Translate this page into:
Choroidal melanoma in phacomatosis pigmentovascularis cesioflflammea
Correspondence Address:
Mukai Chen
Department of Dermatology, The First Affi liated Hospital, Sun Yat-Sen University, No. 58, Zhongshan Second Road, Guangzhou, 510080
China
| How to cite this article: Zhou H, Han J, Mao R, Chen M. Choroidal melanoma in phacomatosis pigmentovascularis cesioflflammea. Indian J Dermatol Venereol Leprol 2016;82:339-342 |
Sir,
A 68-year-old Chinese man presented with extensive erythematous and grayish-blue patches since birth. The patches were asymptomatic and had proportionately increased in size over time. He also had a visual field defect in the left eye for 1 month. There was no relevant family history. Dermatological examination revealed extensive bluish-gray macules on cheeks, periorbital area, sclera, trunk and upper limbs [Figure - 1]a,[Figure - 1]b,[Figure - 1]c. In addition, there were purplish red vascular macules on the right side of the chest and back. There was an overlapping of bluish-gray and purplish red macules on the right upper chest and arm. Dermoscopy revealed reticular distribution of pigmented and purple-red skin lesions consisting of pigmented globules, streaks as well as rounded and linear vessels [Figure - 2]. The histological features were diagnostic of dermal melanocytosis with nevus flammeus [Figure - 2]c. Ophthalmic examination showed bilateral bluish black pigmentation in conjunctiva and sclera suggestive of ocular melanocytosis [Figure - 1]b and [Figure - 1]c. Intraocular pressure in the left eye was normal. Magnetic resonance imaging was suggestive of choroidal melanoma which was confirmed on histopathological examination of left eye after enucleation which revealed diffusely distributed atypical cells intertwined with melanin deposits in the choroid [Figure - 3]a,[Figure - 3]b,[Figure - 3]c. Immunohistochemical analysis was positive for HMB45 and S-100 which confirmed the diagnosis of choroidal melanoma. No other abnormality was detected on systemic examination.
 |
