Translate this page into:
Bullous pyoderma gangrenosum associated with ulcerative colitis
2 Department of Medicine, Sri Devraj Urs Medical College (DEEMED UNIVERSITY), Tamaka, Kolar - 563 101, Karnataka, India
Correspondence Address:
Chandra Lal Naik
Department of Dermatology and STD, Sri Devraj Urs Medical College, Tamaka, Kolar - 563 101, Karnataka
India
| How to cite this article: Naik CL, Singh G, Kumar L, Lokanatha K. Bullous pyoderma gangrenosum associated with ulcerative colitis. Indian J Dermatol Venereol Leprol 2008;74:68-70 |
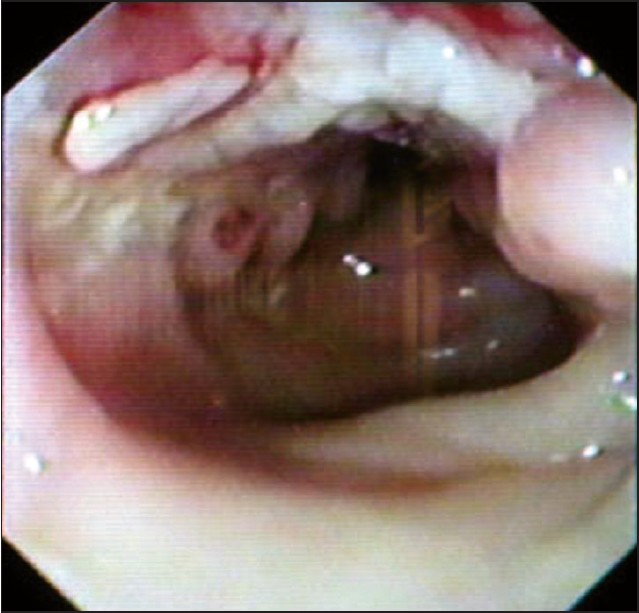 |
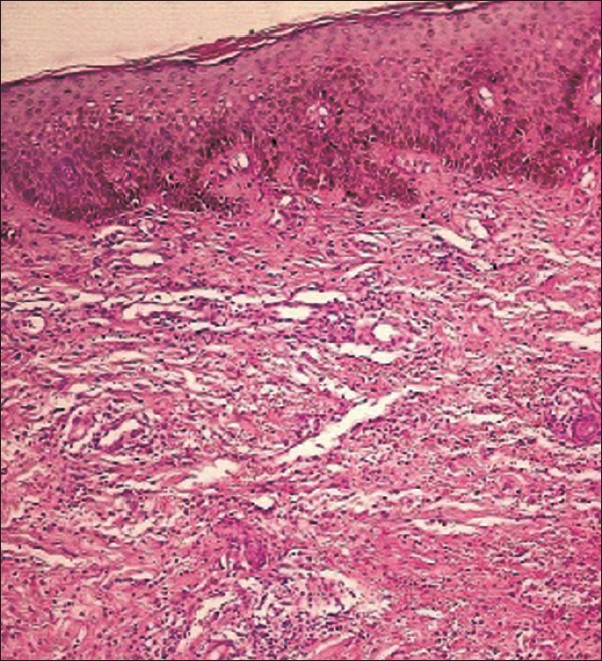
| Figure 3: Colonoscopy showing multiple ulcers in the colon |
 |
| Figure 3: Colonoscopy showing multiple ulcers in the colon |
 |
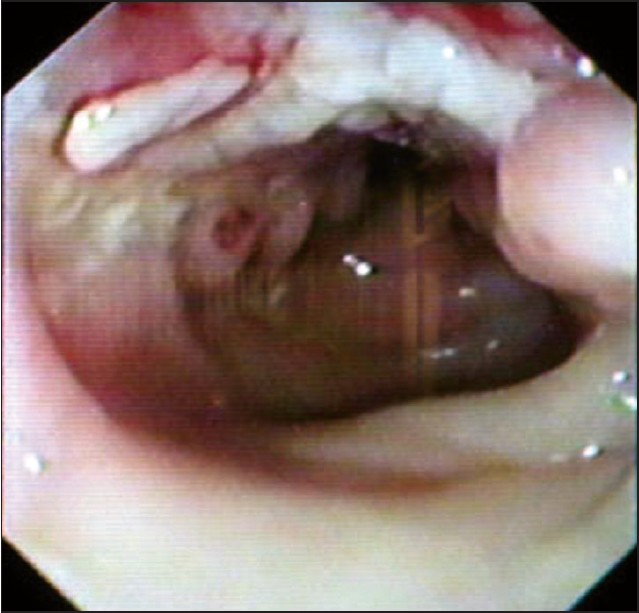
| Figure 2: Dermis showing perivascular lymphocytic infiltration and focal neutrophilic abscess (H and E, X100) |
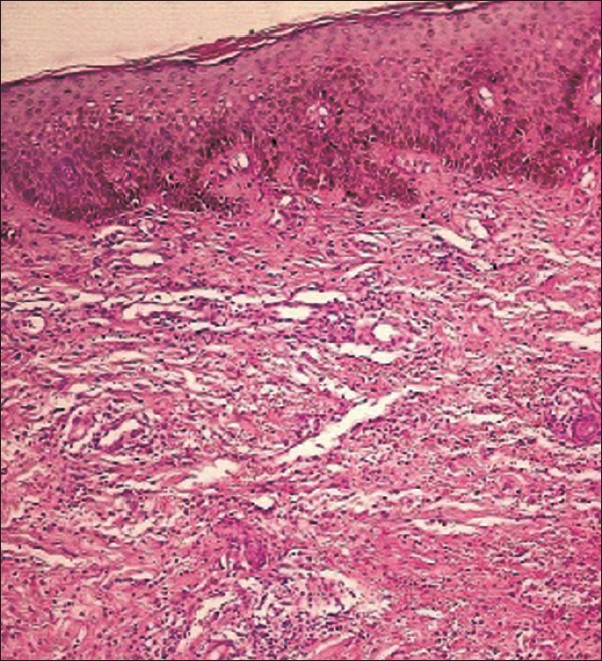 |
| Figure 2: Dermis showing perivascular lymphocytic infiltration and focal neutrophilic abscess (H and E, X100) |
 |
| Figure 1: Multiple vesiculobullous and pustular lesions over the fore arm and extending to the palm |
 |
| Figure 1: Multiple vesiculobullous and pustular lesions over the fore arm and extending to the palm |
Sir,
Pyoderma gangrenosum (PG) is a rare non-infectious neutrophilic dermatosis associated with underlying systemic disease, characterized by distinctive cutaneous ulcers with undermined borders; lesions usually require aggressive therapy and they heal with a characteristic cribriform scar. We report a case of bullous PG associated with ulcerative colitis.
A 55-year-old woman presented with multiple fluid-filled lesions and ulcers over the upper and lower limbs and trunk of two months duration. There was a history of fever and loose stools on and off and loss of weight since two years. History of development of lesions at the site of trauma was elicited. There was no history of extramarital sexual contact, joint pains, mucosal ulcers and any other systemic symptoms. Examination revealed multiple, tender ulcers of varying size with undermined violaceous borders, vesicles and bullae [Figure - 1] distributed over bilateral lower and upper limbs, palms and soles and a few over the trunk. Mucosa, hair and nails were normal. Systemic examination revealed no abnormality.
On investigation, peripheral smear showed hypochromic anemia with neutrophilia; renal function tests and liver function tests were within normal limits, serologic testing revealed negativity for VDRL, HIV 1 and -2, ANA, HBsAg and RA factor. Both bacterial and fungal cultures from the surface of ulcer were sterile; chest X-ray and ultrasound abdomen did not reveal any significant abnormality. No reaction was observed with Mantoux test. Colonoscopy and sigmoidoscopy showed red colonic mucosa with multiple ulcers of varying sizes and shapes and few pseudopolyps distributed throughout the length of the colon [Figure - 2].
