Translate this page into:
Congenital self-healing histiocytosis presenting as blueberry muffin baby: A case report and literature review
2 Institute of Pathology, Faculty of Medicine, University of Belgrade, Belgrade, Serbia
Correspondence Address:
Milos Nikolic
Clinic of Dermatovenereology, Faculty of Medicine, University of Belgrade, Pasterova 2, 11000 Belgrade
Serbia
| How to cite this article: Popadic S, Brasanac D, Arsov B, Nikolic M. Congenital self-healing histiocytosis presenting as blueberry muffin baby: A case report and literature review. Indian J Dermatol Venereol Leprol 2012;78:407 |
Abstract
Congenital self-healing Langerhans cell histiocytosis (CSHLCH), also called as Hashimoto-Pritzker disease, is a rare, benign variant of histiocytosis. Despite the initial dramatic clinical presentation, affected infants are otherwise healthy and skin lesions disappear spontaneously within several weeks to months. We present a case of CSHLCH presenting as blueberry muffin baby. The lesions appeared in the first week of life and lasted 6 months. The follow-up period was 24 months, without any signs of relapse. At the pediatric dermatology unit of our clinic, during the last 20 years, we had 10 children with Langerhans cell histiocytosis and among them only one with CSHLCH. In the literature, we found only 5 newborns with Langerhans cell histiocytosis presenting as blueberry muffin baby, among them only 4 with self-healing CSHLCH. The early recognition of CSHLCH may spare children from redundant and potentially toxic systemic treatment.Introduction
Langerhans cell histiocytosis (LCH) results from abnormal proliferation of S-100 positive and CD1a positive cells with Birbeck granules. These cells may infiltrate single or multiple organs. It is important to distinguish malignant forms of LCH such as Letterer-Siwe disease, and benign forms such as Hashimoto-Pritzker LCH. Blueberry muffin baby (BMB) is rare neonatal syndrome characterized by generalized dark-bluish macular, papular or nodular lesions due to extramedullary hematopoesis. [1] LCH has rarely been associated with clinical presentation of BMB.
To the best of our knowledge, till now, less than 100 cases of CSHLCH have been reported, and among them only 4 with clinical presentation of BMB. [2],[3],[4]
Case Report
A male baby was born to 34-year-old gravida 2, para 1, blood type A, Rh+ mother at 32 weeks of gestation. Pregnancy was complicated by hypertension and delivery was performed by caesarean section. Maternal rubella titres were reported as adequate; and she had no known viral exposures, or rash. The baby weighed 2300 g with Apgar scores 6 and 7 at 1 and 5 min, respectively. Besides respiratory distress syndrome caused by lung immaturity, findings on other organs were unremarkable.
Skin lesions gradually appeared by the end of the first week and at the age of 30 days consisted of numerous non-blanching brownish-black macules ranging from 2 to 5 mm in diameter, papules and nodules up to 1 cm in diameter, disseminated over the trunk, face [Figure - 1] and extremities. One nodule on the trunk [Figure - 2], was particularly large, with scale-crust. Otherwise, the baby was afebrile with stable vital signs.
 |
| Figure 1: Disseminated brownish - black macules, papules and nodules on the face and neck |
 |
| Figure 2: Disseminated macules/papules and a nodule on the trunk in scapular area |
Mucous membranes, lymph nodes, liver and spleen were unaffected. Chest X-rays, pediatric bone surveys, abdominal and CNS ultrasound were normal. Ophthalmologic examination and audiology tests were normal. Complete routine serum biochemical analyses, CBC, urine and stool analyses were normal. TORCH complex (toxoplasmosis, rubella, cytomegalovirus and herpes), VDRL and HIV antibody were negative. Bacterial cultures of blood and urine were negative.
Skin biopsies were performed, the first of the ulcerated nodule and the second of a hyperpigmented macule. Both biopsies showed diffuse dermal infiltrate consisting of uniform cells with abundant eosinophilic cytoplasm and reniform or infolded vesicular nuclei [Figure - 3]a. Extravasated red blood cells, occasional multinuclear giant cells and eosinophils were intermixed within the infiltrate. Immunohistochemical analysis revealed diffuse S-100 and CD1a [Figure - 3]b expression and focal CD68 positivity.