| Figure 1: (a) Diffuse ectopic Mongolian spots overlapping with nevus flammeus on the back. (b) Oculardermal melanocytosis. (nevus of Ota) (c) Multiple episcleral patches with heavy pigmentation under slit-lamp |
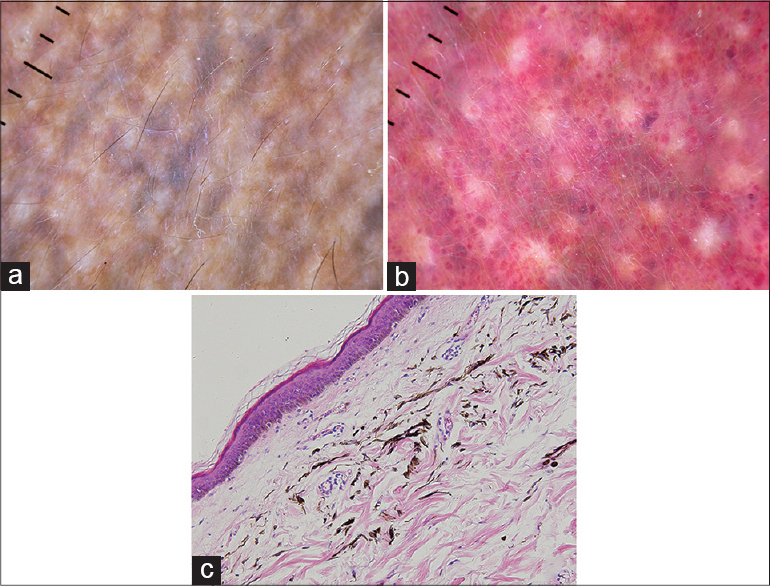 |
| Figure 2: The dermoscopic and histological features of skin lesions. (a) An uneven pigmented net over cheek. (b) Regional red, rounded, globular dots intermingled with pigmented stripes on the chest. (c) Pigmented melanocytes scattered among collagen bundles which confirmed the diagnosis of dermal melanocytosis; numerous subdermal dilated capillaries are consistent with nevus flammeus (H and E, ×200) |
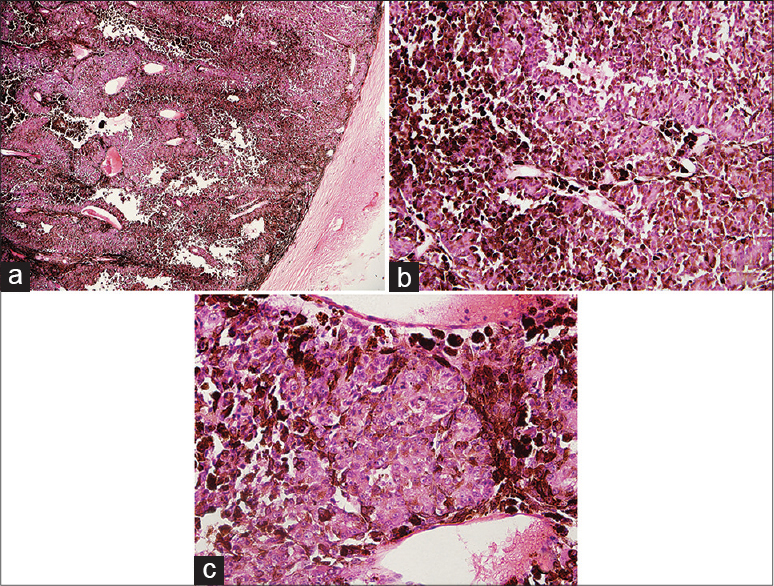 |
| Figure 3: (a) Choroid neoplasms occupying the vitreous chamber (H and E, ×50). (b) Pleomorphic cells intermingled with melanin deposition diffusely distributed in the choroid (H and E, ×200).(c) Marked cytonuclear atypia (H and E, ×400) |
The presence of nevus flammeus, ectopic Mongolian spots and nevus of Ota has been seen in patients with scleral melanocytosis and late onset choroidal melanoma. On this basis, the patient was diagnosed to have phacomatosis pigmentovascularis cesioflammea with adult-onset choroidal melanoma.
Phacomatosis pigmentovascularis, a rare disease characterized by coexisting cutaneous vascular malformations and pigmentary nevus, was first described in 1884 by Ota. Since then, about 250 patients of this condition have been reported, a majority of who were of Asian origin. There are three recognized subtypes of this entity: cesioflammea (blue nevus and nevus flammeus), spilorosea (nevus spilus and a pale pink telangiectatic nevus) and cesiomarmorata (blue spots and cutis marmorata telangiectatica congenita).[1] Cesioflammea is the most common subtype.[2] Its pathogenesis is not well understood. The most accepted hypothesis is that it originates from mosaicism due to a postzygotic somatic mutation occurring after conception and affecting different cell lineages, the so-called “non-allelic twin spotting”.[2] Its diagnosis is primarily clinical. The typical dermoscopic features of nevus flammeus and pigmentary nevus in this patient suggest the importance of dermoscopic examination for diagnosing this disease.
