Translate this page into:
Current treatment of onychomycosis
Correspondence Address:
Devinder Mohan Thappa
Department of Dermatology and STD, JIPMER, Pondicherry - 605 006
India
| How to cite this article: Thappa DM. Current treatment of onychomycosis. Indian J Dermatol Venereol Leprol 2007;73:373-376 |
Onychomycosis accounts for one-third of integumentary fungal infections and one-half of all nail disease. [1] Onychomycosis is most commonly caused by dermatophytes, although Candida species and nondermatophyte molds may also cause disease. [2]
Therapeutic options for the treatment of onychomycosis range from no therapy, palliative care, mechanical or chemical debridement, topical and systemic antifungal agents to a combination of two or more of these modalities. [3] Factors that influence the choice of therapy include the presentation and severity of the disease, current medications the patient is taking, previous therapies for onychomycosis and their response, physician and patient preference and the cost of therapy. [3]
The primary aim of treatment is to eradicate the organism as demonstrated by microscopy and culture. However, eradication of the fungus does not always render the nails normal as they may have been dystrophic prior to infection. Such dystrophy may be due to trauma or nonfungal nail disease; this is particularly likely in cases where yeasts or nondermatophyte molds (secondary pathogens and saprophytes respectively) are isolated. [4]
Topical Therapy
The active antifungal agent in these preparations is an imidazole, an allylamine or a polyene. Two transungual delivery systems are currently available in India: amorolfine 5% nail lacquer and ciclopirox olamine 8% nail lacquer. After evaporation of the solvent, the concentration of the active ingredient, ciclopirox or amorolfine, increases to 34.8 and 25% respectively; this enhances transungual diffusion. [3]
