Translate this page into:
Bullous auto erythrocyte sensitization syndrome in alcohol dependence
2 Department of Psychiatry, Air Force Hospital, Kanpur Cantt, Uttar Pradesh, India
3 Department of Pathology, Air Force Hospital, Kanpur Cantt, Uttar Pradesh, India
Correspondence Address:
Sandeep Arora
Skin Centre, Base Hospital, Delhi Cantt-110010
India
| How to cite this article: Arora S, Arora G, Gupta AK, Singh G. Bullous auto erythrocyte sensitization syndrome in alcohol dependence. Indian J Dermatol Venereol Leprol 2013;79:269 |
Sir,
Auto erythrocyte sensitization syndrome also known as Gardner-Diamond Syndrome is a "Painful Bruising Syndrome" arising as a result of sensitivity to platelet phosphatidyl serine. [1] It was initially reported in 1955 in four women and has since been reported mostly in women of the younger age group, with an underlying psychiatric disorder. [2]
The dermatological manifestations typically include recurrent spontaneous ecchymoses following a stressful event which subside gradually only to recur again. The associated complaints often include gastrointestinal symptoms in more than half [2] or neurological, ocular, hemorrhagic manifestations such as menorrhagia, hematuria and other varied symptomatology. [3] Rarely these patients have reported with bullous lesions. [4],[5]
A 25-year-old young male presented with recurrent dark colored lesions, some with bullae after an odd burning sensation at the site of the lesions on the scalp, neck, trunk and extremities for the past 6 months. The lesions would subside over the next few days with bruise like changes along with resolution of the bulla and residual hyperpigmentation. The patient volunteered history of consuming alcohol about 3-4 years ago as a social drinker and since then increased gradually in past few years to the present level of up to 240-300 ml of spirits on almost all days a week with exhibition of craving, tolerance and palpitation with insomnia in delaying/reducing drinking. More frequent episodes of such binges over the past 6 months along with stress had resulted in frequent such black eruptions with blisters and hence he sought medical attention.
Examination revealed multiple tender black ecchymotic lesions some with bullae over the accessible as well as non-accessible sites on the scalp, neck, trunk and extremities [Figure - 1]. These lesions were observed to subside over a period of 7-10 days with resolution in a bruise like manner with post inflammatory hyperpigmentation. He was observed as an admitted patient to rule out dermatitis artefacta. Although some lesions coincided to sites of scratching, obvious self-induced injury was ruled out by close observation.
 |
| Figure 1: Bullous ecchymotic lesions over arm with close up (inset) |
Mental status examination and ward observation noted a kempt, anxious, restless individual with normal speech, dysphoric mood and anxious affect. No thought/perceptual disturbances were noted. He had alcoholic rationalizations. No cognitive deficits were noted. Sensorium was clear. Insight and judgment was colored by his alcohol-related psychological defenses. Bio-drives noted initial insomnia, poor appetite and energy levels.
Investigations revealed elevated aspartate aminotransferase/alanine aminotransferase and gamma glutamyl transferase, ultrasonography abdomen showed hepatomegaly. Hemogram and coagulation profile were normal. Skin biopsy of the bullous lesion revealed a sub epidermal split with mixed inflammatory infiltrate and extravasation of red blood cells and hemosiderin deposition at places [Figure - 2].
