Translate this page into:
Clinical characteristics of acquired ungual fibrokeratoma
Corresponding Author:
Hyun Jeong Park
Department of Dermatology, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, 222 Banpo-daero, Seocho-gu, Seoul 137-701
Republic of Korea
hjpark@catholic.ac.kr
| How to cite this article: Hwang S, Kim M, Cho BK, Park HJ. Clinical characteristics of acquired ungual fibrokeratoma. Indian J Dermatol Venereol Leprol 2017;83:337-343 |
Abstract
Background: Acquired ungual fibrokeratomas are uncommon fibrous tissue tumors located in the ungual area. Though there are many reports of this entity, only some reports have reviewed the clinical features of the tumor.Aims: The aim of this study was to clarify the clinical characteristics of acquired ungual fibrokeratomas.
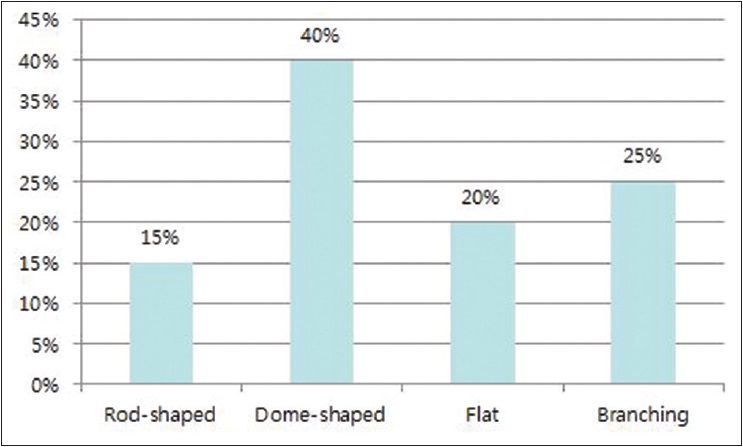
Methods: We reviewed twenty patients who were treated surgically at our clinic from 2003 to 2014 for acquired ungual fibrokeratomas confirmed on histopathological examination. Our study was conducted by retrospective analysis of charts, clinical pictures and patient records. Cases of tuberous sclerosis were not included.
Results: Acquired ungual fibrokeratomas occurred on toenails in 16 (80%) patients and on fingernails in 4 (20%) patients. Periungual lesions were noted in 15 (75%) patients followed by intraungual lesions in 4 (20%) patients and subungual lesions in 1 (5%) patient. A longitudinal groove was observed in 80% of patients. Surgical resection was performed in all cases for both medical and cosmetic reasons. After excision, recurrence occurred in three cases.
Limitations: This was a retrospective study of a limited number of patients.
Conclusions: Acquired ungual fibrokeratomas occurred more commonly on toenails than on fingernails and were located in the periungual area in most patients. A longitudinal groove in the nail plate was a frequent finding. Surgical resection led to medical and cosmetic improvement with a recurrence in 3 (15%) patients.
Introduction
Acquired ungual fibrokeratoma is an uncommon benign fibrous tissue tumor located in the nail area. The term was first coined by Cahn in 1977.[1] He postulated that this was the same as the garlic clove fibroma which was first identified by Steel in 1965.[1],[2] Acquired ungual fibrokeratomas usually present as asymptomatic, solitary, smooth, dome-shaped or finger-like, flesh-colored papules. Accompanying nail deformities include a longitudinal groove and trachyonychia. There are many reports of acquired acral fibrokeratomas but only a few review their clinical features. This study looked at the clinical features, accompanying nail changes, response to treatment and follow-up in twenty patients with acquired ungual fibrokeratomas.
