Translate this page into:
Bullous eosinophilic cellulitis with subcorneal pustules
Correspondence Address:
Hideaki Watanabe
Department of Dermatology, Showa University School of Medicine, 1-5-8, Hatanodai, Shinagawa-ku, Tokyo 142-8555
Japan
| How to cite this article: Kamiyama T, Watanabe H, Sueki H. Bullous eosinophilic cellulitis with subcorneal pustules. Indian J Dermatol Venereol Leprol 2015;81:301-303 |
Sir,
Eosinophilic cellulitis, or Wells syndrome, is an uncommon inflammatory dermatosis of unclear pathogenesis, often characterized by erythematous, edematous plaques that resemble acute bacterial cellulitis or urticaria. Recently, a variety of clinical lesions have been reported in patients with eosinophilic cellulitis, including papules, nodules, vesicles, and, rarely, bullae. However, only a few cases of non-bullous eosinophilic cellulitis with subcorneal pustules have been reported. [1],[2] Here, we describe a patient with bullous eosinophilic cellulitis showing subcorneal neutrophilic and eosinophilic pustules.
A 39-year-old Japanese female presented with a 1-month history of severely pruritic, erythematous vesicular eruptions on her extremities and a 1-week history of erythematous papular lesions on her trunk, which did not respond to oral antihistamines and a topical steroid. There was no history of any antecedent drug intake, chronic sinusitis or asthma.
On physical examination, there were well-demarcated, oval, edematous, erythematous plaques, vesicles, bullae and pustules on the dorsa of the hands, forearms, and soles [Figure - 1]a. The patient had tenderness in these areas. Moreover, multiple erythematous lesions with papules, pustules and crusts were present on the trunk and extremities [Figure - 1]b. She did not have any systemic symptoms such as malaise, fever or arthralgia. Laboratory studies were significant for a white blood cell count of 8400/μL with 15% eosinophils. All other laboratory data, including autoantibodies, were within normal limits. Bacterial culture from a pustule was sterile. A diagnosis of eosinophilic cellulitis was suspected; however, other clinical differentials considered were pyoderma gangrenosum, Sweet′s syndrome, and contact dermatitis with id reaction.
 |
| Figure 1: (a) Edematous erythematous plaques, vesicles, bullae, and pustules on the dorsum of the hand and distal forearm. (b) Erythematous plaques with papules, pustules, and crusts on the abdomen |
Two skin biopsies were performed, one from the bullous lesion on right forearm and another from the erythematous plaque on the abdomen [Figure - 1]a and b]. Histological examination of the forearm lesion showed subcorneal pustules containing mainly neutrophils, severe dermal edema resulting in subepidermal blisters and dense infiltration consisting of equal numbers of eosinophils and neutrophils throughout the dermis [Figure - 2]a and b. Flame figures were observed in the dermis [Figure - 2]c. Biopsy from the abdominal lesion showed subcorneal pustules containing predominantly eosinophils [Figure - 2]d. Perivascular and interstitial infiltrates of eosinophils and lymphocytes as well as flame figures were found in the dermis [Figure - 2]e. There was no vasculitis. Direct immunofluorescence was negative for immunoglobulin G (IgG), IgA, IgM, and C3. Indirect immunofluorescence using monkey esophagus and salt-split human skin as substrates showed no circulating IgG or IgA autoantibodies.
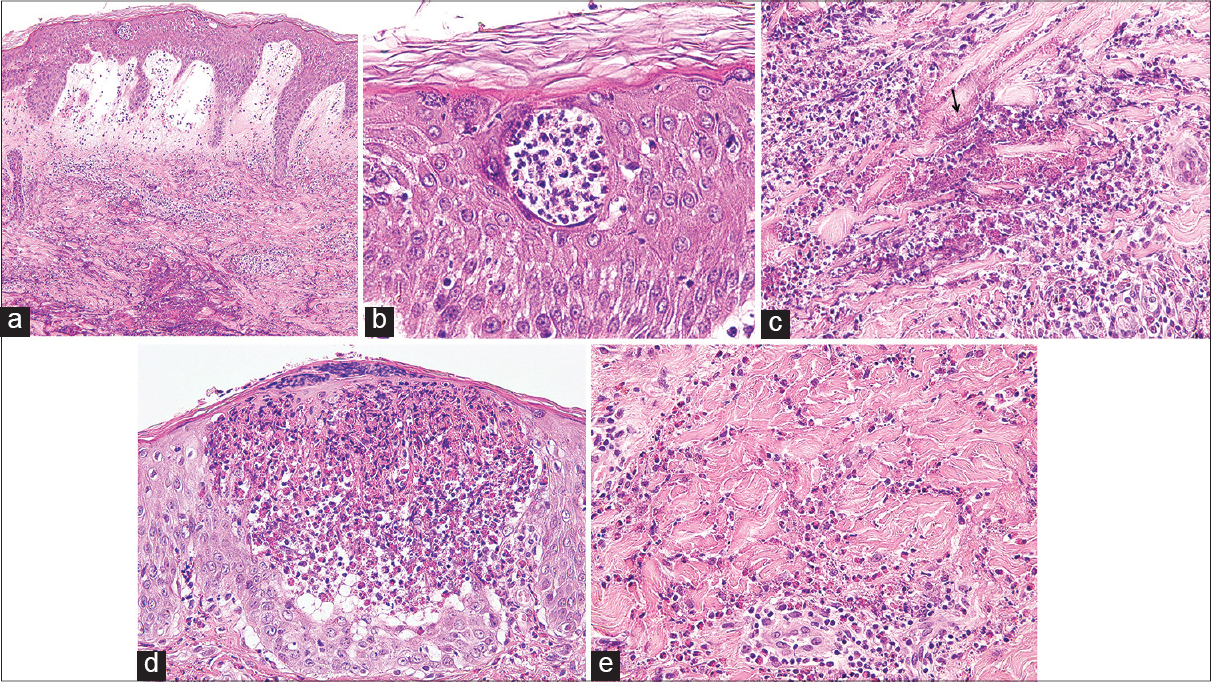 |
