Translate this page into:
Changing trends in leprosy among patients attending a tertiary care institution
2 Department of Community Medicine, Government Medical College, Kozhikode, Kerala, India
Correspondence Address:
Sarita Sasidharanpillai
'Rohini', Girish Nagar, Nallalom PO, Kozhikode - 673 027, Kerala
India
| How to cite this article: Sasidharanpillai S, Reena Mariyath OK, Riyaz N, Binitha MP, George B, Janardhanan AK, Haridas N. Changing trends in leprosy among patients attending a tertiary care institution. Indian J Dermatol Venereol Leprol 2014;80:338-340 |
Sir,
Leprosy elimination was achieved at the global level in December 2000. India announced elimination of leprosy as a public health problem at the national level on January 30, 2006. Leprosy services were decentralized and integrated into the general health system. [1],[2]
At the beginning of 2012, the registered leprosy prevalence globally was 181 941. [3] All areas other than the Americas and African regions reported an increase in the number of new cases detected annually.
In this scenario, we decided to conduct a retrospective data analysis on leprosy among patients who attended the out-patient department (OPD) of our institution during the period January 2003 to December 2012. The study was aimed at detecting any changes in the clinical presentation over the past decade with special reference to grade 2 disability.
Ethical clearance was obtained from the institutional ethics committee. All patients, who attended the OPD with the cardinal features of leprosy were included in the study. Demographic data, details of clinical features including leprosy spectrum and disease complications such as lepra reaction, investigation results and treatment received were collected from individual case records using a pre-set proforma. In cases of relapse, data regarding the previous disease spectrum and treatment received were documented.
The number of patients who had developed grade 2 disability at the time of initial presentation was documented yearly and the grade 2 disability rate of newly detected cases over the years was compared. The results were analyzed using Chi-square test and any change in the disease pattern over the years was noted.
During the study period, 1143 of the 3,911,378 patients who attended the OPD of our institution were diagnosed to have leprosy. A statistically significant decline was noted in new leprosy cases during the study period (P < 0.001). There were 394 females and 749 male patients [Figure - 1]. Borderline tuberculoid leprosy was the commonest type of disease diagnosed throughout the study period. A statistically significant shift toward the lepromatous (LL) spectrum was noted (P = 0.022). The most common age group affected was 16-30 years. A shift towards a higher age group was observed during the study period (P = 0.01).
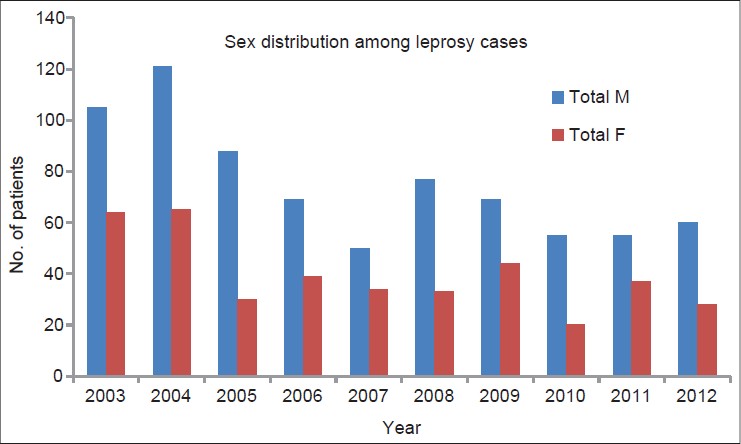 |
| Figure 1: Sex distribution among leprosy cases |
A total of 333 and 810 patients were prescribed paucibacillary (PB) and multibacillary (MB) treatment respectively [Figure - 2]. A statistically significant increase was noted in the number of patients who required MB treatment during the 10 year period (P < 0.001). The study period also witnessed a rise (though statistically insignificant, P = 0.15) in the percentage of smear positive patients [Figure - 3]. A statistically significant (P < 0.001) rise was observed in the rate of new cases with grade 2 disability [Figure - 4].