The skin biopsy taken from the edge of an ulcer revealed normal epidermis with dermis showing perivascular lymphocytic infiltration with endothelial swelling and focal neutrophilic abscess [Figure - 3]. Pyoderma gangrenosum commonly occurs in immunosuppressed patients secondary to accompanying disease, infections or therapy. [1] The pathophysiology is poorly understood, an immune-mediated pathogenesis is suspected, both humoral and cell-mediated abnormalities have been associated with PG. [2]
The skin lesions of PG appear as tender vesiculobullous, papulopustular lesions that develop into painful ulcers with dusky purple borders that are raised and undermined. The base of the ulcer typically reveals both granulation tissue and necrotic material. Lesion may be solitary or multiple and shows pathergy phenomenon. Several variants of PG have been described; ulcerative, pustular, bullous and vegetative, vulvar and peristomal PG. The peristomal PG is a recently recognized variant that occurs primarily in patients with inflammatory bowel disease. The skin lesions usually appear during the course of active bowel disease and frequently concur with exacerbation of colitis. [3]
Other diseases commonly associated with PG include arthritis, hematological diseases and rarely chronic active hepatitis, myeloma, Takayasu′s arteritis, systemic lupus erythematosus, Wegener′s granulomatosis, diabetes mellitus, HIV infection and other neutrophilic pustular dermatoses, particularly Behηet′s syndrome. [4] Several studies have documented patients with PG and Behηet′s syndrome, the two diseases share certain features such as arthritis, pustulation, aphthous lesions of mucous membranes and the phenomenon of pathergy. [4],[5]
The association of PG with ulcerative colitis varies from 1-50% in various studies, however, PG is an extremely rare disease occurring in less than 1% of patients with inflammatory bowel disease with an equal ratio of patients with Crohn′s disease and ulcerative colitis, and similarly various other studies also demonstrated an incidence of less than 1%. [6],[7] Conversely 0.5-5% patients with ulcerative colitis have PG. [8]
| 1. |
Haim S, Friedman-Birnbaum R, Better OS. Skin complications in immunosuppressed patients: Follow-up of kidney recipients. Br J Dermatol 1973;89:169-73.
[Google Scholar]
|
| 2. |
Barham KL, Jorizzo JL, Grattan B, Cox NH. Vasculitis and Neutrophilic Vascular Reactions. In: Burns T, Brethnach S, Cox N, Griffith C, editors. Rook's Text Book Of Dermatology. 7 th ed. Oxford: Blackwell Science Publishing; 2004. p. 49.1-49.46.
th ed. Oxford: Blackwell Science Publishing; 2004. p. 49.1-49.46.'>[Google Scholar]
|
| 3. |
Callen JP. Neutrophilic dermatoses. Dermatol Clin 2002;20:409-19.
[Google Scholar]
|
| 4. |
Rustin MH, Gilkes JJ, Robinson TW. Pyoderma gangrenosum associated with Behcet's disese: Treatment with thalidomide. J Am Acad Dermatol 1990;23:941-4.
[Google Scholar]
|
| 5. |
Munro CS, Cox NH. Pyoderma gangrenosum associated with Behcet's syndrome: Response to thalidomide. Clin Exp Dermatol 1988;13:408-10.
[Google Scholar]
|
| 6. |
Veloso FT, Carvalho J, Magro F. Immune related systemic manifestations of inflammatory bowel disease: A prospective study of 792 patients. J Clin Gastroenterol 1996;23:29-34.
[Google Scholar]
|
| 7. |
Menachem Y, Gotsman I. Clinical manifestations of pyoderma gangrenosum associated with inflammatory bowel disease. Isr Med Assoc J 2004;6:88-90.
[Google Scholar]
|
| 8. |
Basler RS. Ulcerative colitis and the skin. Med Clin North Am 1980;64:941-54.
[Google Scholar]
|
Fulltext Views
3,222
PDF downloads
2,387