Methods
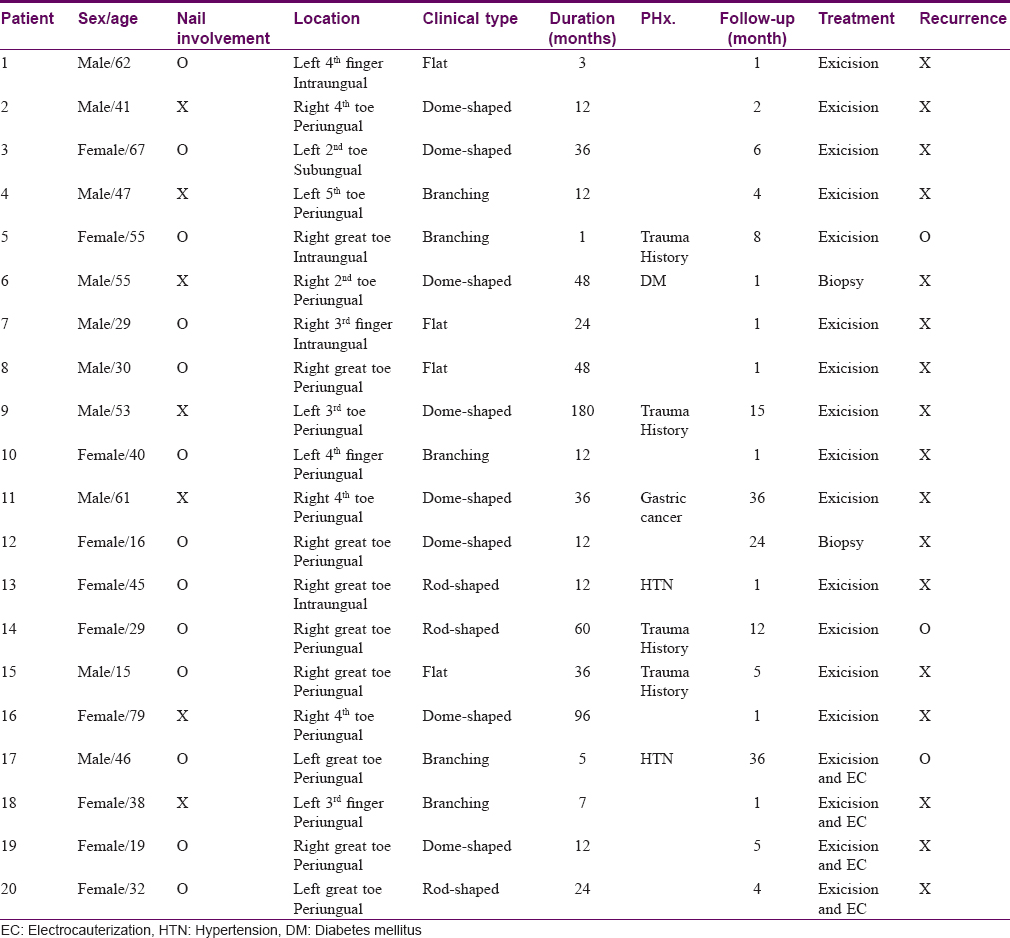
Twenty patients who were treated surgically at our clinic for acquired ungual fibrokeratomas from 2003 to 2014 were included. We analysed patient charts, clinical pictures and patient records (which included sex, age, duration of illness, trauma history and history of previous treatment). Cases with tuberous sclerosis were not included. Acquired ungual fibrokeratomas were classified into four morphological types: Rod-shaped, dome-shaped, flat and branching [Figure - 1]. They were also classified based on location as periungual, subungual and intraungual (”dissecting ungual”) [Figure - 2]. All patients were treated by complete surgical excision and the diagnosis confirmed by histopathologic examination of all excised lesions.
