Translate this page into:
Congenital self-healing Langerhans cell histiocytosis in a male neonate
Correspondence Address:
Hua Wang
No. 136, 2nd Zhong Shan Road, Yu Zhong District, Chong Qing
China
| How to cite this article: Tan Q, Gan LQ, Wang H. Congenital self-healing Langerhans cell histiocytosis in a male neonate. Indian J Dermatol Venereol Leprol 2015;81:75-77 |
Sir,
Congenital self-healing Langerhans cell histiocytosis (CSHLCH) is a self-limited variant of Langerhans cell histiocytosis (LCH) and is characterized by the eruption of multiple disseminated, red-brown crusted papulovesicles that can increase in size and number during the first few weeks of life. [1] Systemic signs are usually absent. We describe a case of this rare but self-limited disease and emphasize the need for long-term follow-up in these patients, even after spontaneous regression of the lesions.
An 18-day-old male neonate was admitted to our hospital with multiple crusted papulovesicular lesions over the body. The neonate was born by spontaneous vaginal delivery at 38 weeks of gestation to a healthy 25-year-old mother. The pregnancy was uncomplicated, with no adverse perinatal events. The parents did not have a history of genital or oral herpes simplex virus (HSV) and had nonreactive Venereal Disease Research Laboratory (VDRL) tests. The mother reported that the lesions were present on the neonate′s second day of life and gradually increased in number. There were no features of a systemic illness in the neonate who was otherwise healthy and feeding well. Physical examination revealed multiple crusted erythematous papules diffusely distributed over the scalp, face and trunk, sparing the mucous membranes, palms and soles [Figure - 1]. Tzanck smear was negative for multinucleated giant cells. There was neither hepatosplenomegaly nor lymphadenopathy. Systemic evaluation including complete blood counts, serum biochemistry, liver function tests, radiographic skeletal survey, ultrasound of the abdomen, bone marrow aspiration, and comprehensive metabolic panels were within normal limits. We did not performed CT scan of the head, chest and abdomen of the patient.
 |
| Figure 1: Crusted erythematous papules distributed over the trunk |
Histopathologic examination of a papule from the trunk revealed an extensive infiltrate composed of sheets of histiocytes that were associated with numerous eosinophils and occasional neutrophils [Figure - 2]. Immunohistochemistry examination showed that most of the histiocytes were positive for S-100 protein [Figure - 3], CD1a [Figure - 4], and CD68. Electron microscopic examination demonstrated Birbeck (Langerhans) granules