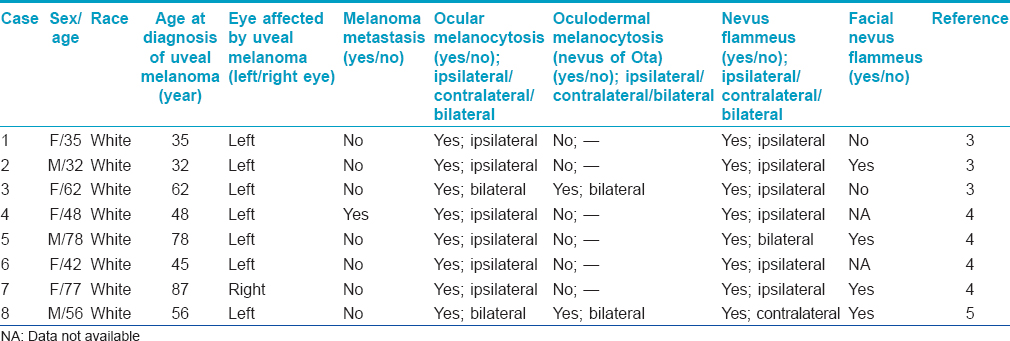
Phacomatosis pigmentovascularis may be associated with systemic involvement including vascular, neurological and ophthalmological involvement.[2] To date, eight patients (5 women, 3 men; median age at onset 52 years, range: 32–87 years) of phacomatosis pigmentovascularis with coexisting choroidal melanoma have been reported, all of who were of Caucasian origin [Table - 1].[3],[4],[5] All cases had ocular melanocytosis while three patients had oculodermal melanocytosis (known as nevus of Ota). This finding supports oculo-dermal melanocytosis as a risk factor for intraocular melanoma; however, we could not exclude the possibility that its etiopathogenesis may have a role in ocular melanoma.[6],[7]
Isolated nevus of Ota is more common in Asians than Caucasians, but the associated uveal melanoma occurs predominantly in Caucasians. In Caucasians, an association between isolated nevus of Ota and uveal melanoma is well acknowledged; in Asian or blacks more than a dozen such cases have been reported.[6],[7] Many researchers believe that dark-skinned individuals with nevus of Ota are also at some risk of developing uveal melanoma.[7]
According to Shields et al., pigmentary nevus in patients with phacomatosis pigmentovascularis may remain confined to the eyes without manifesting any associated skin lesion. Such cases are liable to be missed on naked eye examination. Since, nevus flammeus lesions are discernible to the naked eye, it has often been a necessary precursor to the diagnosis of phacomatosis pigmentovascularis in a vast majority cases. The authors suggest that all patients with nevus flammeus should undergo regular ophthalmic screening to exclude the possibility of coexisting ocular melanocytosis and even uveal melanoma.[4]
In conclusion, although a majority of patients with coexisting phacomatosis pigmentovascularis and choroidal melanoma are of Caucasian origin, the condition may affect Asians. Irrespective of race, patients with phacomatosis pigmentovascularis, especially those of cesioflammea subtype and elderly patients with ocular or oculodermal melanocytosis may develop choroidal melanoma and need regular ophthalmological follow-up.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Happle R. Phacomatosis pigmentovascularis revisited and reclassified. Arch Dermatol 2005;141:385-8.
[Google Scholar]
|
| 2. |
Fernández-Guarino M, Boixeda P, de Las Heras E, Aboin S, García-Millán C, Olasolo PJ. Phakomatosis pigmentovascularis: Clinical findings in 15 patients and review of the literature. J Am Acad Dermatol 2008;58:88-93.
[Google Scholar]
|
| 3. |
Tran HV, Zografos L. Primary choroidal melanoma in phakomatosis pigmentovascularis IIa. Ophthalmology 2005;112:1232-5.
[Google Scholar]
|
| 4. |
Shields CL, Kligman BE, Suriano M, Viloria V, Iturralde JC, Shields MV, et al. Phacomatosis pigmentovascularis of cesioflammea type in 7 patients: Combination of ocular pigmentation (melanocytosis or melanosis) and nevus flammeus with risk for melanoma. Arch Ophthalmol 2011;129:746-50.
[Google Scholar]
|
| 5. |
Krema H, Simpson R, McGowan H. Choroidal melanoma in phacomatosis pigmentovascularis cesioflammea. Can J Ophthalmol 2013;48:e41-2.
[Google Scholar]
|
| 6. |
Chen YC, Chang CH, Hsu SL, Hsu MW, Lee CL. Malignant melanoma of the choroid in the eye with oculodermal melanocytosis of a Chinese woman. Kaohsiung J Med Sci 2010;26:673-8.
[Google Scholar]
|
| 7. |
Sharan S, Grigg JR, Billson FA. Bilateral naevus of Ota with choroidal melanoma and diffuse retinal pigmentation in a dark skinned person. Br J Ophthalmol 2005;89:1529.
[Google Scholar]
|
Fulltext Views
3,620
PDF downloads
2,258