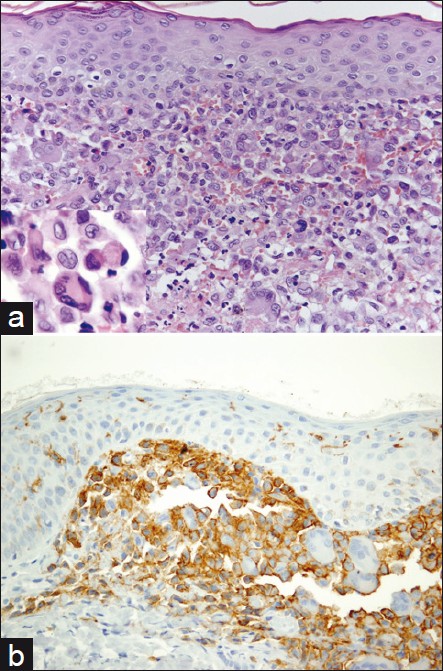 |
| Figure 3: (a) Dermal infiltrate with uniform cells showing reniform or infolded nuclei (inset) admixed with dispersed multinuclear cells, eosinophils and red blood cells (H and E, ×400, inset �1000). (b) Diffuse expression of CD1a in the dermal infiltrate (streptavidin-biotin, ×400) |
Histopathological appearance and immunohistochemical results were consistent with LCH. Since the baby had no signs of other organ involvement, a presumptive diagnosis of self-healing histiocytosis Hashimoto-Pritzker was established. Topical betamethasone dipropionate ointment bid was initiated and an observational approach was chosen in order to identify possible signs of systemic involvement.
During the next 6 months, all skin lesions disappeared, some leaving postinflammatory hyperpigmentation or scars. During the following 24 months (the last check-up was in August 2011) the patient remained healthy with no evidence of recurrence or systemic involvement.
Discussion
Congenital self-healing LCH was first described by Hashimoto and Pritzker in 1973. It is a rare disease, characterized by disseminated/generalized papules, vesicles, or nodules, occasionally with scaling, sometimes urticarial or hemangioma-like.
Affected infants are otherwise healthy and skin lesions tend to involute spontaneously within weeks to months. The diagnosis of LCH is based on histopathology which is indistinguishable for all forms of LCH. Characteristic histopathology and absence of other system involvement permit differentiation of benign forms of LCH. The diagnosis of CSHLCH should be made only retrospectively, after exclusion of involvement of other organs/systems.
According to the data collected by Belhadjali et al., CSHLCH may be divided into two groups, the first group with skin lesions appeared at birth, and the second group with later onset, as observed in our patient. [5] Estimated incidence of LCH is 2.24 to 8.9 cases/one million/year among European children. [6],[7] The real incidence of self healing LCH is unknown and may be underestimated due to the spontaneous resolution and failure of clinical recognition. [8]
Blueberry muffin baby is a rare neonatal skin presentation. [1],[2],[3],[4],[9] NLM PubMed search for blueberry muffin baby reveals only 40 references.
The term blueberry muffin baby was initially used for newborns with congenital rubella and later for other congenital infections (TORCH, Parvovirus, Coxsackie virus, Epstein-Barr and syphilis), hematologic disorders (spherocytosis, alloimmuniszation, twin-twin transfusion syndrome and foeto-maternal transfusion), metabolic disorders, neoplastic (congenital leukaemia, neuroblastoma, congenital rhabdomyosarcoma) and other diseases (histiocytosis, lupus). [1],[2],[3] The initial clinical presentation in our patient was highly suggestive for blueberry muffin baby. We excluded infections and other known causes of BMB. The histopathological finding and immunohistochemistry confirmed the diagnosis of LCH. Enjolras et al., first reported three patients with LCH presenting as BMB. [3] The main characteristics of all published cases of LCH presenting as BMB are summarized in [Table - 1].
