Translate this page into:
Chromoblastomycosis with a sporotrichoid distribution
Correspondence Address:
Arpita Nibedita Rout
Department of Dermatology, All India Institute of Medical Sciences, Bhubaneswar - 751 019, Odisha
India
| How to cite this article: Rout AN, Sahu K, Sirka CS. Chromoblastomycosis with a sporotrichoid distribution. Indian J Dermatol Venereol Leprol 2019;85:506-508 |
Sir,
An 82-year-old farmer presented with multiple asymptomatic verrucous growths on the left lower limb of 23 years duration. He could not recall any definite history of trauma, before the appearance of the lesions. On examination, there were three discrete verrucous plaques on the left leg [Figure - 1]a. Multiple black spots were seen on the verrucous plaques extending from medial malleolus to lateral malleolus covering the entire anterior aspect of left ankle [Figure - 1]b. Possibility of cutaneous chromoblastomycosis, tuberculosis verrucosa cutis and lichen planus hypertrophicus was considered. There was no regional or generalized lymphadenopathy. Complete blood count, liver function test and renal function test were within normal range. X-ray of the limb did not reveal any abnormality. Examination of the black dots in 10% potassium hydroxide (KOH) preparation did not show any spores. Histopathological examination of the lesion showed hyperkeratosis and papillomatosis with brownish thick-walled copper-penny bodies within mixed inflammatory infiltrates composed of neutrophils and lympho-histiocytes in the superficial dermis [Figure - 2]a and [Figure - 2]b. Culture of the tissue biopsy specimen did not grow any organism. A diagnosis of chromoblastomycosis in sporotrichoid pattern was made based on morphology of the lesions and histopathology findings. The patient was treated with itraconazole 200mg twice daily. There was a marked response after 2 months of treatment [Figure - 3]. He is on regular follow-up and continuing the treatment.
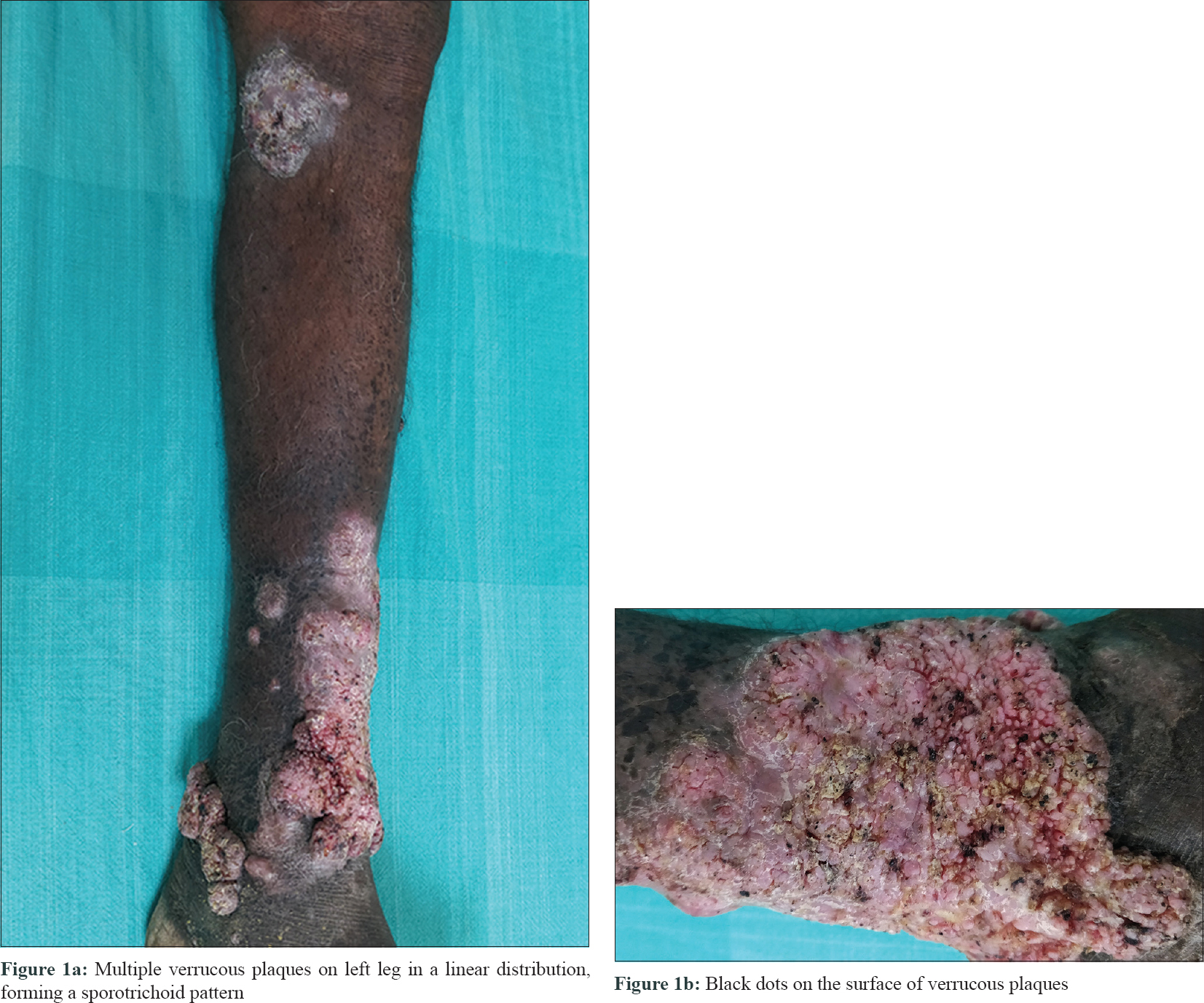 |
| Figure 1 |
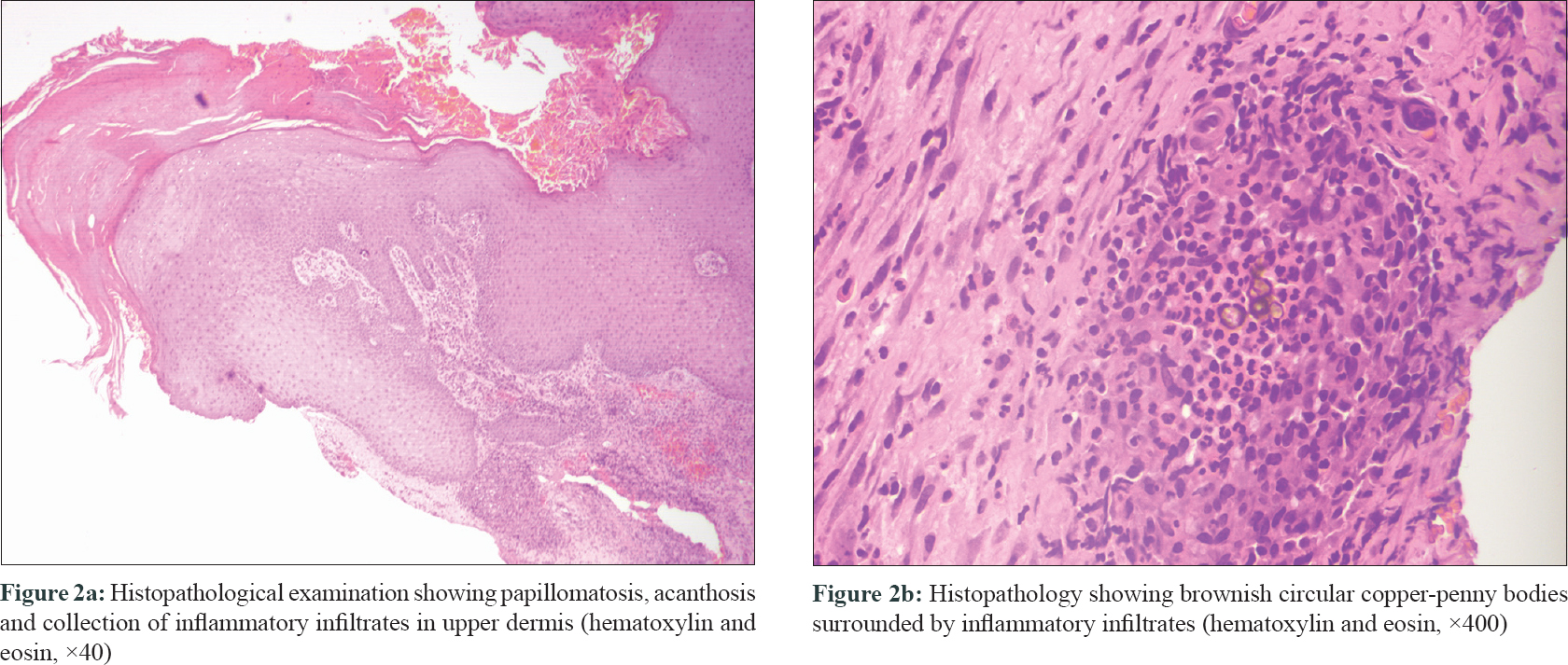 |
| Figure 2 |
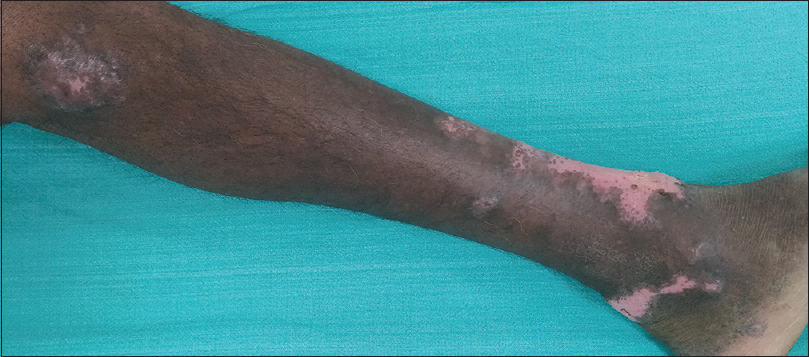 |
| Figure 3: Marked response after 2 months of oral itraconazole 200 mg twice daily |
