VDRL and HIV serology were negative in all. Gram stained smears from the ulcer revealed pus cells and gram-positive cocci in the first 2 patients, and gram-positive cocci and gram-negative bacilli in the third patient. Pus culture did not reveal growth of any significance. Tissue smears for Donovan bodies were also negative. The pathergy test was negative in all the patients. Biopsy revealed features of secondary leukocytoclastic vasculitis and vascular thrombosis in all patients. The second patient, in addition, had a significant lymphocytic infiltrate. Based on the history, clinical features and histopathology, a diagnosis of bipolar aphthosis (BA) was made in all the patients.
DISCUSSION
The nosologic field of aphthosis is not well defined.[4] Recurrent aphthae is the most common cause of ulceration of the oral mucosa.[5] Similar ulcers on the genitalia are rare. Unusually patients with genital aphthae have a history of oral aphthae as well, but lesions on these two sites do not necessarily occur concomitantly. Complex aphthosis is a disorder in which patients develop recurrent oral and genital aphthous ulcers (bipolar aphthosis; BA) or almost constant, multiple oral aphthae (unipolar aphthosis), without manifestations of systemic disease. Behçet′s disease (BD) is a multisystem disease characterized clinically by oral and genital aphthae, arthritis, cutaneous lesions, and ocular, gastrointestinal, and neurological manifestations.[1] Patients with BA do not fulfill the criteria for BD. However, comparative studies have shown that there are similarities in the characteristics of aphthae (number, localization, recurrences and presence of scars) in patients of BA and BD, supporting the hypothesis of a continuous spectrum linking severe aphthosis to BD.[3] These evidences suggest that BA is a forme fruste of BD.[1],[2],[3] Bipolar aphthosis is thought to occur almost exclusively in women, although exact epidemiological data is not available. There are reports of genital aphthae being more common in female BD patients.[4] Since ulcers in BA and BD are characteristically located on the external genitalia, many of these patients self-refer to Genitourinary Medicine/STD clinics.
Genital ulcers of BA may closely mimic genital herpes, both in morphology and in their tendency to recur. The size of genital ulcers in patients with BA is usually less than 1-2 cm. In women, these ulcers rarely erode the deeper tissue and, when located in the vagina, may lead to urinary/fecal fistula formation.[6] The genital aphthae of BA usually heal with scarring, more so in women.
We report 3 women with BA who presented with unusually large, destructive genital ulcers. All our patients had a striking similarity in the course of the disease, morphology of the lesions and complete response to immunosuppressive treatment. The lesions were located on the lower one-third to half of the vulva in all patients. To the best of our knowledge such a predilection of site and mutilation of this extent of the external genitalia due to genital aphthae has not been reported.
| 1. |
Ghate JV, Jorizzo JL. Beh�et's disease and complex aphthosis. J Am Acad Dermatol 1999;40:1-20.
[Google Scholar]
|
| 2. |
Boyvat A, Ekmekci P, Gurgey E. Bipolar aphthosis. A forme fruste of Behcet's disease. Long term follow-up of 26 cases. Adv Exp Med Biol 2003;528:321-2.
[Google Scholar]
|
| 3. |
Verpilleux MP, Bastugi-Garin S, Revuz J. Comparative analysis of severe aphthosis and Beh�et's disease: 104 cases. Dermatology 1999;198:247-51.
[Google Scholar]
|
| 4. |
Tursen U, Gurler A, Boyvat A. Evaluation of clinical findings according to sex in 2313 Turkish patients with Beh�et's disease. Int J Dermatol 2003;42:346-51.
[Google Scholar]
|
| 5. |
Rogers RS 3rd. Recurrent Aphthous Stomatitis: Clinical characteristics and associated systemic disorders. Semin Cutan Med Surg 1997;16:278-83.
[Google Scholar]
|
| 6. |
Kontogiannis V, Powell RJ. Beh inverted question market's disease. Postgrad Med J 2000;76:629-37.
[Google Scholar]
|
Fulltext Views
4,196
PDF downloads
1,306





