Translate this page into:
Clear cell papulosis: A case report and its possible association with epidermal immature dendritic cells
Corresponding Author:
Joong Sun Lee
Department of Dermatology, School of Medicine, Eulji University, 95, Dunsanseo-ro, Seo-gu, Daejeon 35233
South Korea
sun_lee@eulji.ac.kr
| How to cite this article: Kim JH, Jung KE, Koo DW, Lee JS. Clear cell papulosis: A case report and its possible association with epidermal immature dendritic cells. Indian J Dermatol Venereol Leprol 2017;83:379-381 |
Sir,
A17-month-old boy presented with multiple hypopigmented, discrete, round-to-oval maculopapules on the groin and abdomen [Figure - 1] which were initially seen at birth and have been gradually increasing in number and size with age. A skin biopsy revealed mild acanthosis, hyperkeratosis and the occasional presence of benign-appearing pagetoid clear cells having abundant clear cytoplasm with pale, round-to-oval nuclei along the basal layer of the epidermis [Figure - 2] which were slightly larger than those of keratinocytes and showed indistinct nucleoli. There were several S100 positive basal melanocytes; however Fontana-Masson staining confirmed reduced/absent melanization. We performed immune histochemical staining to exclude vitiligo, [Figure - 3]. The clear cells stained positive for D-PAS, cytokeratin7, carcinoembryonic antigen and epithelial membrane antigen and showed relatively decreased positivity for Melan-A and HMB-45 and negative for S100 protein. Interestingly, there was a prominent increase in the number of S100 protein-positive dendritic cells in the epidermis. Additional staining for CD1a, confirmed them to be immature dendritic cells.
 |
| Figure 1 |
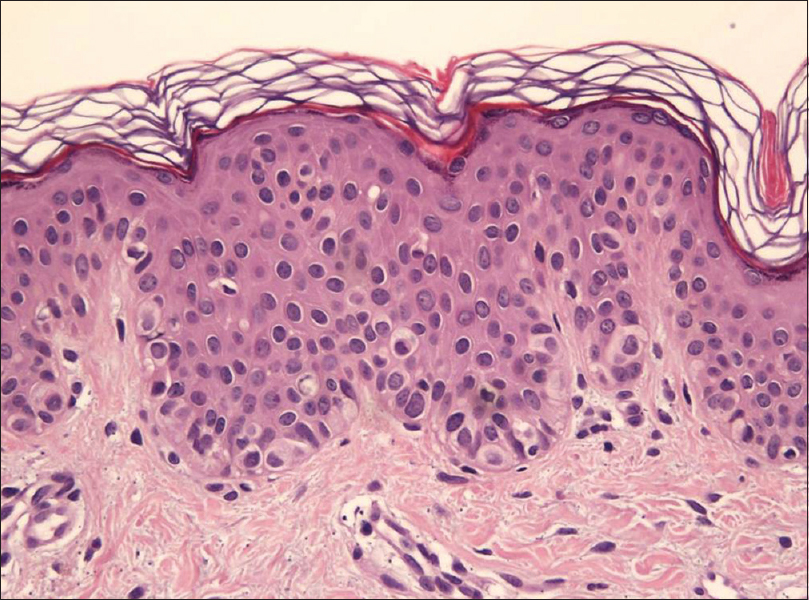 |
| Figure 2: Skin biopsy done from the abdomen. H and E stained specimen revealing mild acanthosis, hyperkeratosis and the presence of some benign-appearing pagetoid clear cells showing abundant clear cytoplasm with pale, round-to-oval nucleus, along the basal layer of the epidermis. No mitotic figures were identified (H and E, ×200) |
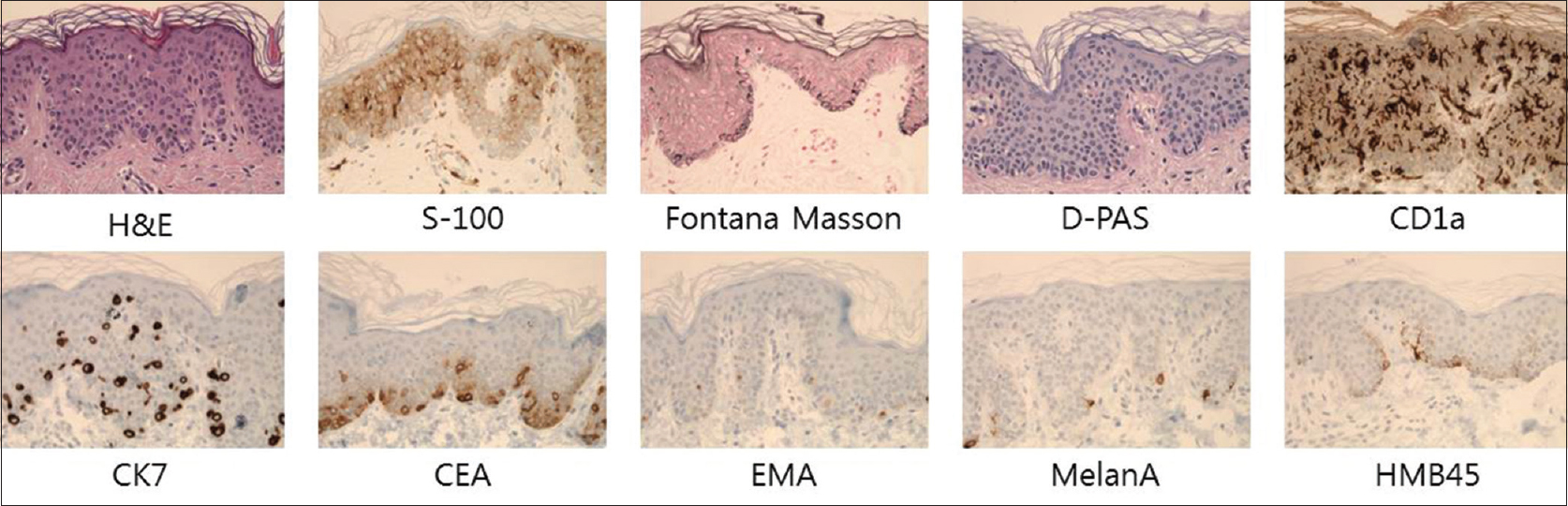 |
| Figure 3: The distribution of clear cells in the lesional skin. Immunohistochemical staining for D-PAS, cytokeratin7, carcinoembryonic antigen and epithelial membrane antigen show positivity with clear cells (×400). There is a prominent increase in the number of S100 protein and CD1a-positive dendritic cells in the epidermis (×400). Reduced to absent melanin pigmentation in the lesion was confirmed by Fontana-Masson stain (×400). The clear cells show relatively decreased positivity for Melan A and HMB45 (×400) |