 |
| Figure 1 |
 |
| Figure 2 |
Results
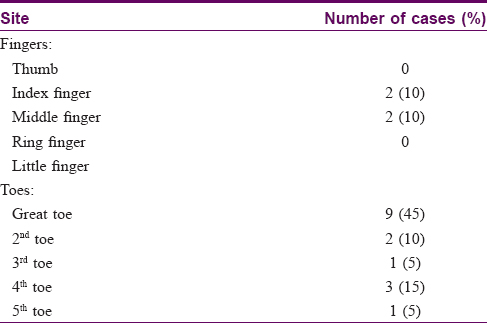
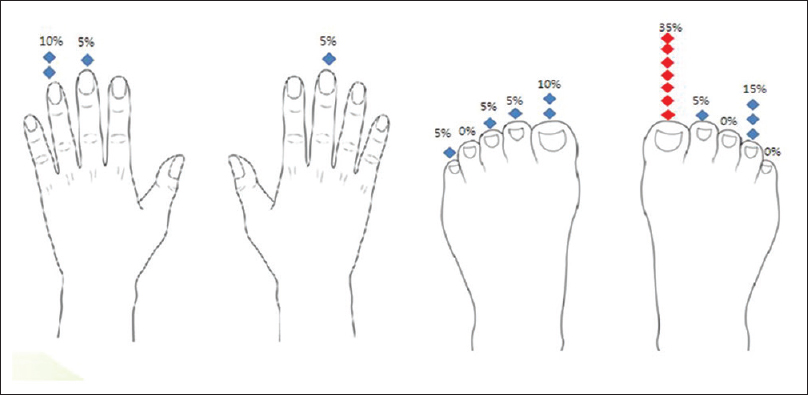
The main clinical data are shown in [Table - 1] and [Figure - 3]. Patient details are listed in [Table - 2].
 |
| Figure 3: Distribution of acquired ungual fibrokeratoma of nail unit of fingers and toenails |
The patients ranged in age from 15 to 79 years with a mean of 41.2 years. The male to female ratio was 10:10. Almost all patients (17/20) remembered when the lesion first appeared. The average delay for seeking medical advice was 28 months. Symptom duration was 40.4 months on average. A high proportion of patients were in their 40s (5/20). Three patients had lesion onset in childhood. Associated diseases observed included hypertension (2/20), diabetes mellitus (1/20) and gastric cancer (1/20). Four patients (20%) had a history of trauma with the lesion developing 2.5 years later on average.
All patients had a single lesion. Toenails (16/20, 80%) were involved more commonly than fingernails (4/20, 20%), most commonly the right great toenail. Tumors presented as asymptomatic, skin-colored, hyperkeratotic papules and the base of each lesion was surrounded by an epidermal collarette. In order of decreasing frequency, lesions were dome-shaped (8/20, 40%), branching (5/20, 25%), flat (4/20, 20%) and rod-shaped (3/20, 15%) [Figure 4a]. Distribution was periungual (15/20, 75%), intraungual (4/20, 20%) or subungual (1/20, 5%) [Figure 4b]. A longitudinal groove was the most commonly associated nail deformity (16/20, 80%). Also trachyonychia (8/20, 40%), chromonychia (4/20, 20%), onycholysis(4/20, 20%), subungual hyperkeratosis (3/20, 15%), and dissected nail plates (2/20, 10%) were observed.
 |
| Figure 4a: Clinical manifestation of AUFK |
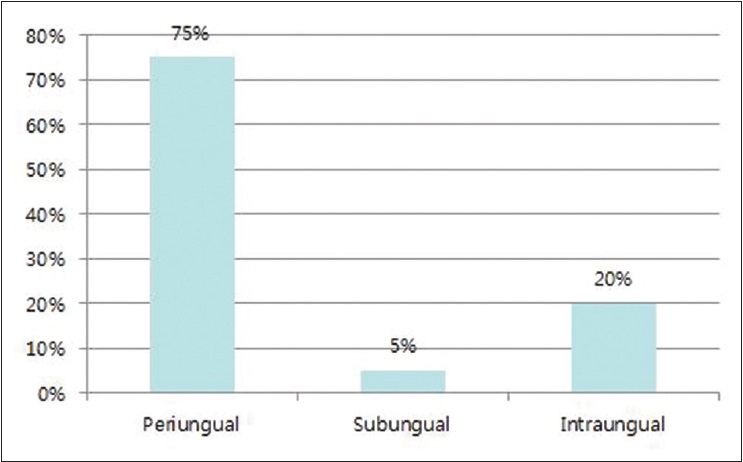 |
| Figure 4b: Distribution of AUFK of nail unit |
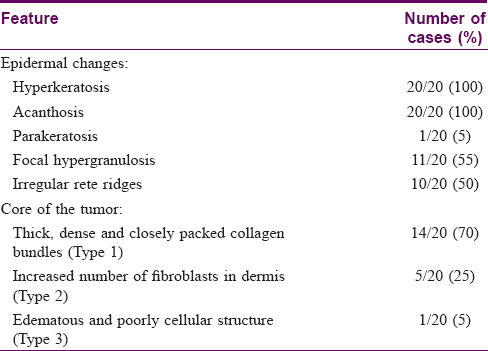
The histopathological findings in our cases are summarized in [Table - 3].