Amorolfine nail lacquer is applied once a week, whereas ciclopirox olamine nail lacquer is applied daily. [4] Long-term (6-12 months) monotherapy has been used in the treatment of white superficial onychomycosis and distal subungual onychomycosis limited to the distal nail of a few digits. Nail lacquers are also utilized as adjunctive therapy or for secondary prophylaxis in severe onychomycosis. Amorolfine nail lacquer alone was effective in around 50% of cases of distal subungual onychomycosis. [5] Although no recent reports are available, tioconazole 28% nail solution was suggested as one of the topical therapies for onychomycosis in past studies. [6] Recently, topical acidified nitrite treatment has shown promising results. [7]
Systemic Therapy
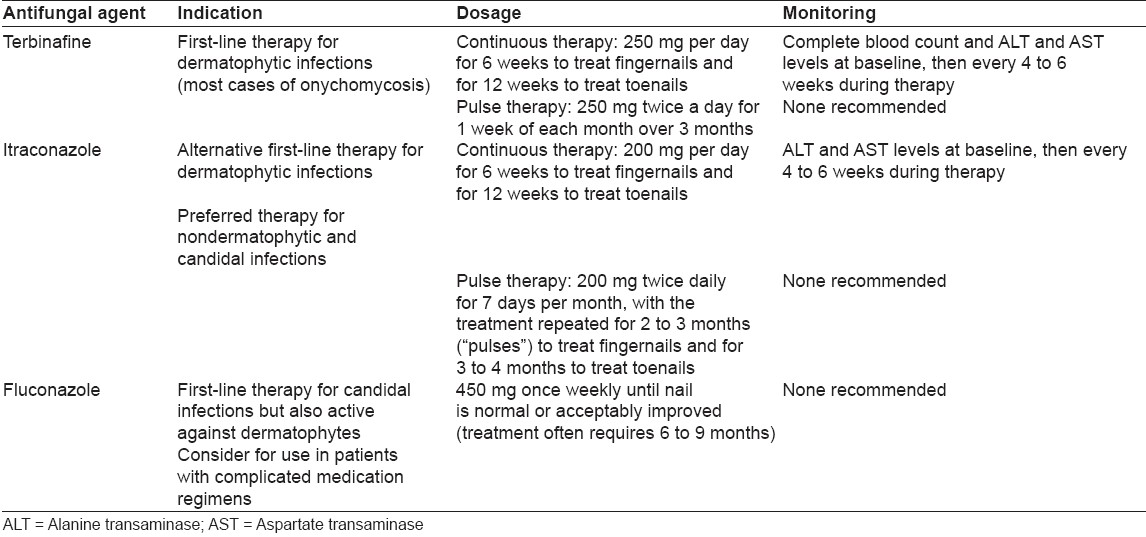
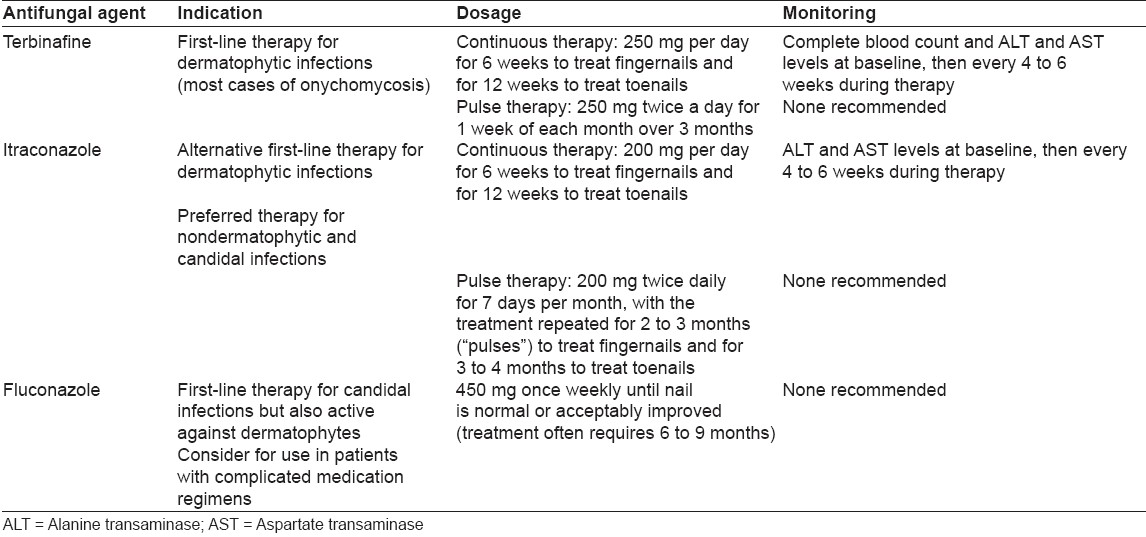
Orally administered griseofulvin has been available for many years, but its use is limited by its narrow spectrum, the necessity for long courses of treatment, disappointing cure rates (around 30%) and high relapse rates. [1],[8] It is the only antifungal agent licensed for use in children with onychomycosis in USA and UK. The oral form of ketoconazole is much more effective but carries risk of hepatotoxicity. [1],[8] Current evidence supports the use of newer antifungal agents as part of individualized treatment plans that consider patient profiles, nail characteristics, infecting organism(s), potential drug toxicities and interactions and adjuvant treatments. [3] The newer agents include triazoles and allylamines that have become first-line medications in the treatment of onychomycosis [Table - 1]. [1],[8],[9] These agents offer shorter treatment courses, higher cure rates and fewer relapses. Of the newer drugs, terbinafine and itraconazole are most widely used.
Terbinafine is superior to itraconazole both in vitro and in vivo for dermatophyte onychomycosis and should be considered first-line treatment, with itraconazole as the next best alternative. [3] Cure rates of 80-90% for fingernail infection and 70-80% for toenail infection can be expected. These medications share characteristics that enhance their effectiveness: prompt penetration of the nail and nail bed, persistence in the nail for months after discontinuation of therapy and generally good safety profiles.