| Figure 2: (a) The bullous lesion shows subcorneal pustules, subepidermal blisters, papillary dermal edema, and dense infiltration of neutrophils and eosinophils involving the full thickness of the dermis (H and E, ×100). (b) Subcorneal pustules containing mainly neutrophils (H and E, ×400). (c) Flame figures in the dermis (H and E, ×400). (d) The erythematous plaque shows subcorneal pustules containing many eosinophils (H and E, ×400). (e) Aggregates of eosinophilic granules and nuclear fragments around collagen bundles in the dermis. Perivascular and interstitial infiltrate of eosinophils and lymphocytes as well as flame figures in the dermis (H and E, ×400) |
Based on these findings, a diagnosis of bullous eosinophilic cellulitis was made. The patient was commenced on prednisolone 0.5 mg/kg daily and fexofenadine 60 mg twice daily combined with a topical steroid. Clinical improvement of the skin lesions was observed 2 weeks after treatment. Prednisolone use was tapered and discontinued after 9 weeks. During a six month follow up period, there was no clinical relapse or eosinophilia.
Subcorneal pustules are very rare in eosinophilic cellulitis, and have previously been described only in two cases of eosinophilic cellulitis; [1],[2] however, both these cases were of non-bullous eosinophilic cellulitis. We were unable to find any previous report of bullous eosinophilic cellulitis, which histologically showed subcorneal pustules. Takata et al., [1] reported cutaneous botryomycosis followed by non-bullous eosinophilic cellulitis with sterile subcorneal pustules. Chao et al., [2] reported non-bullous eosinophilic cellulitis with subcorneal pustules, diagnosed as an id reaction, after a molten aluminium burn. Although two cases of bullous eosinophilic cellulitis with pustules have been reported, [3],[4] histological features of the pustules were not described.
The important finding in this case was that subcorneal neutrophilic pustules and subcorneal eosinophilic pustules were observed simultaneously; however, it is difficult to explain the findings. We think that these two forms of pustules might be due to different pathogenic mechanisms or simply due to the time course of each lesion. A biopsy from the abdominal lesion performed 1 week after the appearance of the erythematous papules showed subcorneal eosinophilic pustules. By contrast, a biopsy from the right forearm performed 1 month after the occurrence of the vesicular eruptions displayed subcorneal neutrophilic pustules. Indeed, Takata et al. [1] performed a biopsy 3 weeks after onset and diagnosed eosinophilic cellulitis with subcorneal eosinophilic pustules, whereas Chao et al., [2] performed a biopsy after 6 weeks and diagnosed eosinophilic cellulitis with subcorneal pustules containing both neutrophils and eosinophils. Eosinophils can release interleukin (IL)-8, which exhibits chemotactic activity for neutrophils. [5] We postulate that subcorneal eosinophilic pustules could be sequentially replaced by subcorneal neutrophilic pustules.
| 1. |
Takata T, Nakajima H, Ikeda M, Kodama H, Tamaki H, Sano S. Cutaneous botryomycosis associated with eosinophilic cellulitis. J Dermatol 2009;36:551-4.
[Google Scholar]
|
| 2. |
Chao SC, Lee YP, Lee JY. Eosinophilic cellulitis and panniculitis with generalized vesicular pustular id reaction after a molten aluminum burn. Dermatitis 2010;21:E11-5.
[Google Scholar]
|
| 3. |
Zhu L, Hu D, Wang Q, Hou J, Li M. Diffuse polymorphic Eosinophilic cellulitis in a patient with metallic alloy implants: A possible association? Int J Dermatol 2011;50:1535-7.
[Google Scholar]
|
| 4. |
Yin G, Xie Q. Systemic lupus erythematosus associated with Wells' syndrome. Rheumatol Int 2012;32:1087-9.
[Google Scholar]
|
| 5. |
Yousefi S, Hemmann S, Weber M, Hölzer C, Hartung K, Blaser K, et al. IL-8 is expressed by human peripheral blood eosinophils. Evidence for increased secretion in asthma. J Immunol 1995;154 5481-90.
[Google Scholar]
|
Fulltext Views
3,736
PDF downloads
2,002