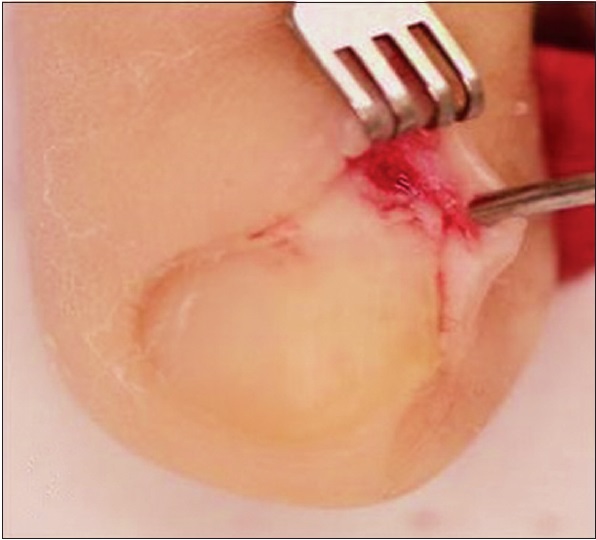
All patients were treated by surgical excision [Figure 5a], [Figure 5b], [Figure 5c], [Figure 5d]. The mean post-excision follow-up period was 8.6 months. After excision, recurrence occurred in three cases, all of whom gave a history of trauma preceding the appearance of the tumors. During follow-up, only one patient had residual scarring around the proximal nail fold and almost all patients were satisfied with the postoperative result as they regained normal nail contours.
 |
| Figure 5a: Oblique incisions were made at corners of the perionychium |
 |
| Figure 5b: Oblique incisions were made at corners of the perionychium |
 |
| Figure 5c: The proximal nail fold was retracted to expose the nail matrix by skin hooks |
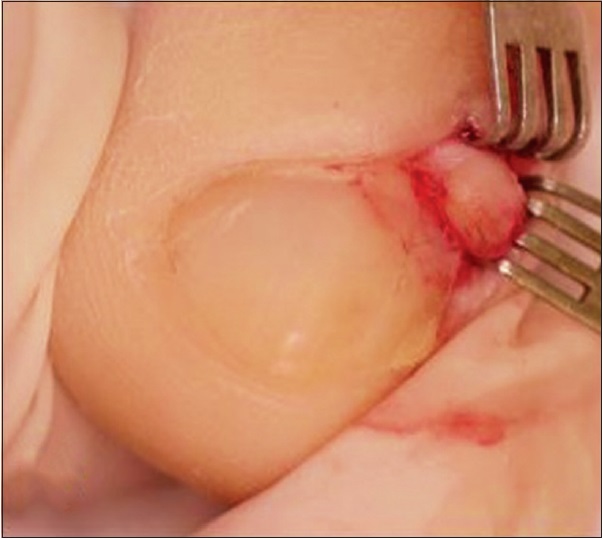 |
| Figure 5d: The whole tumor was exposed and excised with its basal attachment |
Discussion
Acquired periungual fibrokeratomas are rare, benign, fibrous, hyperkeratotic tumors.[1],[3] They usually present as lesions that emerge from the proximal nail fold or sometimes from the nail bed.[4],[5] Cahn proposed the term “acquired periungual fibrokeratoma” because these lesions were thought to be histologically identical to acquired digital fibrokeratomas.[1] Although acquired periungual fibrokeratoma is considered a topographical variant of acquired digital fibrokeratoma, it has a unique “garlic clove” shape.[2],[6]
Including the word “acquired” in the terminology of this unusual tumor leads one to believe that there is a precipitating factor. However, the etiology of acquired ungual fibrokeratoma is still unknown. Hare and Smith proposed that trauma is involved, while Nemeth and Penneys reported that factor XIIIa-positive dermal dendritic cells play an important role in the regulation of collagen synthesis.[7],[8],[9],[10] A traumatic origin has been suggested because acquired ungual fibrokeratomas occur most frequently on the fingers and toes.[11] However, a history of injury is usually present in only a few cases and in only four of our patients, although other patients might not have noticed minor trauma. In our study too, the middle and ring fingernails as well as the great and fourth toenails were more commonly affected and these are sites likely to be exposed to trauma or infection, supporting the above hypothesis.[7],[8] Trauma may be a trigger due to damage to the nail matrix but further research is needed.
