Translate this page into:
Clinicohistopathological correlation of leprosy
Correspondence Address:
Amrish N Pandya
702/B, Amrutdhara Apartments, Opposite St. Xavier's School, Ghod Dod Road, Surat - 395 001
India
| How to cite this article: Pandya AN, Tailor HJ. Clinicohistopathological correlation of leprosy. Indian J Dermatol Venereol Leprol 2008;74:174-176 |
Sir,
Leprosy is one of the major public health problems of the developing countries. The principle of reducing the load of infection in society, to break the chain of infection, is the cornerstone of leprosy control work today. Clinical judgment and skin smear examination is required for early diagnosis and adequate treatment to make the patient noninfectious. But in some early and borderline cases of leprosy, it is difficult to label only on clinical basis. So, histopathological examination is a must for confirmation of diagnosis in doubtful cases of leprosy. Moreover, correct labeling of paucibacillary and multibacilllary cases is a prerequisite. No multibacilllary case should be treated as paucibacillary case. So, clinicohistopathological correlation of leprosy cases assumes a pivotal role for early diagnosis and for proper labeling of a case.
Fifty skin biopsies, of clinically suspected leprosy cases, were stained by Haematoxylin and Eosin and Ziehl Neelsen stain methods. The Ridley and Jopling classification was followed in both clinical and histopathological diagnoses. We also included indeterminate and histoid types of leprosy for analysis. The data pertaining to age, sex, clinical and histopathological classification of the type of leprosy were collected and analyzed. In analyzing the histopathology of a lesion, special attention was given to the following features, viz., invasion of the epidermis with or without erosion, involvement of the sub-epidermal zone, character and extent of granuloma, density of lymphocytic infiltrate, epithelioid cells and other cellular elements, nerve involvement and the presence of M. leprae .
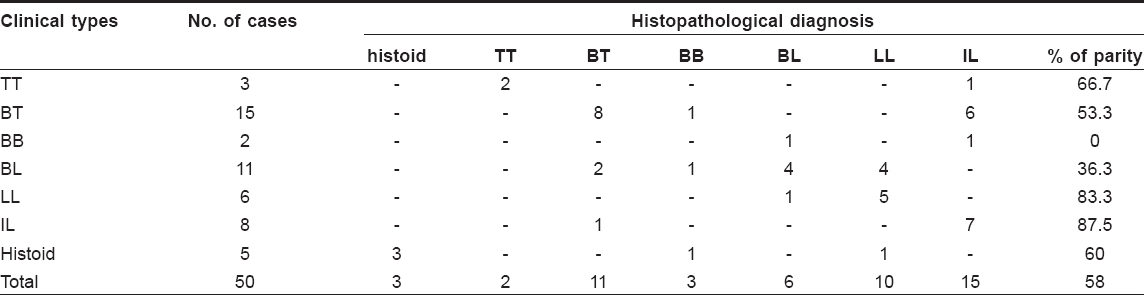
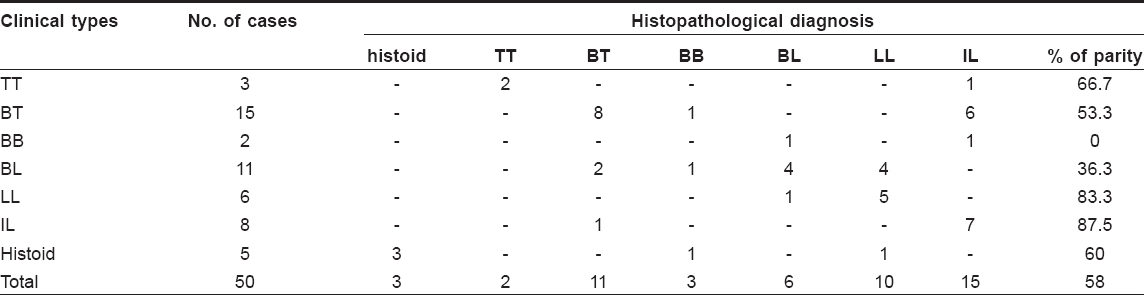
Results of our study are mentioned in [Table - 1].
When M. leprae enters a person with sufficient cell-mediated immunity (CMI) against it, the bacilli will be destroyed. If the CMI is slightly impaired, some bacilli will multiply and a lesion will develop. Depending upon the degree of the immunity, more apparent clinical and histopathological features of the various types of leprosy may gradually develop. On histopathological study, the type of the granuloma cell serves to provide the spectrum of leprosy in two, with epithelioid cells extending from TT to BB and macrophages occurring in BL and LL.
Lymphocytes are the most numerous of all in BL, a few in BB and most scanty in LL. Erosion of epidermis by granuloma is often a valuable sign for the identification of TT. Infiltration of the subepidermal zone is almost invariable in TT, but inconstant in BT. This zone is almost clear, unless compressed by an expanding granuloma, in BB, BL and LL. In the present study, a complete parity between clinical type and histological type was noted in 58% cases [Table - 1].
Ridley and Jopling in their study of 82 cases found complete agreement between clinical and histological types in 56 patients (68.3%). [2] Kar et al. in their study observed total parity in 70%. They also observed highest parity in stable poles, i.e. TT (87.5%) and LL (71.4%), followed by IL (81.2%), BT (60.9%), BB (54.5%) and BL (53.8%). [3] Kalla et al. in a study of 736 patients observed highest parity in LL and TT group (76.7% and 75.6%), respectively, followed by BT (44.2%), BL (43.7%) and BB (37.0%). [4] Jerath and Desai in a study of 130 cases found complete agreement in 89 cases (68.5%). The figures for individual groups were TT (74.5%), BT (64.7%), BB (53.8%) and BL (28.5%), LL (61.5%) and indeterminate leprosy (88.8%). [5] Considering the data of present study and other comparative studies, we can say that maximum disparity is seen in borderline cases. Parity in the polar group is maximum, because they are stable and showed a fixed histopathology, while borderline and indeterminate groups may have different histopathology in different site and lesion.
The clinicopathological picture is determined by the equilibrium between the agent and the host resistance. Skin has different pathophysiological subunits wherein there is some local modulation of the central host response as a result of which there are different grades of resistance and hence different clinicopathological responses in different areas. We conclude from our study that histopathological examination should be carried out in all cases of leprosy to arrive at a definite diagnosis of leprosy and to classify the type of the disease.
| 1. |
Sehgal VN. Leprosy. Dermatol Clin 1994;12:629-41.
[Google Scholar]
|
| 2. |
Ridley DS, Jopling. WHO classification of leprosy according to immunity: A five group system. Int J Lepr 1966;34:255-73.
[Google Scholar]
|
| 3. |
Kar PK, Arora PN. Clinicopathological study of macular lesions in leprosy. Indian J Lepr 1994;66:435-41.
[Google Scholar]
|
| 4. |
Kalla G, Salodkar A, Kachhawa D. Clinical and histopathological correlation in leprosy. Int J Lepr 2000;68:184-5.
[Google Scholar]
|
| 5. |
Jerath VP, Desai SR. Diversities in clinical and histopathological classification of Leprosy. Lepr India 1982;54:30.
[Google Scholar]
|
Fulltext Views
2,869
PDF downloads
2,485





