Translate this page into:
Cauliflower like growth in the groins
2 Department of Pathology, Sri Devaraj Urs Medical College, Tamaka, Kolar, Karnataka, India
Correspondence Address:
G Rajesh
Senior Resident, Department of Dermatology, Sri Devaraj Urs Medical College, Tamaka, Kolar - 563 101, Karnataka
India
| How to cite this article: Rajesh G, Kumar M U. Cauliflower like growth in the groins. Indian J Dermatol Venereol Leprol 2012;78:661-663 |
A 38-year-old male presented with large cauliflower-like growth in his groins since 15 years. The growth started insidiously as small pigmented raised lesions in the groins. The lesions were aymptomatic and gradually increased in size laterally in the inguinal region and inwards into the perineum. There was no history of sexual promiscuity in either spouse. Examination revealed polypoidal swellings in the inguinal region extending downwards into the perineum along the lateral end of scrotum (20 × 8 cms - in the right groin, 8 × 5 cms- in the left groin) [Figure - 1]. The growth was soft in consistency, mobile, and non-tender. External genitalia were normal. Biopsy was done and histopathology of the tumor showed marked hyperkeratosis, papillomatosis, acanthosis and with sharp horizontal demarcation from the dermis. The epidermis showed squamous and basaloid cells with several horncysts [Figure - 2].
 |
| Figure 1: Giant polypoidal pigmented growth in the bilateral groins |
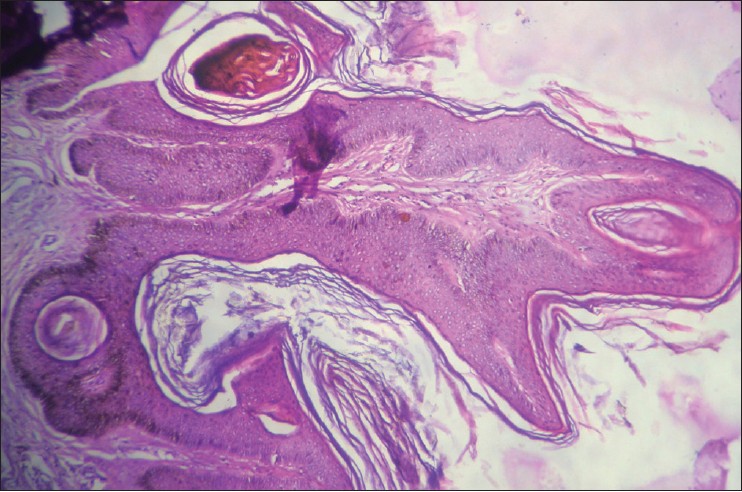 |
| Figure 2: Histological section shows marked hyperkeratosis, papillomatosis, acanthosis, and horn cysts. (H and E, ×100) |
What is your diagnosis?
Answer: Hyperkeratotic seborrheic keratosis.
Histopathology: Asymptomatic pigmented growth with histopathology showing hyperkeratosis, squamous, and basaloid cells and horncysts confirms the diagnosis hyperkeratotic seborrheic keratosis.
Discussion
Seborrheic keratoses (SK) (also known as seborrheic warts, senile warts, verruca seborrheica, basal cell papilloma, basal cell acanthoma, and benign acanthokeratoma) are benign epidermal tumors composed of epidermal keratinocytes. [1] The lesion of SK can occur at any site but most frequently seen on face and upper trunk. The lesions are usually asymptomatic but may be itchy. It begins as well-circumscribed, dull, flat, tan, or brown patches. As they grow, they become more papular, taking on a waxy verrucous or ′stuck on′ appearance. [1] Clinical variants include common SK, dermatosis papulosa nigra, pedunculated SK, flat SK, stucco keratoses. [2]
The precise etiology of SK is unknown. Genetics, sun exposure, and infection have all been implicated as possible factors. [3] Multiple SK may be a familial trait with an autosomal dominant inheritance. [1] Viral infection has also been considered as possible cause of SK; epidermodysplasia verruciformis-associated HPV DNA has been demonstrated on non-genital SK biopsies. [2] New insights have been gained in recent years in the molecular pathogenesis. Studies have reported high frequency of mutations of FGFR3 and PIK3CA in certain types of SK, supporting the concept that the variants of SK share a common genetic background. [4]
Six types of histologic variants are recognized; acanthotic, hyperkeratotic, adenoid, clonal, irritated, and melanoacanthoma. All SK have in common hyperkeratosis, acanthosis, and papillomatosis. Two types of cells are seen in acanthotic epidermis; squamous cells (have the appearance of squamous cells, normally found in the epidermis) and basaloid cells (resemble basal cells, found normally in basal layer of epidermis). [5] Of these, the acanthotic subtype appears to be the most common. But, in our case, hyperkeratosis and papillomatosis was marked. Squamous eddies, as seen in irritated SK, was absent.