Acquired ungual fibrokeratomas usually present as asymptomatic, firm, smooth, flesh-colored papules protruding laterally on the nail plate from beneath the cuticle of the proximal nail fold. Verruca vulgaris, a supernumerary digit, Koenen's tumor of tuberous sclerosis, pyogenic granuloma, eccrine poroma, cutaneous horn, epidermoid cyst, acrochordons and neurofibromas must be included in the differential diagnosis of acquired ungual fibrokeratoma.[8],[11],[12],[13]
The histopathologic appearance of an acquired ungual fibrokeratoma is distinct. Histopathologic findings include hyperkeratosis, acanthosis, focal hypergranulosis and irregular rete ridge elongation in the epidermis. The core of the tumor consists of thickened collagen in the dermis oriented parallel to the long axis of the lesion [Figure - 6].[1] In 1985, Kint et al. classified acquired digital fibrokeratomas into three histologic subtypes.[14] In all three, the epidermis is acanthotic and hyperkeratotic. In the first variant, tumor cores are composed of thick, dense, closely packed and irregularly arranged collagen bundles. The second variant shows an increase in grouped fibroblasts and reduced elastic fibers. The third variant is composed of a poorly cellular and edematous structure with completely absent elastic tissue. When this classification was applied to our patients, the first variant was found to be the most common (70%) followed by the second (25%) and third (5%) variants [Table - 3], consistent with the above report by Kint et al.
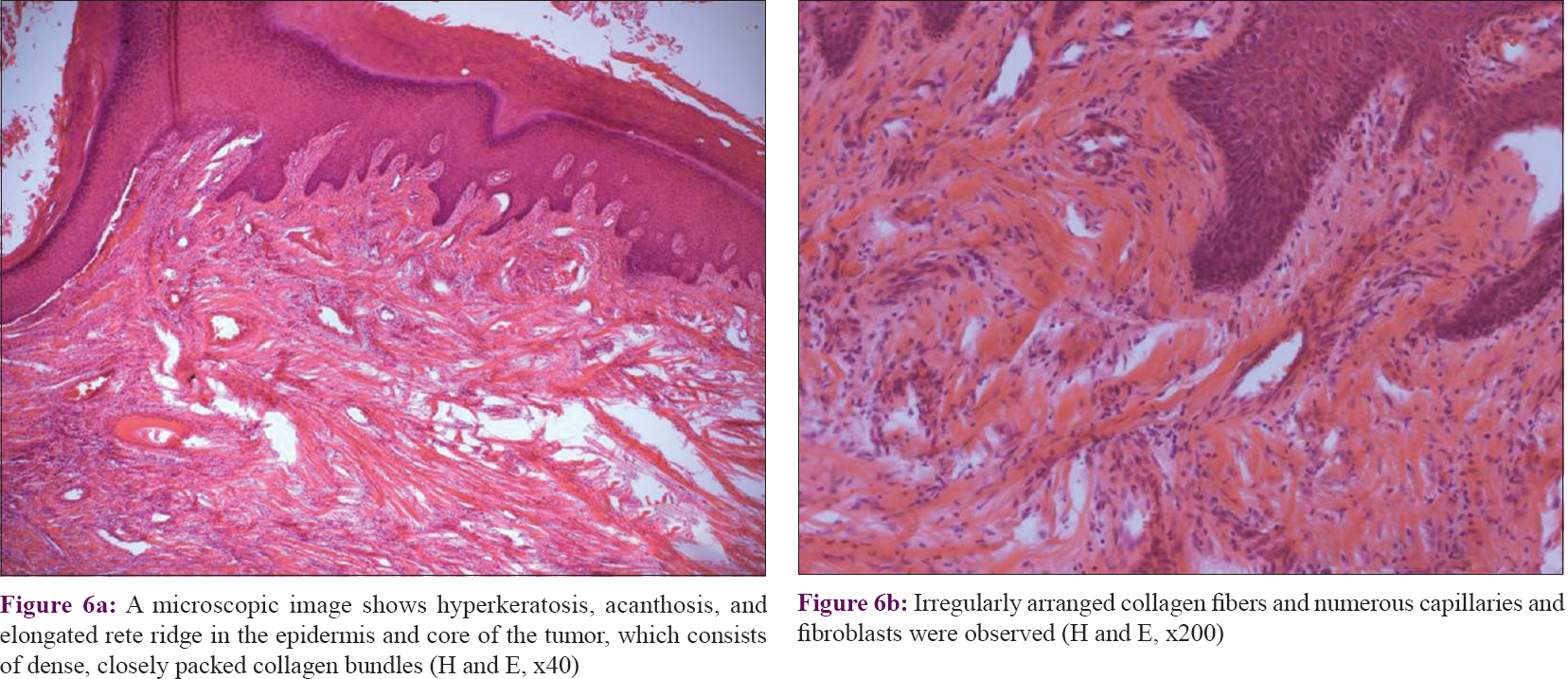 |
| Figure 6(H and E, x40) |
Kint et al. divided acquired ungual fibrokeratomas into two types based on appearance, dome-shaped and finger-like.[14] However, we observed more diverse morphologies and classified them into four subtypes: Rod-shaped, dome-shaped, flat and branching. Rod-shaped acquired ungual fibrokeratomas are smooth and trigonal; dome-shaped lesions curving and round; flat ones have a horizontal surface without a slope and branching acquired ungual fibrokeratomas appear to be divided into two or more parts. Kim et al. classified acquired ungual fibrokeratoma into four clinical types viz., pine-pit-like, dome-shaped, finger-like and chicken's foot-like.