Translate this page into:
Blastomycosis-like pyoderma
Correspondence Address:
Shweta S Sawalka
Department of Dermatology, 4th Floor, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai - 400 022
India
| How to cite this article: Sawalka SS, Phiske MM, Jerajani H R. Blastomycosis-like pyoderma. Indian J Dermatol Venereol Leprol 2007;73:117-119 |
Abstract
A 9-year-old female, presented with recurrent bilaterally symmetrically distributed flesh colored vegetative plaques, papules and nodules on trunk, and upper and lower extremities since 15 days. Investigations revealed anemia, hypoproteinemia, decreased albumin and positive D-xylose test. Pus swab and biopsy for culture sensitivity showed Enterococci species. Biopsy showed spongiotic psoriasiform dermatitis with subcorneal pustule. She fulfilled criteria for the diagnosis of blastomycosis-like pyoderma viz. presentation of large verrucous plaques with pustules and elevated border, pseudoepitheliomatous hyperplasia with abscess histologically and growth of one pathogenic bacterium on culture or tissue biopsy. She responded to long-term amoxicillin-clavulanic acid therapy. |
| Post treatment clearance of lesions |
 |
| Post treatment clearance of lesions |
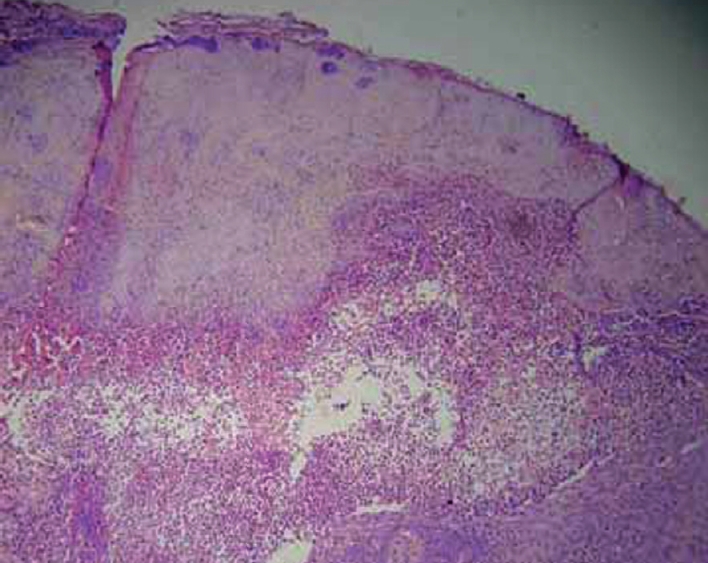 |
| Marked epidermal hyperplasia with intraepidermal blister and areas of spongiosis and mixed infi ltrate in dermis (H and E, x100) |
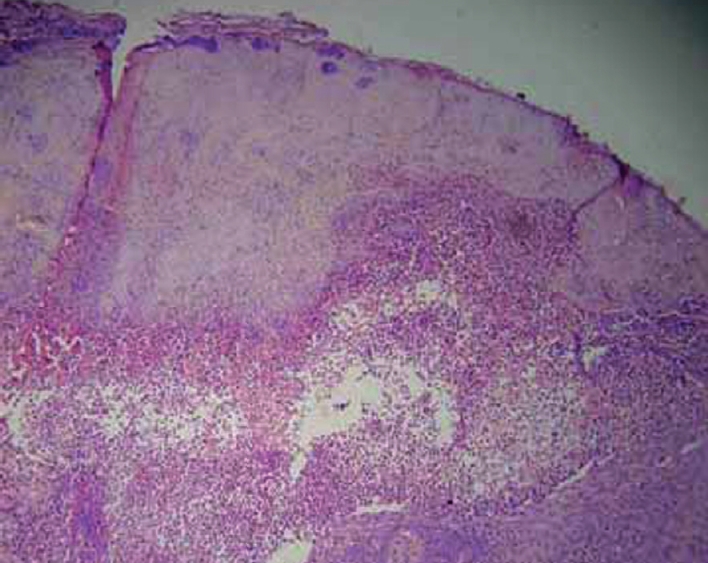 |
| Marked epidermal hyperplasia with intraepidermal blister and areas of spongiosis and mixed infi ltrate in dermis (H and E, x100) |
 |
| Flesh colored plaques with overlying crusting and erosions |
 |
| Flesh colored plaques with overlying crusting and erosions |
 |
| Multiple, fl esh colored papules, pustules and nodules coalescing to form plaques |
 |
| Multiple, fl esh colored papules, pustules and nodules coalescing to form plaques |
INTRODUCTION
Blastomycosis-like pyoderma, a rare condition manifesting as vegetating skin lesions, is an unusual tissue reaction possibly to bacterial infection, commonest organism being Staphylococcus aureus . We present a case of blastomycosis-like pyoderma. The uniqueness of our case is its younger age of presentation, association with malnutrition as proved by D-xylose test and presence of Giardia in stools. This case highlights the need to look for malnutrition as an underlying factor for blastomycosis-like pyoderma in tropical and subtropical countries.