Clear cell papulosis is a recently identified entity, characterized by female predominance, racial predilection for Asians and genetic predisposition as evidenced by reports of cases in several siblings.[1],[2],[3],[4] It usually undergoes spontaneous regression after growth; making adult cases rare.[1],[2] The pathophysiology of clear cell papulosis is still unknown, but Kim et al. have suggested that the clear cells of clear cell papulosis may have originated from eccrine secretory cells,[3] as these cells are stained with IKH-4, carcinoembryonic antigen and CAM 5.2, but not with lysozyme. Histopathologically, these clear cells can be confused with melanocytes, Langerhans cells or Toker cells.[1],[2],[3],[4] Clear cells of clear cell papulosis are typically scattered among basal keratinocytesor in the supra basal layer, as a single cell or in groups. They are round, having a benign appearance being larger than the neighboring keratinocytes and are characterized by pale, round-to-oval nuclei with ample, clear cytoplasm. Mitotic figure or pleomorphism have not been reported in most cases.[1],[2] If clear cell papulosis is clinically suspected, immunohistochemical studies may help in making a correct diagnosis. To date, all cases of clear cell papulosis have been reported to stain positive with mucin, carcinoembryonic antigen, CAM5.2, cytokeratin7, colloidal iron, cytokeratin AE1/AE3, epithelial membrane antigen and gross cystic disease fluid protein-15 and negative for the S100 protein.[1],[2],[3] The white lesions demonstrated conspicuous reduction or absence of epidermal melanization and a decreased number of basal melanocytes.[4] Chen et al. suggested it could be related to a dysfunction of melanocytes in clear cell papulosis.[4] Some authors have proposed a relationship between clear cell papulosis and extramammary Paget's disease as pagetoid clear cells are present in the epidermis in both conditions. Despite the pathogenesis of extramammary Paget's disease being controversial,[4] tadpole-shaped clear cells have been found at the lesional periphery in a depigmented variant of extramammary Paget's disease which are similar to the clear cells of clear cell papulosis.[4] Due to the milk line distribution and similarity to pagetoid cells, some researchers have suggested that clear cells of clear cell papulosis may give rise to cutaneous Paget's disease.[1],[4] In addition, several studies suggest that clear cell papulosis might be a precursor of extramammary Paget's disease by means of a transformed Toker cell (Her2/neu, p53 expression), but no direct evidence has been reported yet.[2],[4] Recently, a large study about clear cell papulosis by Tseng et al. demonstrated that there is no direct relationship between clear cell papulosis and mammary Paget's disease/extra mammary Paget's disease.[1]