[15] Although there are differences in classification, Kim et al. found that dome-shaped acquired ungual fibrokeratomas were the most common clinical type, as in our study. In this study accompanying nail abnormalities include longitudinal grooving, trachyonychia, chromonychia, subungual hyperkeratosis, onycholysis and dissected nail plates. Acquired ungual fibrokeratomas should be considered in the differential diagnosis of periungual tumors with a longitudinal nail groove. The groove is thought to be due to the fibrokeratoma originating from the underside of the proximal nail fold, compressing the nail matrix.[14]
Acquired ungual fibrokeratomas do not spontaneously regress.[12] They should be excised when they cause symptoms or significant cosmetic problems. The preferred treatment is total excision because superficial removal usually results in recurrence.[16] Various surgical techniques can be used to resect these tumors depending on their size and location. Usually, the tumor is incised around its base and dissected from the bone. If a lesion is beneath the nail plate, partial or total removal of the nail is required first. Lesions above the nail plate however, can be removed by shaving followed by phenolization, carbon-dioxide laser vaporization or surgical resection after lifting the proximal nail fold as a banner flap.[17],[18],[19] During the procedure, the germinal matrix should be preserved by careful dissection along the undersurface of the tumor and the tumor should be completely excised with its basal attachment.[20],[21] To minimize the risk of recurrence, we recommend careful elevation of the nail plate and retraction of the proximal nail fold to expose the whole tumor and surrounding nail matrix, avoiding additional injury to the nail matrix.
Our study had some limitations. Apart from being a retrospective study with inevitable biases, we only had a limited number of patients. Further studies are needed to look into the etiology of acquired ungual fibrokeratomas.