CASE REPORT
A 9-year-old female weighing 21 kg, full term normal delivery, born of consanguineous marriage, with normal developmental milestones and immunization history till date presented with multiple itchy raised lesions on hands, feet and trunk since 15 days. She reported recurrence of similar lesions since one year subsiding with antibiotics. There was no history of trauma, consumption of bromides, tuberculosis or tuberculosis contact. She was 50 th percentile for age, pale and malnourished, with normal vital parameters. There was pitting non-tender edema of the hands and feet with cervical and inguinal lymphadenopathy. The systemic and musculoskeletal examination was normal.
Cutaneous examination revealed multiple, bilaterally symmetrically distributed, flesh colored papules and nodules, coalescing to form fleshy plaques ranging from 1 to 7 cm on the dorsal aspects of hands, feet and wrist [Figure - 1]. Similar lesions, distributed bilaterally asymmetrically were seen on neck, trunk, thighs and knees. Lesions on trunk and feet showed overlying crusting and erosions [Figure - 2].
Laboratory findings showed anemia of 8.5 gm/dl with hypochromasia, microcytosis and anisocytosis, reversal of albumin/globulin ratio (A/G ratio- 1.7/1.6), hypoproteinemia and hypocalcemia (6.6 mg%). Blood sugar, serum electrolytes, renal function tests and urine examination were normal. Serum protein electrophoresis showed decreased albumin. ELISA for HIV and serum VDRL were negative. Stool examination revealed cysts and trophozoites of Giardia lamblia . Mantoux test and pathergy test were negative. X-ray chest showed cardiomegaly. Ultrasonography of abdomen was normal. D-xylose test showed decreased excretion (0.98 gm) of xylose over a period of 5 hours (normal range:> 1.2 gm of excretion) confirming malabsorption. Esophagogastroduodenoscopy was normal. Duodenal biopsy revealed duodenitis and papillary atrophy.
Pus swab grew Methicillin resistant Staphylococcus aureus (MRSA), Acinetobacter, Pseudomonas, Enterococci species , but no AFB and fungi were grown. Biopsy from the papule showed a thick scale crust, marked epidermal hyperplasia with intraepidermal blister and spongiosis with perivascular and interstitial eosinophilic, neutrophilic and histocytic infiltrate in the dermis [Figure - 3]. Special stains for AFB and fungi were negative. Tissue biopsy grew Enterococcus species, but no AFB and fungi. Direct immunofluorescence was negative. Prolonged course of antibiotics was given; based on the bacterial sensitivity with remarkable flattening of skin lesions [Figure - 4], return of general well being and no development of new lesions. Clinico-pathologic findings, positive bacterial cultures and negative cultures for AFB and fungi strongly suggested the diagnosis of blastomycosis-like pyoderma though our patient did not meet all criteria for diagnosis as bromide levels could not be done.
DISCUSSION
Various synonyms for this condition are: pseudoepithelioma cutane, pyodermitis chronica vegetans of Azua and pseudoepithelioma of Azua, mycosis-like pyoderma, hyper inflammatory proliferative pyoderma and pyoderma vegetans. [1]
In 1903, Azua and Pons first described this condition under the title of pseudo-epitheliomatous cutane. [2] In 1979 Su et al proposed criteria for the diagnosis. [3] The disease is uncommon in India with case reports from various states. Mohan Singh et al reported a case of 53-year-old male from Himachal Pradesh. Kumar Vijay et al reported seven cases. Dutta TK et al reported a case with chronic myeloid leukemia from Pondicherry.
