Translate this page into:
Blood-filled masses on scalp in a middle-aged woman
Corresponding author: Prof. Sujay Khandpur, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi - 110 029, India. sujay_khandpur@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Dev T, Bakhshi S, Naranje P, Khandpur S. Blood-filled masses on scalp in a middle aged woman. Indian J Dermatol Venereol Leprol 2021;87:82-5.
Sir,
Angiosarcoma is a rare aggressive tumor of malignant potential, with a poor 5-year survival rate.1 Fifteen percent of all head and neck sarcomas and 1% of all soft tissue sarcomas are angiosarcomas. Among all the sites,the skin and soft tissue is the most commonly involved location (approximately 60% cases), and half of these cases present in the head and neck, especially the scalp in elderly fair men with a median age of 65 to 70 years. The commonest sites of metastases include lungs, liver and lymph nodes.1,2 A 66-year-old woman presented to dermatology outpatient department with a 4-month history of gradually progressive, painless, hemorrhagic bullae and reddish-purple nodules and plaques on the scalp and forehead. She also had multiple daily episodes of cough, with mild to moderate hemoptysis for the past 3 months. Subsequently, she developed sudden onset right-sided chest pain and breathlessness and was radiologically found to have right-sided pneumothorax and left-sided hydropneumothorax, which was relieved with intercostal chest tube drainage. There was no history of weight loss, decreased appetite or fever. Dermatological examination revealed tense, approximately 3 × 3 cm sized hemorrhagic, blood-filled bullae and multiple reddish-purple nodules and plaques with overlying hemorrhagic crusting, bilaterally over the frontotemporal aspect of the scalp and the adjoining forehead, along with underlying ecchymosis and induration extending to the bilateral cheeks. The plaques were slightly warm, tender and associated with bleeding on palpation [Figures 1a-c]. Her ear, nose, throat, ocular and oral examination was normal and no locoregional lymphadenopathy was noted. Her co-morbidities included well-controlled hypothyroidism. The clinical differential diagnoses included primary cutaneous angiosarcoma, cutaneous metastasis with unknown primary, and a lesser possibility of primary systemic amyloidosis. Complete blood count and serum biochemistry were within normal limits, except moderate microcytic hypochromic anemia. Skin biopsy from the plaque showed large areas of hemorrhage and necrosis, along with deep dermal infiltration by irregular jagged vascular spaces, which were dissecting between the collagen bundles [Figures 2a-b]. The vascular spaces were lined by atypical endothelial cells, which were diffusely immunopositive for Friend Leukemia Virus Integration 1 and focally immunopositive for both CD31 and CD34 [Figure 2c]. High-resolution computed tomography of the chest showed bilateral multiple cavitary and noncavitary lung nodules with surrounding ground-glass opacities suggestive of hemorrhage, along with right pneumothorax and left hydropneumothorax [Figures 3a and b]. Positron emission tomography scan revealed multiple 18-fluoro-deoxy glucose-avid heterogeneously enhancing nodular lesions on the scalp without any bony erosions, multiple 18-fluoro-deoxy glucose-avid and nonavid cavitary and noncavitary nodules scattered in bilateral lung fields and few low-grade 18-fluoro-deoxy glucose-avid subcentimetric mediastinal lymph nodes. On bronchoscopy, a wide-based ulcerated lesion at the medial wall of the lower end of the left main bronchus was noted. Biopsy of this lesion and cytology of bronchoalveolar lavage did not show any evidence of malignancy, granulomas or fungal elements. Based on high-resolution computed tomography chest and Positron emission tomography-computed tomography findings, a diagnosis of primary cutaneous angiosarcoma with pulmonary metastasis (stage IV) was made. She was started on intravenous paclitaxel, initially at a dose of weekly 80 mg/m2 and once the patient’s general condition improved, it was changed to 160 mg/m2 every three weeks. Complete resolution of cough and hemoptysis was noted after 1 cycle of chemotherapy, while cutaneous lesions showed almost complete resolution after 5 cycles [Figures 4a-c]. Serial PET scans showed a significant decrease in extent, number and metabolic resolution of scalp thickenings, bilateral lung nodules and mediastinal lymph nodes. So far, she has received 15 cycles of chemotherapy uneventfully and no recurrence of cutaneous and pulmonary lesions has been noted. The patient is able to comfortably carry out her daily activities.