Acknowledgment
This study was supported by the Basic Science Research Program and Creative Materials Discovery Program through the National Research Foundation of Korea (NRF) which is funded by the Ministry of Education, Science and Technology and the Ministry of Science, Information and Communications Technologies (ICT) and Future Planning (2015R1C1A2A01055073, 2016M3D1A1021387).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. | Cahn RL. Acquired periungual fibrokeratoma. A rare benign tumor previously described as the garlic-clove fibroma. Arch Dermatol 1977;113:1564-8. [Google Scholar] |
| 2. | Steel HH. Garlic-clove fibroma. JAMA 1965;191:1082-3. [Google Scholar] |
| 3. | Verallo VV. Acquired digital fibrokeratomas. Br J Dermatol 1968;80:730-6. [Google Scholar] |
| 4. | Saito S, Ishikawa K. Acquired periungual fibrokeratoma with accessory germinal matrix. J Hand Surg Br 2002;27:549-55. [Google Scholar] |
| 5. | Hashiro M, Fujio Y, Tanaka M, Yamatodani Y. Giant acquired fibrokeratoma of the nail bed. Dermatology 1995;190:169-71. [Google Scholar] |
| 6. | Yasuki Y. Acquired periungual fibrokeratoma – A proposal for classification of periungual fibrous lesions. J Dermatol 1985;12:349-56. [Google Scholar] |
| 7. | Hare PJ, Smith PA. Acquired (digital) fibrokeratoma. Br J Dermatol 1969;81:667-70. [Google Scholar] |
| 8. | Nemeth AJ, Penneys NS. Factor XIIIa is expressed by fibroblasts in fibrovascular tumors. J Cutan Pathol 1989;16:266-71. [Google Scholar] |
| 9. | Cerio R, Griffiths CE, Cooper KD, Nickoloff BJ, Headington JT. Characterization of factor XIIIa positive dermal dendritic cells in normal and inflamed skin. Br J Dermatol 1989;121:421-31. [Google Scholar] |
| 10. | Cerio R, Spaull J, Oliver GF, Jones WE. A study of factor XIIIa and MAC 387 immunolabeling in normal and pathological skin. Am J Dermatopathol 1990;12:221-33. [Google Scholar] |
| 11. | Altman DA, Griner JM, Faria DT. Acquired digital fibrokeratoma. Cutis 1994;54:93-4. [Google Scholar] |
| 12. | Berger RS, Spielvogel RL. Dermal papule on a distal digit. Acquired digital fibrokeratoma. Arch Dermatol 1988;124:1559-60, 1562-3. [Google Scholar] |
| 13. | Vinson RP, Angeloni VL. Acquired digital fibrokeratoma. Am Fam Physician 1995;52:1365-7. [Google Scholar] |
| 14. | Kint A, Baran R, De Keyser H. Acquired (digital) fibrokeratoma. J Am Acad Dermatol 1985;12(5 Pt 1):816-21. [Google Scholar] |
| 15. | Kim JM, Cho HH, Kin WJ, Mun JH, Song M, Kim HS, et al. Clinical characteristics of acral fibrokeratoma. Korean J Dermatol 2014;52:535-9. [Google Scholar] |
| 16. | Shelley WB, Phillips E. Recurring accessory “fingernail”: Periungual fibrokeratoma. Cutis 1985;35:451-4. [Google Scholar] |
| 17. | Mazaira M, del Pozo Losada J, Fernández-Jorge B, Fernández-Torres R, Martínez W, Fonseca E. Shave and phenolization of periungual fibromas, Koenen's tumors, in a patient with tuberous sclerosis. Dermatol Surg 2008;34:111-3. [Google Scholar] |
| 18. | Berlin AL, Billick RC. Use of CO2 laser in the treatment of periungual fibromas associated with tuberous sclerosis. Dermatol Surg 2002;28:434-6. [Google Scholar] |
| 19. | Vazquez-Doval FJ. Surgery of the nail region. In: Atlas of nail diseases. ESMONpharma; 2008. p. 112-3. [Google Scholar] |
| 20. | Lee CY, Lee KY, Kim KH, Kim YH. Total excision of acquired periungual fibrokeratoma using bilateral proximal nail fold oblique incision for preserving nail matrix. Dermatol Surg 2010;36:139-41. [Google Scholar] |
| 21. | Yé lamos O, Alegre M, Garcé s JR, Puig L. Periungual acral fibrokeratoma: Surgical excision using a banner flap. Actas Dermosifiliogr 2013;104:830-2. [Google Scholar] |
Fulltext Views
13,767
PDF downloads
2,799