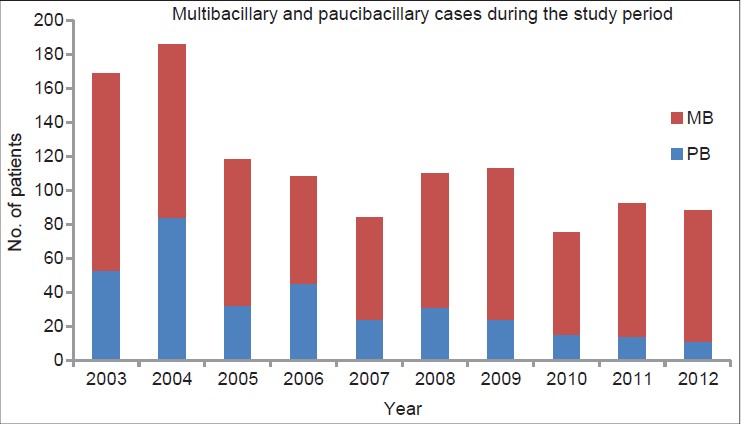 |
| Figure 2: Multibacillary and paucibacillary cases during the study period |
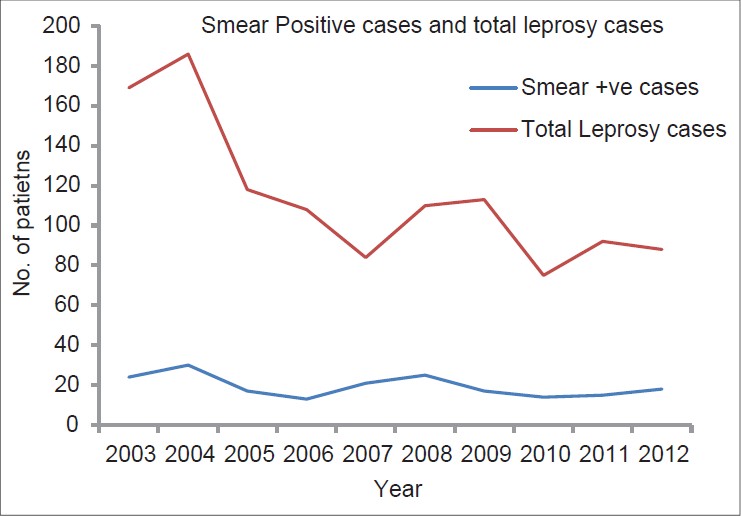 |
| Figure 3: Smear positive cases and total leprosy cases |
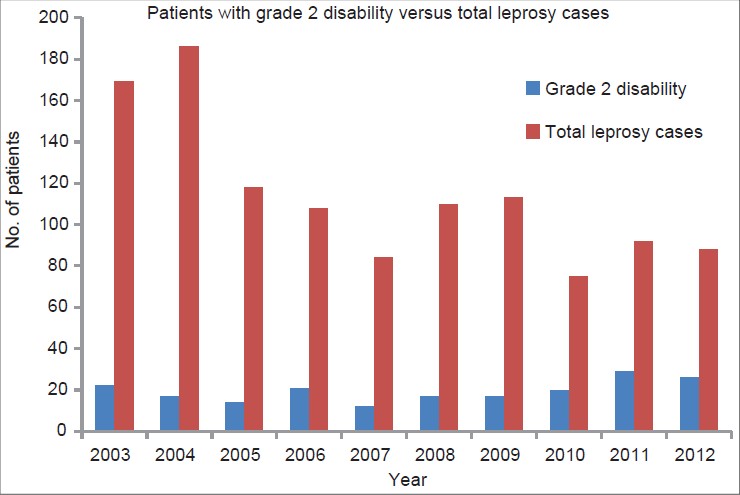 |
| Figure 4: Patients with grade 2 disability versus total leprosy cases |
One hundred and forty five (15.8%) of the 920 patients at risk developed type 1 lepra reaction. Thirty six (18.6%) of 194 borderline lepromatous and lepromatous patients developed type 2 reaction. No significant change was observed in reaction patterns during the 10 year period.
Sixty five (5.7%) of the 1143 patients were cases of relapsed disease of whom 27 had received treatment for paucibacillary disease while 38 had received treatment for multibacillary disease. Six patients had received dapsone monotherapy previously but they could not be considered as relapses as they had not been treated with multidrug therapy.
A significant observation was the increase observed in multibacillary and smear positive cases during the 10 year period, a finding noted in many other recent studies. [4],[5],[6],[7] A delay in diagnosis and initiation of treatment may have been responsible for this finding as well as the significant increase observed in new cases with grade 2 disability during the later years of the study. The latter observation is in concordance with the Malawi study. [5] The post-elimination relaxation in active case detection, might have contributed to these findings.
The major limitation of our study was the dependence on data collected from case records in a tertiary care institution which does not reflect the status of disease in the general population as more severely affected patients are usually referred to a tertiary referral unit. However, we cannot overlook the rise in proportion of patients with extensive disease in recent years.
We need to set up special surveillance units wherever leprosy services have been decentralized to monitor the efficacy of the existing system in early case detection. More epidemiologic studies are required to determine the prevalence of leprosy in the general population.
Acknowledgments
We are grateful to Mr. Gangadharan and Mr. Mohammed Basheer, junior health inspectors. Department of Dermatology, Government Medical College, Kozhikode for their invaluable help in data collection.
| 1. |
Pannikar V. Enhanced global strategy for further reducing the disease burden due to leprosy: 2011-2015. Lepr Rev 2009;80:353-4.
[Google Scholar]
|
| 2. |
Patro BK, Madhanraj K, Singh A. Is leprosy 'elimination' a conceptual illusion? Indian J Dermatol Venereol Leprol 2011;77:549-51.
[Google Scholar]
|
| 3. |
World Health Organisation.Wkly Epidemiol Rec 2012;87:317-28.
[Google Scholar]
|
| 4. |
Sachdeva S, Khan Z, Ansari MA, Amin SS. Leprosy: Down but not out. Trop Doct 2011;41:28-30.
[Google Scholar]
|
| 5. |
Msyamboza KP, Mawaya LR, Kubwalo HW, Ng'oma D, Liabunya M, Manjolo S, et al. Burden of leprosy in Malawi: Community camp-based cross-sectional study. BMC Int Health Hum Rights 2012;12:12.
et al. Burden of leprosy in Malawi: Community camp-based cross-sectional study. BMC Int Health Hum Rights 2012;12:12.'>[Google Scholar]
|
| 6. |
Boggild AK, Correia JD, Keystone JS, Kain KC. Leprosy in Toronto: An analysis of 184 imported cases. CMAJ 2004;170:55-9.
[Google Scholar]
|
| 7. |
Ramos JM, Martínez-Martín M, Reyes F, Lemma D, Belinchón I, Gutiérrez F. Gender differential on characteristics and outcome of leprosy patients admitted to a long-term care rural hospital in South-Eastern Ethiopia. Int J Equity Health 2012;11:56.
[Google Scholar]
|
Fulltext Views
2,812
PDF downloads
2,203