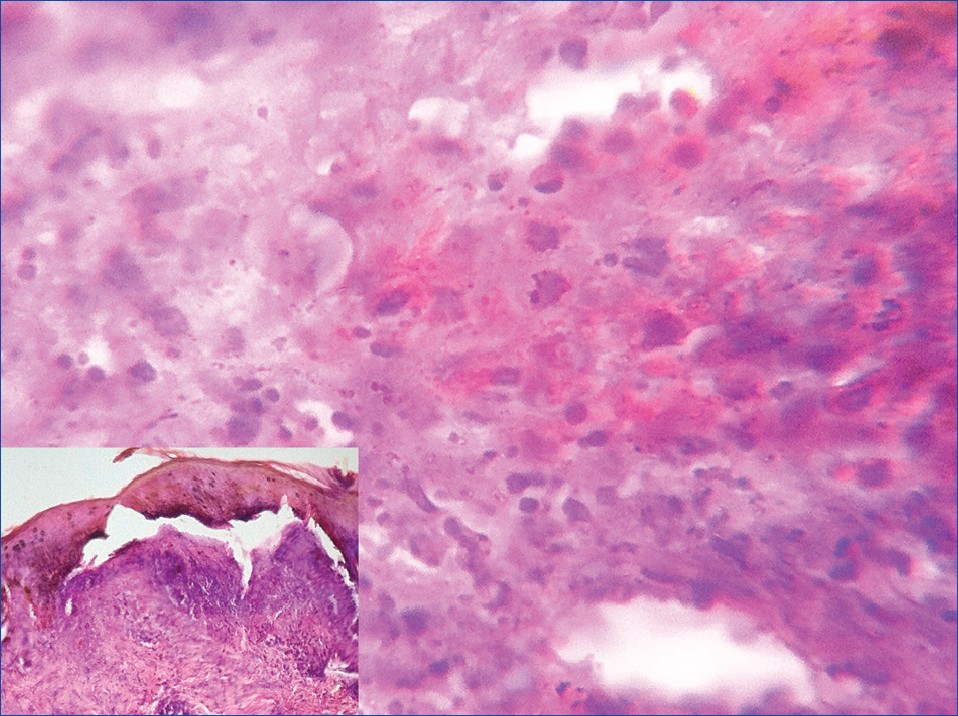 |
| Figure 2: Photomicrograph of the inflammatory infiltrate and haemosiderin (H and E, ×40) and bullous lesion showing subepidermal split with mixed inflammatory cell infiltrate (H and E, ×10) as inset |
An intradermal test for autoerythrocyte sensitization was done with washed RBCs of the patient in the inaccessible region of the interscapular area with a saline control on the opposite side. A painful ecchymotic reaction was noted at the site of injection, similar to his presenting lesions. There was no reaction at the control site.
He was treated with forced abstinence, vitamin supplements, anti-craving agents (Tab Naltrexone 25 mg BD, Tab Topiramate 50 mg BD), psychotherapy and other supportive measures. He responded well to treatment.
A follow-up period of 1 year did not reveal any fresh lesions, he has abstained from alcohol consumption and his biochemical profile has returned to normal.
Bullous lesions in this rare disorder are extremely uncommon with the only two other reports in female patients. [4],[5] A literature search reveals varied clinical presentation of these patients with and without dermatitis artefacta. [2],[3] In our case, dermatitis artefacta as a cause of all the lesions, which were not linear, regularly outlined or homogeneous, distributed on inaccessible sites as well, was ruled out by close observation of the patient as an admitted case. However, the presence of bruising of auto erythrocyte sensitization at the sites of occasional trauma supports the diagnosis as the inflammatory response of autoerythrocyte sensitization is manifest at the site of injury. The hairy scalp was shaved by the patient only after the initial presentation which already had manifest lesions.
A male patient with Gardner-Diamond Syndrome with bullous lesions with coexistent alcohol dependence is interesting. Recognition of alcohol dependence as an aggravating factor as a primary psychiatric ailment in such patients is important as this may be missed in the lookout for the psychiatric disorders usually associated with this syndrome. [2] Management of the primary psychiatric ailment is usually curative for the dermatological disorder as was in our case.
| 1. |
Groch GS, Finch SC, Rogoway W, Fischer DS. Studies in the pathogenesis of autoerythrocyte sensitization syndrome. Blood 1966;28:19-33.
[Google Scholar]
|
| 2. |
Thappa DM, Kumari R. Current best evidence from dermatology literature. Indian J Dermatol Venereol Leprol 2009;75:332-5.
[Google Scholar]
|
| 3. |
Sawhney MP, Arora G, Arora S, Prakash J. Undiagnosed purpura: A case of autoerythrocyte sensitization syndrome associated with dermatitis artefacta and pseudo-ainhum. Indian J Dermatol Venereol Leprol 2006;72:379-81.
[Google Scholar]
|
| 4. |
Chatterjee M, Jaiswal AK. Painful bruising syndrome. Indian J Dermatol Venereol Leprol 2002;68:347-8.
[Google Scholar]
|
| 5. |
Gaikwad RP, Deshpande SS, Dhamdhere DV. Painful bruising syndrome presenting as bullous lesions. Indian J Dermatol 2011;56:245-6.
[Google Scholar]
|
Fulltext Views
1,964
PDF downloads
1,742