- Pre-treatment picture showing multiple hemorrhagic bullae and reddish-purple nodules and plaques, over both sides of forehead surrounded with ecchymosis and dusky erythematous ecchymotic macule over right cheek

- Pre-treatment picture showing a large dusky erythematous plaque over the right side of forehead with hemorrhagic crusting on the surface, surrounded by ecchymosis

- Pre-treatment picture showing multiple large hemorrhagic bullae and nodules and plaques over left side of forehead extending into the scalp
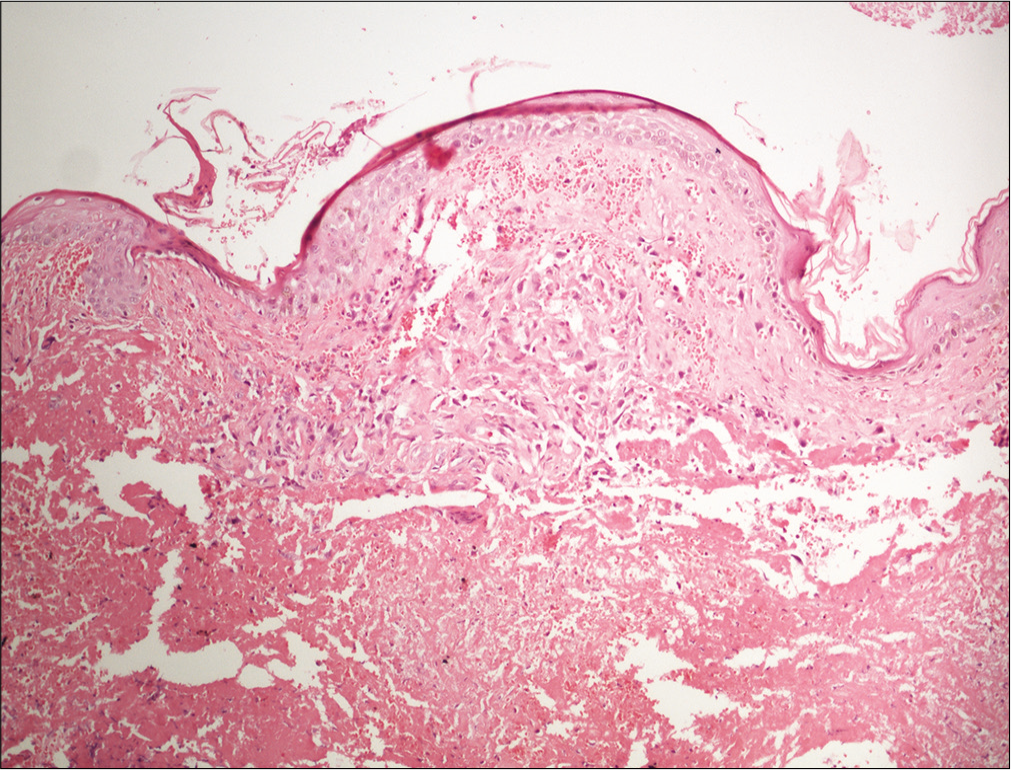
- Skin biopsy showing irregular anastomosing channels in the dermis, lined by endothelial cells with enlarged and hyperchromatic nuclei dissecting in H and E, x 20
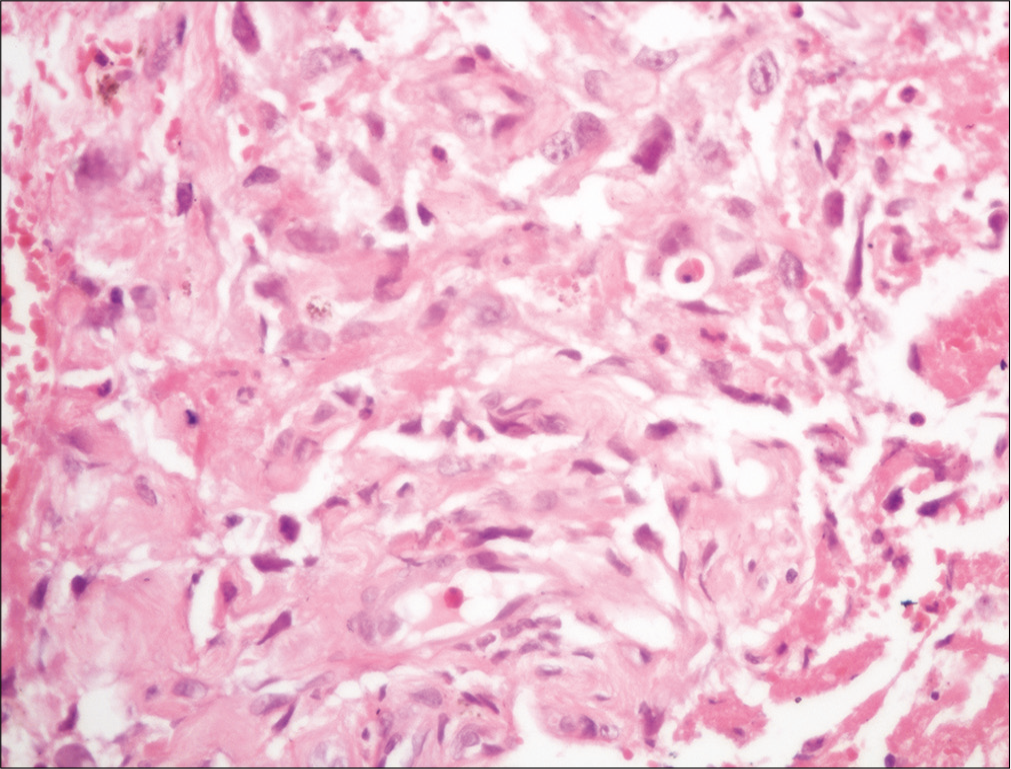
- Skin biopsy showing irregular anastomosing channels in the dermis, lined by endothelial cells with enlarged and hyperchromatic nuclei dissecting in between collagen bundles (H and E, ×400)
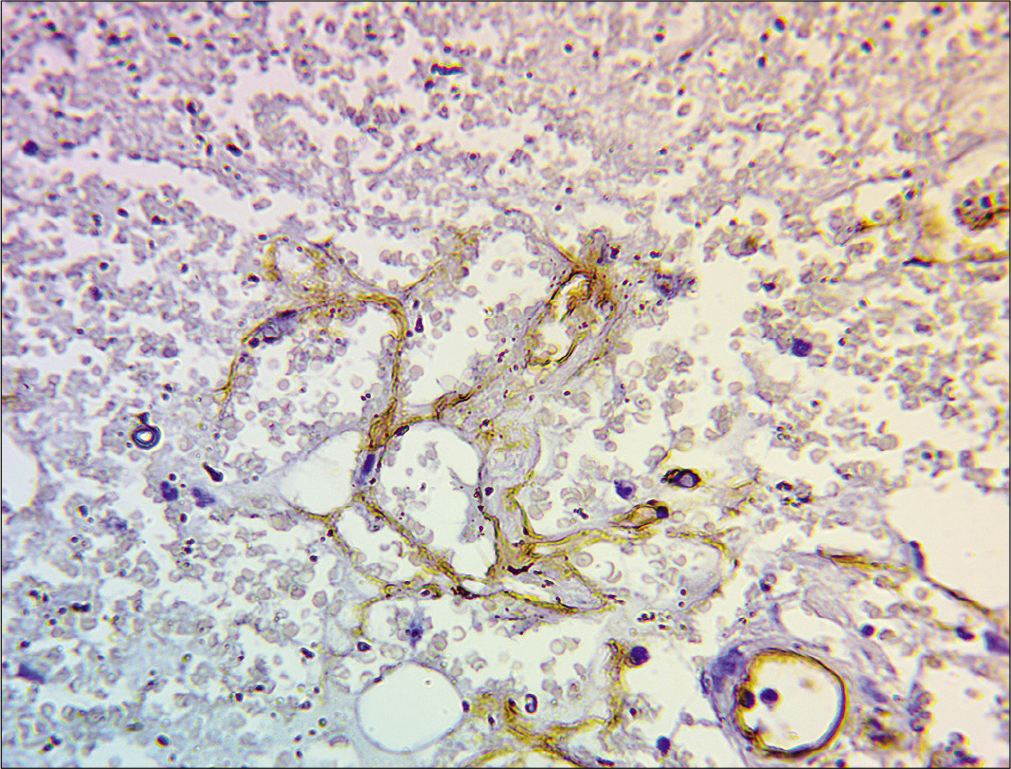