Seborrheic keratosis involving the genital region is a rare entity, which can be easily misdiagnosed as genital warts. Giant SK situated in the anogenital region often resemble condylomata acuminata clinically and histopathologically, yet they are benign neoplasms of unknown cause, in contrast to condylomata acuminata, which are hyperplasias induced by human papillomavirus (HPV). [6] HPV studies were not done in our case due to lack of facility. Recently, dermoscopy is available as a non-invasive diagnostic procedure, which can be used to diagnose SK by its typical findings; milia-like cysts, comedo-like openings, fissures and ridges, moth eaten borders, hair-pin blood vessels, finger-print like structures, network-like structures, and sharp demarcation. [2]
Thakur et al[7] reported a case of SK of the penis in a 50-year-old, presenting as multiple giant polypoidal lesions on penile skin and suggested that SK should be considered in differential diagnosis of pedunculated lesions in skin. Livaoglu et al[8] reported a similar large, polypoidal SK in the genitalia in a 42-year-old male patient. Shenoy et al[9] reported a case of melanoacanthoma in the genital region.
Treatment options for SK include simple curettage, cautery, cryotherapy, or laser ablation. Larger lesions requiring skin surgery are usually removed by excision. We advised surgical excision for our patient.
| 1. |
Mackie RM, Quinn AG. Non-melanoma skin cancer and other epidermal skin tumours. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7 th ed. Oxford: Blackwell Publishing; 2004. p. 36.1-36.50.
th ed. Oxford: Blackwell Publishing; 2004. p. 36.1-36.50.'>[Google Scholar]
|
| 2. |
Rajesh G, Thappa DM, Jaisankar TJ, Chandrashekar L. Spectrum of seborrheic keratoses in south Indians: A clinical and dermoscopic study. Indian J Dermatol Venereol Leprol 2011;77:483-8.
[Google Scholar]
|
| 3. |
Thomas VD, Swanson NA, Lee KK. Benign epithelial tumors, hamartomas and hyperplasias. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell D, editors. Fitzpatrick's Dermatology in General Medicine. 7 th ed. New York: McGraw-Hill; 2008. p. 1054-67.
th ed. New York: McGraw-Hill; 2008. p. 1054-67.'>[Google Scholar]
|
| 4. |
Hafner C, Landthaler M, Mentzel T, Vogt T. FGFR3 and PIK3CA mutations in stucco keratosis and dermatosis papulosa nigra. Br J Dermatol 2010;162:508-12.
[Google Scholar]
|
| 5. |
Kirkham N. Tumors and cysts of the epidermis. In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, editors. Lever's Histopathology of the Skin. 9 th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. p. 806-66.
th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. p. 806-66.'>[Google Scholar]
|
| 6. |
Li J, Ackerman AB. " Seborrheic keratoses" that contain human papillomavirus are condyloma acuminate. Am J Dermatopathol 1994;16;398-405.
[Google Scholar]
|
| 7. |
Thakur JS, Thakur A, Chauhan C, Diwana VK, Chauhan DC. Giant pedunculated seborrheic keratosis of penis. Indian J Dermatol 2008;53:37-8.
[Google Scholar]
|
| 8. |
Livaoglu M, Karacal N, Gücer H, Arvas L. Giant genital seborrheic keratosis. Dermatol Surg 2007;33:1357-8.
[Google Scholar]
|
| 9. |
Shenoy MM, Teerthanath S, Bhagavan KR. Genital and perianal melanoacanthomas. Indian J Dermatol 2007;52:109-10.
[Google Scholar]
|
Fulltext Views
9,544
PDF downloads
2,228