Our case of clear cell papulosis had a distinctive congenital onset showing the characteristic epidermal presence of S100 protein and CD1 a-positive dendritic cells. Brunhuber et al. found that S100 protein-positive dendritic cells show direct contact with cytokeratin7-positive Paget cells.[5] They suggested that tumor fragment-loaded dendritic cells may be able to cross prime and activate lymphocytes for antitumor immunoreactions.[5] Regarding the possible relationship between clear cell papulosis and Paget'sdisease, we can infer that dendritic cells may play an important role in the pathophysiology of clear cell papulosis. Moreover, in most cases, Paget's disease is accompanied by an outstanding infiltration of mixed inflammatory cells in the tumor-surrounding dermal tissue which is not apparent in clear cell papulosis.[5] It might be a distinctive feature of clear cell papulosis, suggesting that it is not a precancerous condition.
To conclude, clear cell papulosis has a benign histologic appearance though it is similar to Toker cells and Paget cells.[2],[4] Our rare case of congenital clear cell papulosis suggests that immature epidermal dendritic cells may play a role in the pathogenesis of clear cell papulosis. Further studies are needed to elucidate more details about this uncommon condition.
Financial support and sponsorship
This paper was supported by Eulji University, Daejeon, South Korea.
Conflicts of interest
There are no conflicts of interest.
| 1. | Tseng FW, Kuo TT, Lu PH, Chan HL, Chan MJ, Hui RC. Long-term follow-up study of clear cell papulosis. J Am Acad Dermatol 2010;63:266-73. [Google Scholar] |
| 2. | Wysong A, Sundram U, Benjamin L. Clear-cell papulosis: A rare entity that may be misconstrued pathologically as normal skin. Pediatr Dermatol 2012;29:195-8. [Google Scholar] |
| 3. | Kim YC, Mehregan DA, Bang D. Clear cell papulosis: An immunohistochemical study to determine histogenesis. J Cutan Pathol 2002;29:11-4. [Google Scholar] |
| 4. | Chen YH, Wong TW, Lee JY. Depigmented genital extramammary Paget's disease: A possible histogenetic link to Toker's clear cells and clear cell papulosis. J Cutan Pathol 2001;28:105-8. [Google Scholar] |
| 5. | Brunhuber T, Haybaeck J, Schäfer G, Mikuz G, Langhoff E, Saeland S, et al. Immunohistochemical tracking of an immune response in mammary Paget's disease. Cancer Lett 2008;272:206-20. [Google Scholar] |
Fulltext Views
3,885
PDF downloads
1,641