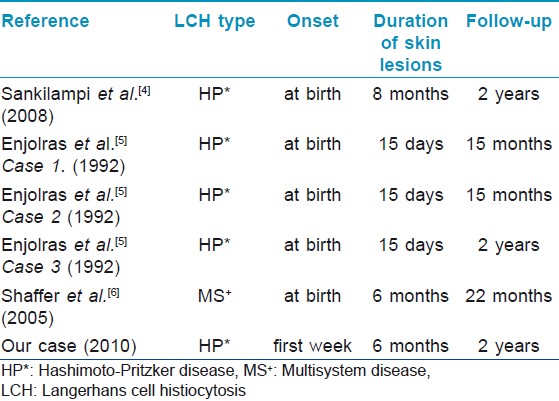
Lesions in all reported patients cleared rapidly, from two weeks up to 8 months. In our patient, the lesions regressed in 6 months. Blueberry muffin baby was the presentation of CSHLCH in 5/6 cases, and in 1/6 patients BMB was the initial presentation of LCH with multiorgan involvement [Table - 1].
Topical steroids can be beneficial as the first line therapy, particularly for erythematous lesions. Surgical excision may be the treatment of choice for isolated skin nodules. Other treatment modalities have been suggested for mild skin LCH, such as topical nitrogen mustard, psoralen with ultraviolet light, tacrolimus ointment. Overtreatment of isolated skin disease should be avoided. [10]
During the last 20 years, we treated 10 pediatric patients with LCH, among them 9 with Letterer-Siwe disease and only one with CSHLCH.
The early recognition of CSHLCH will spare children from redundant and potentially toxic systemic treatment.
| 1. |
Mehta V, Balachandran C, Lonikar V. Blueberry muffin baby: A pictoral differential diagnosis. Dermatol Online J2008;14:8.
[Google Scholar]
|
| 2. |
Sankilampi U, Huikko-Tarvainen S, Karja V, Pirinen E, Naukkarinen A, Hollmen A. Congenital Langerhans cell histiocytosis mimicking a "blueberry muffin baby". J Pediatr Hematol Oncol 2008;30:245-8.
[Google Scholar]
|
| 3. |
Enjolras O, Leibowitch M, Bonacini F, Vacher-Lavenu MC, Escande JP. Congenital cutaneous Langerhans histiocytosis. Apropos of 7 cases. Ann Dermatol Venereol 1992;119:111-7.
[Google Scholar]
|
| 4. |
Shaffer MP, Walling HW, Stone MS. Langerhans cell histiocytosis presenting as blueberry muffin baby. J Am Acad Dermatol 2005;53:143-6.
[Google Scholar]
|
| 5. |
Belhadjali H, Mohamed M, Mahmoudi H, Youssef M, Moussa A, Chouchane S, et al. Self-healing Langerhans cell histiocytosis (Hashimoto-Pritzker disease): Two Tunisian cases. Acta Dermatovenerol Alp Panonica Adriat 2008;17:188-92.
[Google Scholar]
|
| 6. |
Müller J, Garami M, Hauser P, Schuler D, Csóka M, Kovács G, et al. Hungarian experience with Langerhans cell histiocytosis in childhood. J Pediatr Hematol Oncol 2006;23:135-42.
[Google Scholar]
|
| 7. |
Stalemark H, Laurencikas E, Karis J, Gavhed D, Fadeel B, Henter JI. Incidence of Langerhans cell histiocytosis in children: A population-based study. Pediatr Blood Cancer 2008;51:76-81.
[Google Scholar]
|
| 8. |
Kapur P, Erickson C, Rakheja D, Carder KR, Hoang MP. Congenital self-healing reticulohistiocytosis (Hashimoto-Pritzker disease): Ten-year experience at Dallas Children's Medical Center. J Am Acad Dermatol 2007;56:290-4.
[Google Scholar]
|
| 9. |
Bacchetta J, Douvillez B, Warin L, Girard S, Pages MP, Rebaud P, et al. Blueberry Muffin Baby and spontaneous remission of neonatal leukaemia. Arch Pediatr 2008;15:1315-10.
[Google Scholar]
|
| 10. |
Abla O, Egeler RM, Weitzman S. Langerhans cell histiocytosis: Current concepts and treatments. Cancer Treat Rev 2010;36:354-9.
[Google Scholar]
|
Fulltext Views
3,969
PDF downloads
1,997