within the cytoplasm of some of the histiocytes. The granules were tennis racket-shaped [Figure - 5]. Based on these histopathological, immunohistochemical, and ultrastructural features, together with the clinical characteristics, a diagnosis of congential self-healing Langerhans cell histiocytosis was made. The lesions completely disappeared at 6 months of age leaving hypopigmented scars. The patient showed no signs of cutaneous or internal Langerhans cell histiocytosis at 1 year of age.
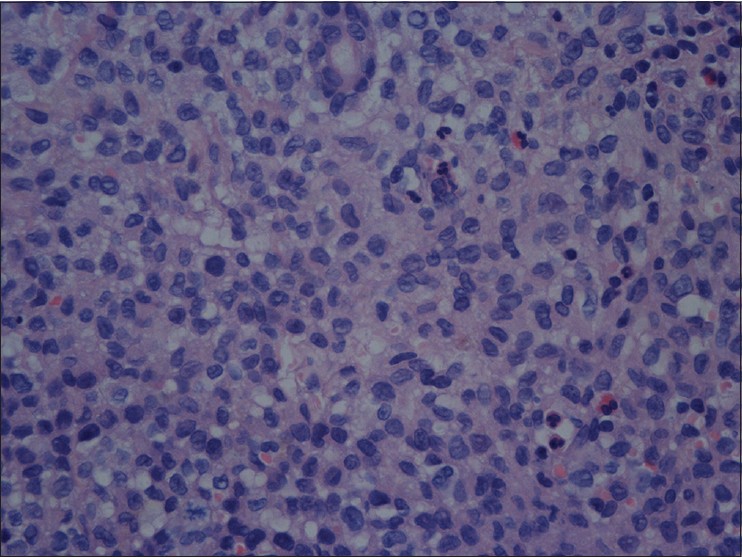 |
| Figure 2: Histiocytes infiltrated with eosinophils in the dermis (H and E, ×400) |
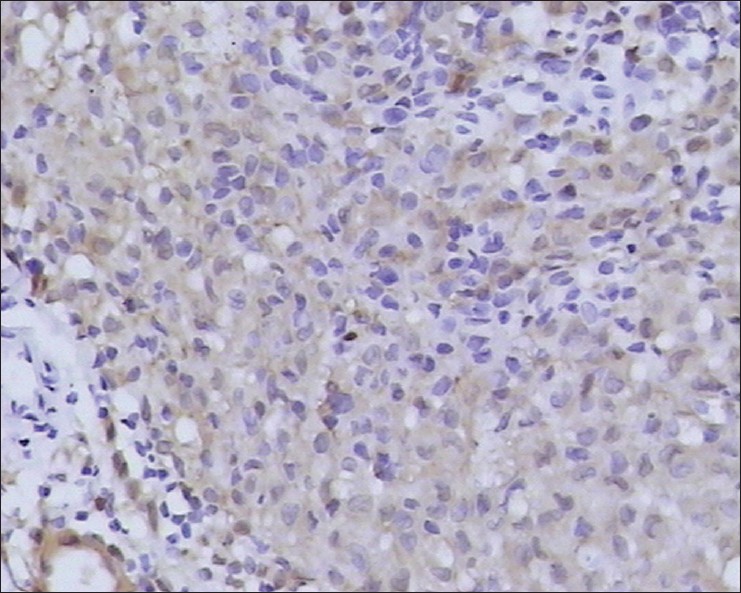 |
| Figure 3: Infiltrating histiocytes are positive for S-100 protein (magnification, ×400) |
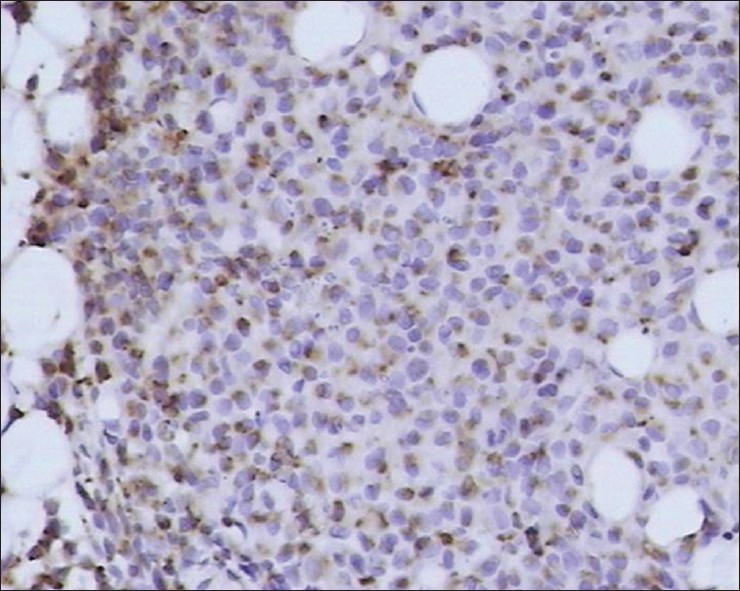 |
| Figure 4: Infiltrating histiocytes are positive for CD1a protein (magnification, ×400) |
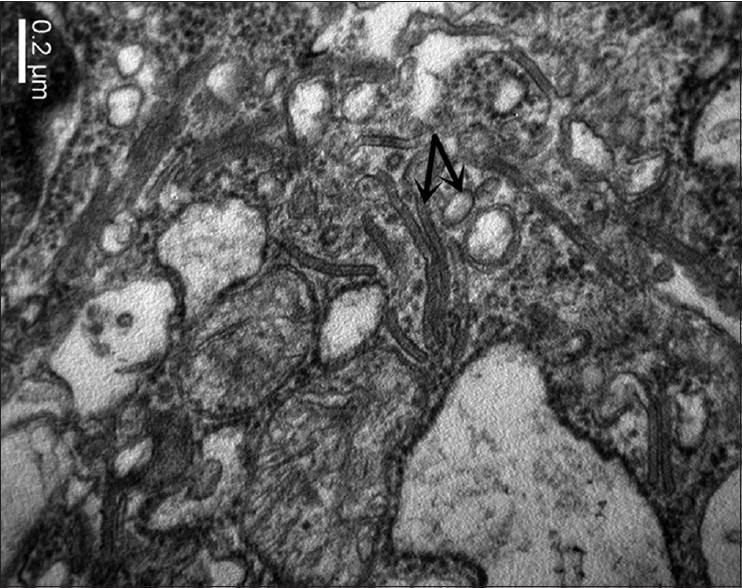 |
| Figure 5: Electron photomicrograph showing Birbeck granules |
Congential self-healing Langerhans cell histiocytosis is a confounding disorder with a wide spectrum of outcomes ranging from spontaneous remissions to metastasis and death. [2] Langerhans cell histiocytosis has four main clinical forms: eosinophilic granuloma, Hand-Schüller-Christian disease, Letterer-Siwe disease and congenital self-healing reticulohistiocytosis. The self-healing form of congenital Langerhans cell histiocytosis was first reported in 1973 by Hashimoto and Pritzker who described a congenital disorder characterized by multiple reddish-brown crusted papulovesicles limited to the skin that spontaneously healed without sequelae. [3] Subsequently, more than 40 cases have been reported in the literature. [4]
Cutaneous changes are the most common initial manifestation in neonates with Langerhans cell histiocytosis. The disease is limited to the skin and/or mucous membranes in one-third of patients. The skin lesions of Langerhans cell histiocytosis exhibit a wide spectrum of morphology. The most common initial skin lesion is erythematous, often crusted, and contains vesiculo-pustules. [2] It is important to distinguish this condition from other vesiculo-bullous diseases present in neonates, including disseminated herpes simplex, varicella, cytomegalovirus, congenital candidiasis, impetigo neonatorum, congenital syphilis, erythema toxicum neonatorum, transient neonatal pustular melanosis, epidermolysis bullosa, and incontinentia pigmenti. [5] Tzanck preparations, bacterial, viral, and fungal cultures, and serum biochemistry help to differentiate congenital self-healing Langerhans cell histiocytosis from other disorders. In our case, the neonate was well and had no evidence of bacterial, fungal, and viral infections.
