Translate this page into:
Black dot tinea capitis caused by trichophyton rubrum in an adult female presenting with cicatricial alopecia
2 Department of Dermatology, Maulana Azad Medical College, New Delhi, India
3 Department of Pathology, Maulana Azad Medical College, New Delhi, India
4 Department of Microbiology, Jawarhar Lal Nehru Institute of Medical Science, Porompat, Imphal East, Manipur, India
Correspondence Address:
Chitralekha Keisham
Keishamthong Thangjam Leirak, Imphal West - 795 001, Manipur
India
| How to cite this article: Keisham C, Sarkar R, Khurana N, Ghosh N, Garg VK, Manoj RK. Black dot tinea capitis caused by trichophyton rubrum in an adult female presenting with cicatricial alopecia. Indian J Dermatol Venereol Leprol 2015;81:224 |
Sir,
A 20-year-old housewife presented to us with complaints of itching and gradual loss of hair over the scalp for the past 2 years. She was taking multiple treatments from private practitioners but without much relief. On examination, there were multiple patches of hair loss over the scalp along with areas of gray scales and black dots. There was an area of alopecia with loss of hair follicles of size 3 × 12 cm present over the vertex with black dots at the periphery [Figure - 1]. The hairs at the periphery were dull, matted, and easily pluckable. She also had multiple nits along the hair shaft. There was no regional lymphadenopathy. She did not have any systemic disease and was not receiving immunosuppressive drugs. The test done to rule out human immunodeficiency virus(HIV) infection was also normal. Potassium hydroxide mount of the hair shaft showed spores in an endothrix pattern. The scalp biopsy showed numerous rounded PAS positive spores within hair shafts in the follicle along with focal perifollicular fibrosis associated with mild chronic inflammation and spongiosis [Figure - 2]. A diagnosis of black dot tinea capitis presenting with cicatricial alopecia was made. The fungal culture was contaminated with Alternaria species. The patient was treated with oral griseofulvin, 250 mg twice a day along with a ketoconazole and salicylic acid combination shampoo. She was also given ivermectin weekly for 3 weeks along with oral 1% permethrin scalp lotion weekly for pediculosis capitis. After 3 weeks, the patient stopped treatment on her own and presented to us after another 2 weeks. At that time, there was some improvement in the itching, pain, and scaling. All the black dots had disappeared [Figure - 3]. Although she was re-started on griseofulvin, she stopped treatment on her own again after taking treatment for 2 months. She then became symptomatic again. A fungal culture was re-sent and revealed growth of Trichophyton rubrum on this occasion. The culture on Sabouraud agar showed white, heaped, velvety colonies with red pigmentation on the reverse side after 3 weeks. Microscopically, clavate microconidia, without macroconidia were noted along the hyphae. Due to her poor compliance with treatment and persistence of disease, she was advised terbinafine, 250 mg once daily along with ketoconazole shampoo for 1 month, that was continued for another month on account of persisting lesions. A repeat culture sent at the end of 2 months of this treatment was negative. She was advised to follow up monthly to assess for recurrence or re-infection. The patient was, however, lost to follow up.
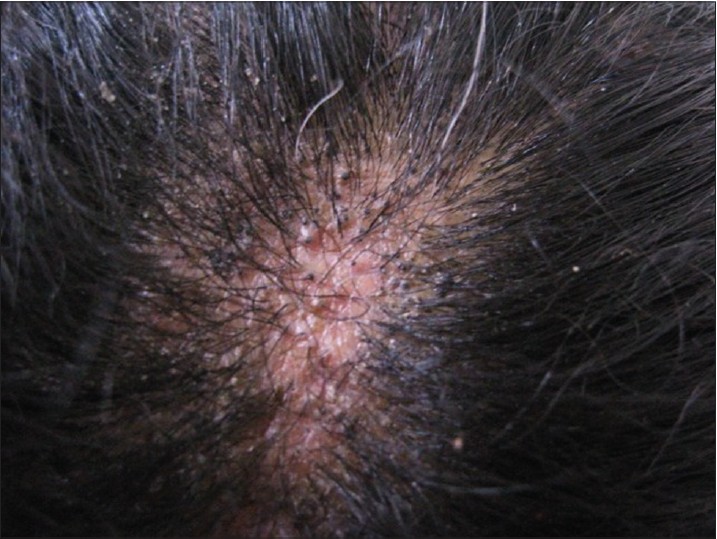 |
| Figure 1: Areas of cicatricial alopecia with gray scales and black dots at the periphery |
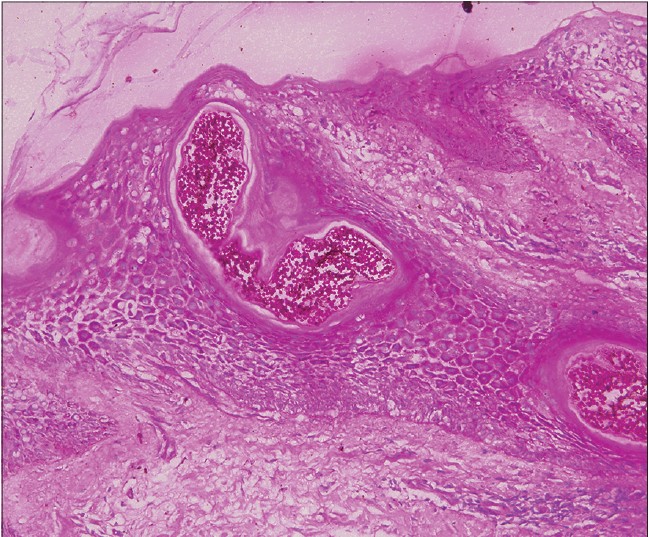 |
| Figure 2: PAS positive spores within the hair shaft (Perodic Acid Schiff Stain, ×400) |
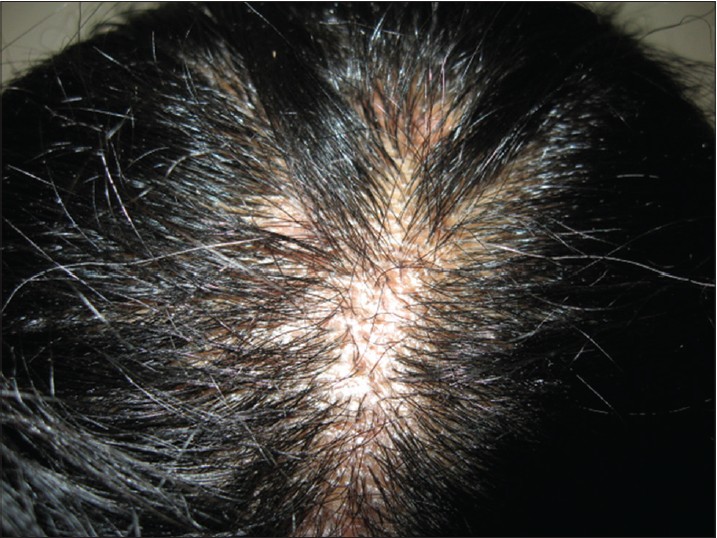 |