- Immunohistochemistry showing atypical endothelial cells showing focal positivity to CD 34, in × 400
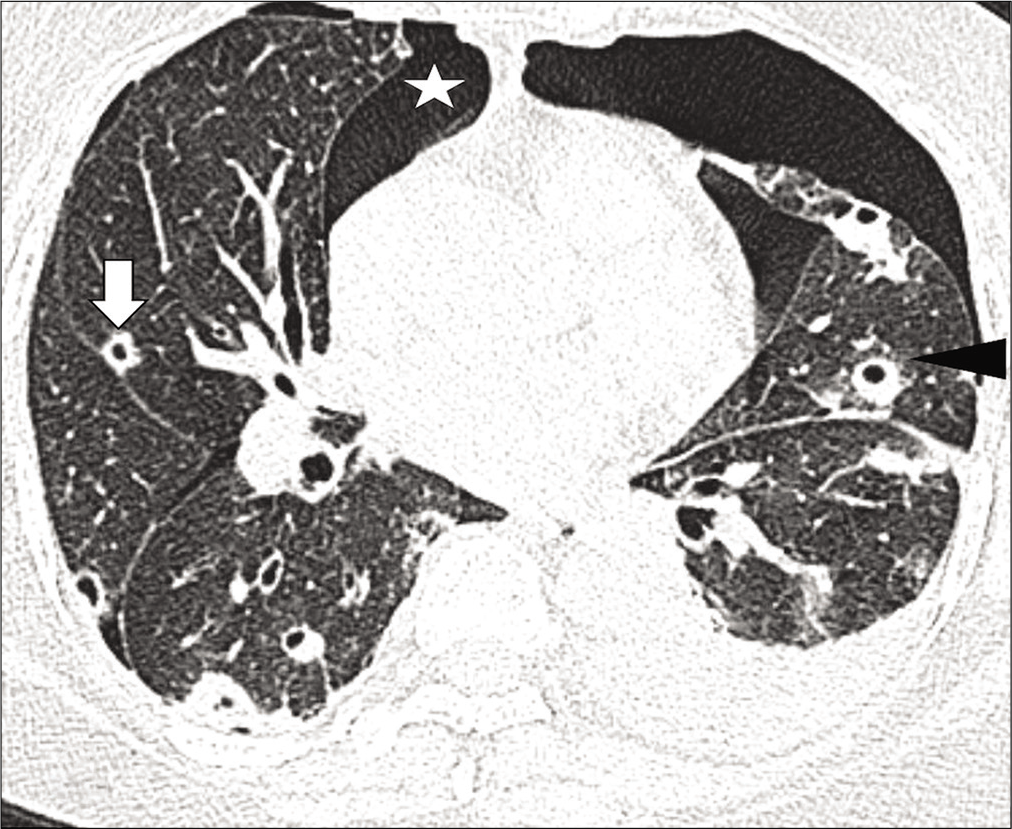
- High-resolution computed tomography chest axial lung window images show multiple random nodules, predominantly cavitary (white thick arrows), and some noncavitary (white thin arrow) with surrounding ground-glass opacities (arrowhead). Mild right pneumothorax (asterisk) and left hydropneumothorax (black arrow) are also noted
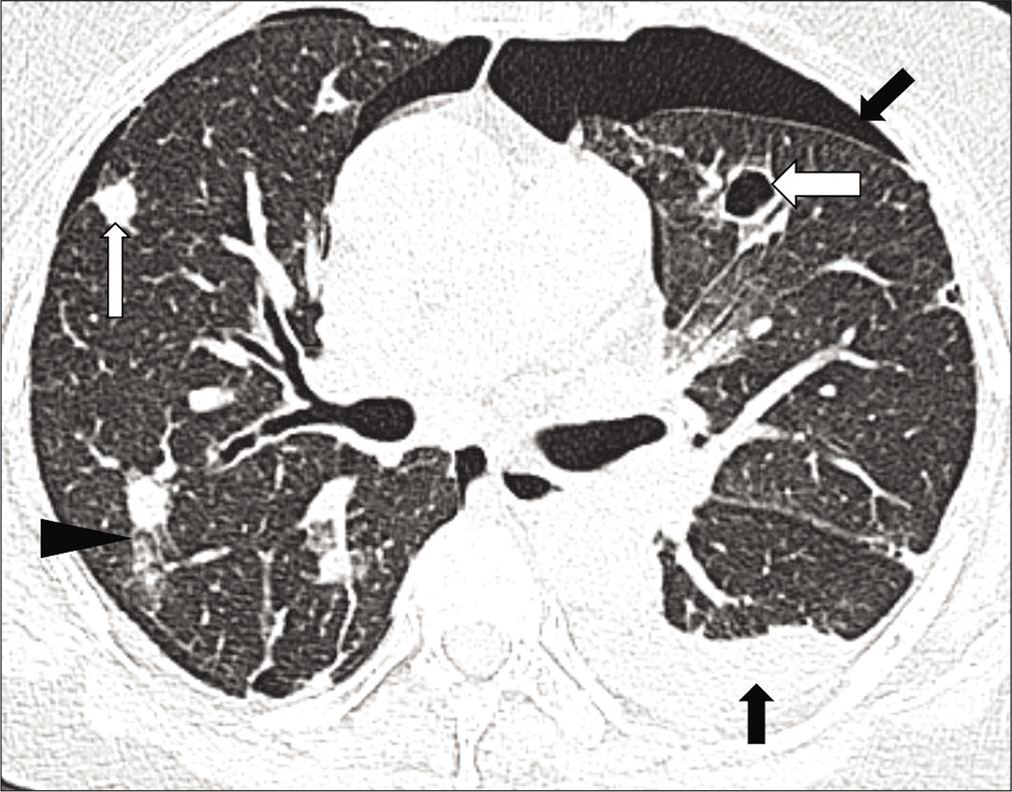
- High-resolution computed tomography chest axial lung window images show multiple random nodules, predominantly cavitary (white thick arrows), and some noncavitary (white thin arrow) with surrounding ground-glass opacities (arrowhead). Mild right pneumothorax (asterisk) and left hydropneumothorax (black arrow) are also noted

- Post-treatment picture (after 5 cycles of chemotherapy) showing significantly reduced lesions and complete resolution of ecchymosis over both sides of forehead and right cheek