Blastomycosis-like pyoderma presents as vegetating skin lesions similar to blastomycosis or warty tuberculosis. The commonest organisms implicated are Staphylococcus aureus , b-hemolytic streptococci, Pseudomonas aurigenosa , Proteus mirabilis , E. coli and Candida albicans . [4] Factors like alcoholism and nutritional deficiency lead to impairment of host defenses resulting in the reduction of skin resistance to bacterial invasion. In this setting, minor trauma creates a localized area of lowered resistance and the common skin pathogen become established, provoking hypertrophic tissue response resembling cutaneous blastomycosis. Later, new lesions arise de novo as countless organisms from the primary site swarm over the predisposed skin. [5]
Other causative factors include leukemia, primary immunodeficiency, immunosuppressive therapy, X-ray radiation, diabetes mellitus, alcoholism, malnutrition, obesity etc. Brown CS et al have reported two cases associated with nutritional deficiency. [5] Blastomycosis-like pyoderma associated with malabsorption is not reported. It can also develop in areas of tattoo, foreign body lesions and during halogen therapy. [1],[2],[4],[5] The initial lesion usually begins at the site of trauma and presents as large verrucous plaques with multiple pustules and elevated borders. Histology shows pseudoepitheliomatous hyperplasia and multiple abscesses. [2],[4]
Criteria for blastomycosis like pyoderma proposed by Su Duncan and Perry [2],[4]
- Large verrucous plaques with multiple pustules and elevated border.
- Pseudoepitheliomatous hyperplasia with abscesses in tissue biopsy specimen.
- Growth of at least one pathogenic bacterium from the culture of a tissue biopsy specimen
- Negative culture for deep fungi, atypical mycobacteria and M. tuberculosis
- Negative fungal serology test result
- Normal bromide and iodide levels in the blood
Differential diagnosis includes North American blastomycosis, (ruled out by culture positivity for B. dermatitidis ) chromoblastomycosis, coccidioidomycosis and phycomycosis diagnosed by positive cultures. Cutaneous herpes infection presenting with vegetating verrucoid plaques can cause confusion, but these have hemorrhagic quality and cultures are positive. Prolonged ingestion and elevated blood levels of bromide suggesting bromoderma can present with verrucoid plaques. Pyoderma gangrenosum can be ruled out by characteristic irregular exudative and undermined edges of the ulcer. Histological differential diagnosis includes deep fungal infections like North or South American blastomycosis, bacterial infections like granuloma inguinale, lupus vulgaris, carcinomas like basal cell carcinomas, keratoacanthomas and bromodermas. [2]
Numerous treatment modalities have been attempted including systemic antibiotics like penicillin, minocycline, ciprofloxacin, cotrimoxazole and topical antibiotics, steroids, curettage, wet compresses and carbon dioxide laser debridement. [3] Nguyen RT et recently reported response of the disease to acitretin. [6]
The case highlights the importance of timely diagnosis of blastomycosis-like pyoderma which requires long term antibiotic therapy for satisfactory resolution of the skin lesions.
| 1. |
Bianchi L, Carrozzo AM orlandi A, Campione E, Hagman JH, Chimenti S. Pyoderma vegetans and ulcerative colitis. Br J Dermatol 2001;144:1224-7.
[Google Scholar]
|
| 2. |
Su WP, Duncan SC, Perry HO. Blastomycosis like pyoderma. Arch Dermatol 1979;115:170-3.
[Google Scholar]
|
| 3. |
Trygg KJ, Madison KC. Blastomycosis like pyoderma caused by Pseudomonas aeruginosa: Report of a case responsive to ciprofloxacin. J Am Acad Dermatol 1990;23:750-2.
[Google Scholar]
|
| 4. |
Singh M, Kumar B, Kaur S, Malik A. Blastomycosis like pyoderma. Indian J Dermatol Venereol Leprol 1985;51:226-8.
[Google Scholar]
|
| 5. |
Brown CS, Kligman AM. Mycosis like pyoderma. Arch Dermatol 1957;75:123-5.
[Google Scholar]
|
| 6. |
Nguyen RT, Beardmore GL. Blastomycosis-like pyoderma: Successful treatment with low-dose acitretin. Australas J Dermatol 2005;46:97-100.
[Google Scholar]
|
Fulltext Views
6,024
PDF downloads
2,621