The morphologic characteristics of the lesions are not helpful in predicting the extent of disease. [2] Congenital self-healing Langerhans cell histiocytosis should be differentiated from other histiocytic disorders known to spontaneously regress in infancy, namely juvenile xanthogranuloma, generalized eruptive histiocytoma, and indeterminate cell histiocytoma. [6] A skin biopsy must be performed for a definitive diagnosis. The most interesting feature of the lesions of congenital self-healing Langerhans cell histiocytosis is their spontaneous involution, usually by 3 months of age, leaving hypopigmented or hyperpigmented macules. [5] In our case, the lesions regressed at 6 months of age. The prognosis of the disease depends on the age of onset, number of organs involved, and physiologic dysfunction. Treatment of Langerhans cell histiocytosis and congenital self-healing Langerhans cell histiocytosis in the neonate varies and there have been case reports of patients with purely cutaneous disease who have developed permanently disabling diseases such as diabetes insipidus. [2] Therefore, a thorough systemic evaluation is warranted to exclude extracutaneous disease in these patients. A close follow-up is recommended for all patients, as spontaneous resolution of skin lesions does not rule out the possibility of eventual progression or relapse, either in the skin or at extracutaneous sites. [6]
| 1. |
Morgan KM, Callen JP. Self-Healing Congenital Langerhans Cell Histiocytosis Presenting as Neonatal Papulovesicular Eruption. J Cutan Med Surg 2001;5:486-9.
[Google Scholar]
|
| 2. |
Stein SL, Paller AS, Haut PR, Mancin AJ. Langerhans cell histiocytosis presenting in the neonatal period: A retrospective case series. Arch Pediatr Adolesc Med 2001;155:778-83.
[Google Scholar]
|
| 3. |
Hashimoto, Pritzker MS. Electron microscopic study of reticulohistiocytoma: An unusual case of congenital, self-healing reticulohistiocytosis. Arch Dermatol 1973;107:263-70.
[Google Scholar]
|
| 4. |
Inuzuka M, Tomita K, Tokura Y, Takigawa M. Congenital self-healing reticulo histiocytosis presenting with hemorrhagic bullae. J Am Acad Dermatol 2003;48:S75-7.
[Google Scholar]
|
| 5. |
Avram MM, Gobel V, Sepehr A. Case records of the Massachusetts General Hospital. Case 30-2007. A newborn girl with skin lesions. N Engl J Med 2007; 357:1327-35.
[Google Scholar]
|
| 6. |
Walia M, Paul P, Mishra S, Mehta R. Congenital Langerhans Cell Histiocytosis: The Self-Healing Variety. J Pediatr Hematol Oncol 2004;26:398-402.
[Google Scholar]
|
Fulltext Views
4,361
PDF downloads
2,571