- Post-treatment picture (after 5 cycles of chemotherapy) showing almost complete resolution of the plaque and surrounding ecchymosis over the right side of forehead with minimal residual crusting

- Post-treatment picture (after 5 cycles of chemotherapy) showing resolution of bullous nodules and plaques with minimal residual crusting
Our patient did not have any known risk factors like prior radiation exposure, chronic lymphedema or exposure to chemicals like arsenic, radium, thorium dioxide and polyvinyl chloride.3 Cutaneous angiosarcoma is characterized by a difficult delineation of surgical margins and a high tendency for local recurrence and distant metastases. No standard treatment guidelines are established due to the rarity of this tumor. In the majority of the cases, complete surgical resection with tumor-free margin is not possible. Surgical resection is the treatment of choice in localized angiosarcoma.4 Mark et al. reported a case series of 28 patients with angiosarcoma of the head and neck and concluded that combined modality therapy offers the best chance for long-term control in patients with angiosarcoma of the head and neck.5
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Prognosis of cutaneous angiosarcoma in Japan: A statistical study of sixty-nine cases. ChirPlastica. 1986;8:151.
- [CrossRef] [Google Scholar]
- Cutaneous angiosarcoma, Analysis of 434 cases from the Surveillance, Epidemiology, and End Results Program, 1973-2007. Ann Diagn Pathol. 2011;15:93-7.
- [CrossRef] [PubMed] [Google Scholar]
- Predisposing factors for poor prognosis of angiosarcoma of the scalp and face: Systematic review and meta-analysis. Head Neck. 2017;39:380-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous angiosarcoma: A current update. J Clin Pathol. 2017;70:917-25.
- [CrossRef] [PubMed] [Google Scholar]
- Angiosarcoma of the head and neck. The UCLA experience 1955, through, 1990. Arch Otolaryngol Head Neck Surg. 1993;119:973-8.
- [CrossRef] [PubMed] [Google Scholar]