Chromoblastomycosis is a chronic cutaneous and subcutaneous fungal infection caused by dematiaceous fungi, following traumatic implantation of the organism.[1] It can spread by autoinoculation and rarely through lymphatics.[2],[3]
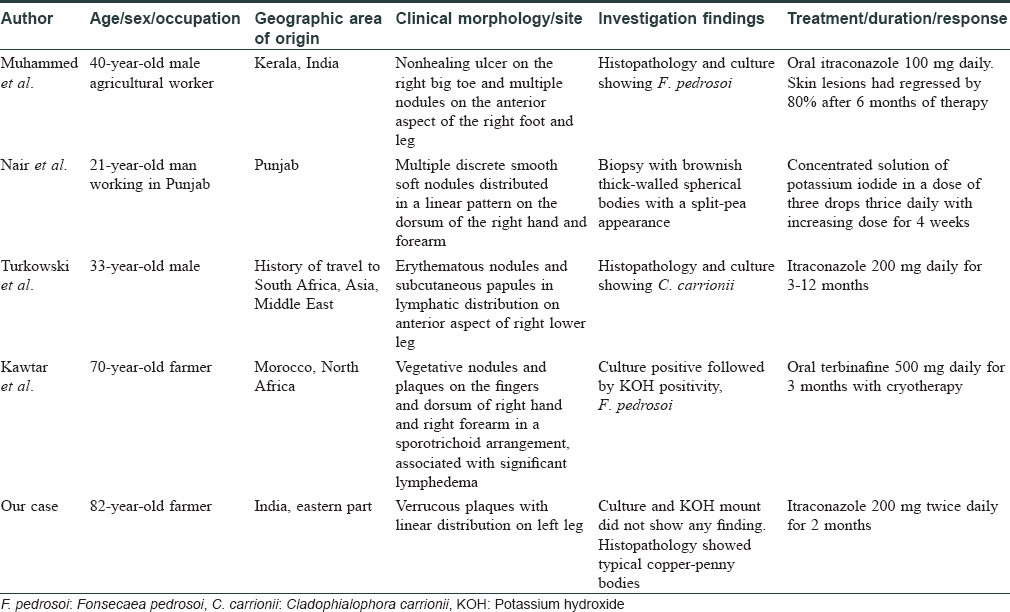
Cutaneous lesions begin as erythematous papules, cauliflower-like nodules or warty growths. They gradually enlarge to form large plaques with brown or black dots on the surface. The most common sites of involvement are the distal limbs. Rarely, it occurs on buttocks, trunk and face.[1] In advanced disease, it can spread to adjoining skin as satellite lesions. Such spread occurs from autoinoculation or transmission via the lymphatic system.[4] In a review of literature, we found four cases of chromoblastomycosis with sporotrichoid distribution.[1],[4],[5],[6]
The sporotrichoid distribution of lesions is seen in sporotrichosis, cutaneous tuberculosis and atypical mycobacterial infection. Chromoblastomycosis can be differentiated from these conditions by identification of the copper-penny bodies, histopathology and culture.