| Figure 3: Improvement in scaling, matting with disappearance of black dots after oral antifungal therapy |
Tinea capitis is a disease of children but 3-11% of cases occurs in adults , especially in the elderly and female population. [1],[2] The most frequently isolated organism in adults is Trichophyton tonsurans and endothrix organisms belonging to anthropophilic group of dermatophytes. [3],[4] Trichophyton rubrum causes tinea capitis in less than 1% of the cases in children as compared to over 10% in adults. [5] Though black dot tinea capitis caused by Trichophyton rubrum is reported, the association of such a case with cicatricial alopecia has not been reported. [6] The presence of cicatricial alopecia in our patient could be explained by the ability of Trichophyton rubrum to cause inflammatory patterns of tinea capitis like folliculitis or kerion.This might have occurred in our patient, during the course of the chronic illness, but was not seen at the time of presentation. Another explanation for cicatricial alopecia is the presence of secondary infection. Although pediculosis can be complicated by secondary infection, the history and clinical features were not suggestive of it. Tinea capitis in adults usually occurs in people with contributory factors like atopy or collagen vascular disease or immunosuppresion. But there were no such contributory factors in our patient. The presence of Alternaria in the culture could be explained by the fact that it is a common airborne contaminant in the laboratory. We did not suspect it to be the primary cause of infection due to the excellent clinical response to griseofulvin.The histopathological features were not supportive of a dermal or subcutaneous infection due to Alternaria causing the scarring alopecia.
The long duration of illness in our patient could be explained by the lack of compliance and the chronic nature of disease caused by Trichophyton species. [7] A carrier in the household, usually a child, can also be a source of reinfection. Trichophyton species are more responsive to terbinafine than griseofulvin as seen in certain studies, [8],[9] and the same was observed in our patient.
| 1. |
Cremer G, Bournerias I, Vandemeleubroucke E, Houin R, Revuz J. Tinea capitis in adults: Misdiagnosis or reappearance? Dermatology 1997;194:8-11.
[Google Scholar]
|
| 2. |
Ginter-Hanselmayer G, Weger W, Ilkit M, Smolle J. Epidemiology of tinea capitis in Europe: Current state and changing patterns. Mycoses 2007;50 Suppl 2:6-13.
[Google Scholar]
|
| 3. |
Ooka S, Kashima M, Kubota Y, Noguchi A, Kawai S, Nakamura Y, et al. A case of black dot ringworm with a review of Japanese cases. J Dermatol 2000;27:658-63.
[Google Scholar]
|
| 4. |
Jha BN, Garg VK, Agrawal S, Khanal B, Agarwalla A. Tinea capitis in eastern Nepal. Int J Dermatol 2006;45:100-2.
[Google Scholar]
|
| 5. |
Schwinn A, Ebert J, Brocker EB. Frequency of Trichophyton rubrum in tinea capitis. Mycoses 1995;38:1-7.
[Google Scholar]
|
| 6. |
Price VH, Rosenthal SA, Villafane J. Black dot tinea capitis caused by Trichophyton rubrum. Arch Dermatol 1963 Apr; 87:487-8.
[Google Scholar]
|
| 7. |
Dahl MV, Grando SA. Chronic dermatophytosis: What is special about Trichophyton rubrum? Adv Dermatol 1994;9:97-109.
[Google Scholar]
|
| 8. |
Gupta AK, Drummond-Main C. Meta-analysis of randomized, controlled trials comparing particular doses of griseofulvin and terbinafine for the treatment of tinea capitis. Pediatr Dermatol 2013;30:1-6.
[Google Scholar]
|
| 9. |
Mohrenschlager M, Korting HC, Seidl HP, Ring J, Abeck D. Tinea capitis. Therapeutic options in the post-griseofulvin era. Hautarzt 2002;53:788-94.
[Google Scholar]
|
Fulltext Views
8,476
PDF downloads
2,812