Usually, histopathology reveals acanthosis and may demonstrate pseudo-carcinomatous hyperplasia. Neutrophils and giant cells may be seen infiltrating the epidermis with occasional formation of micro-abscesses. The dermis reveals a granulomatous tissue reaction with a mixed focal or diffuse inflammatory infiltrate consisting of lymphocytes, neutrophils, monocytes, plasma cells, eosinophils and giant cells of the foreign body and Langhans types. The copper-penny bodies may be seen both intracellularly and extracellularly.
The diagnosis of chromoblastomycosis is from microscopic identification of Medlar bodies/fumagoid bodies/muriform bodies/copper-penny bodies/sclerotic bodies on scrapings from the lesion in 20% KOH and/or histological examination of a biopsy specimen and by culture of scrapings or biopsy material.[1] Our patient had multiple nodules in a linear fashion distant from the primary plaque and the diagnosis was confirmed by demonstration of copper-penny bodies in tissue section.
Treatment options include itraconazole, terbinafine and potassium iodide. Our patient was treated with oral itraconazole 200mg twice daily and after 2 months there was good response without any side effects of therapy.
In chromoblastomycosis with satellite lesions, presentation in a sporotrichoid fashion is rare.[1] In our case, based on the morphology, autoinoculation following scratching or minor trauma might have been the cause rather than lymphatic spread. We could not isolate the organism in culture, but the histopathology and response to treatment proved the diagnosis retrospectively. Though isolation of organism in culture is regarded as the gold standard for diagnosis, in resource-poor centers, classical morphology and histopathology can be the pointers to diagnosis. We have compiled and compared the four cases with our case in regards to clinical morphology, site of involvement, investigations and treatment outcomes [Table - 1].[1],[4],[5],[6] We report this case because of its rarity and response to monotherapy with itraconazole.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Muhammed K, Nandakumar G, Asokan KK, Vimi P. Lymphangitic chromoblastomycosis. Indian J Dermatol Venereol Leprol 2006;72:443-5.
[Google Scholar]
|
| 2. |
Queiroz-Telles F, Esterre P, Perez-Blanco M, Vitale RG, Salgado CG, Bonifaz A. Chromoblastomycosis: An overview of clinical manifestations, diagnosis and treatment. Med Mycol 2009;47:3-15.
[Google Scholar]
|
| 3. |
Kondo M, Hiruma M, Nishioka Y, Mayuzumi N, Mochida K, Ikeda S. A case of chromomycosis caused by Fonsecaea pedrosoi and a review of reported cases of dematiaceous fungal infection in Japan. Mycoses 2005;48:221-5.
[Google Scholar]
|
| 4. |
Nair PS, Sarojini PA. Chromoblastomycosis resembling sporotrichosis. Indian J Dermatol Venereol Leprol 1993;59:125-6.
[Google Scholar]
|
| 5. |
Turkowski Y, Aleissa S, Plotnikova N, Tse J, Rosmarin D. Sporotrichoid chromoblastomycosis on right lower leg. J Am Acad Dermatol 2018;79:AB268.
[Google Scholar]
|
| 6. |
Kawtar I, Salim G, Mariame M, Fatimazahra M, Imane T, Salma B, et al. Sporotrichoid chromomycosis. Dermatol Online J 2013;19:20394.
[Google Scholar]
|
Fulltext Views
4,500
PDF downloads
2,126