Terbinafine
Terbinafine is the drug of choice in tinea unguium. This agent is notably less effective against nondermatophytes, including Candida species and molds. In addition to transient tolerance problems, terbinafine has several important drug interactions because of its hepatic metabolism. [1],[10],[11] Terbinafine is not recommended for patients with chronic or active liver disease. [12],[13]
Terbinafine 250 mg per day is given continuously for 12 weeks to treat toenail infections and for 6 weeks to treat fingernail infections. [1],[14] Studies have shown that the regimen for toenails results in a mycologic cure rate of 71-82% and a clinical cure rate of 60-70%. [15],[16] Studies comparing terbinafine pulse therapy of 250 mg twice a day for 1 week of each month for 3 months with continuous therapy over 3 months showed no difference in efficacy. [9]
Itraconazole
Itraconazole has a broad antifungal spectrum that includes dermatophytes, many nondermatophytic molds and Candida species. [1] Headache, rash and gastrointestinal upset occur in about 7% of treated patients, but hepatic toxicity is rare. [13],[14] Because itraconazole is metabolized by the hepatic cytochrome P450 system, significant drug interactions can occur notably with statins, quinidine, pimozide, and benzodiazepines, amongst others. [1],[11],[13] Increased gastric pH decreases the absorption of itraconazole. [1],[11],[13] Therefore, the effectiveness of this antifungal agent can be decreased by histamine H 2 blockers and proton pump inhibitors.
The dosage of itraconazole is 200 mg once daily taken continuously for 12 weeks to treat toenail infections and for 6 weeks to treat fingernail infections. Pulse treatment consists of 200 mg taken twice daily for 1 week per month, with the treatment repeated for 2-3 months (i.e., two to three ′pulses′) for fingernail infections. [14],[17],[18] This dosage, given in three to four pulses, has also been shown to be effective in the treatment of toenail infections. [19],[20],[21] Published studies have demonstrated similar success rates for continuous and pulse therapies, with mycologic cure rates ranging from 45 to 70% and clinical cure rates ranging from 35 to 80%. [14],[19],[20]
Fluconazole
Like itraconazole, fluconazole is active against common dermatophytes, Candida species and some nondermatophytic molds. [1] Fluconazole is not currently approved for the treatment of onychomycosis, but attention has been focused on once-weekly dosing (450 mg), taking advantage of the drug′s pharmacokinetics to reduce treatment costs, and potentially improve compliance. [22],[23],[24] In fingernail onychomycosis, [25] fluconazole in a dosage of 450 mg taken once weekly for 3 months was associated with a 90% clinical cure rate and nearly total mycologic eradication. Lower dosages were slightly less effective.
Treatment of Yeast Infections
Itraconazole is the most effective agent for the treatment of candidal onychomycosis where the nail plate is invaded by the organism. It is used in the same dosage regimen as for dermatophytes; treatment duration is 2 months for fingernails and 3-4 months for toenails. Fluconazole is thought to be equally effective in candidal onychomycosis and can be used at the dosage of 50 mg daily or as pulse therapy at the dosage of 300 mg per week. Duration of treatment is 6 weeks for fingernails and 3 months for toenails. Patients with chronic mucocutaneous candidiasis may fail to respond to normal dosages and require higher or even double dosages of antifungals, that too for longer durations. [26]
Treatment of Nondermatophyte Molds
Many varieties of saprophytic molds can invade diseased nail. [3] Although itraconazole has a broader spectrum, there is little categorical evidence to support the choice of one drug. [3] In USA and Europe, ciclopirox nail lacquer has its advocates. Nail avulsion followed by an oral agent during the period of regrowth is probably the best method. [4]
Treatment of Onychomycosis in Children
Onychomycosis in children is rare, with an estimated prevalence of 0.2%. [21] Although griseofulvin is still considered the treatment of choice in dermatophyte infections of children, this possibly may not apply to onychomycosis. [27] Topical antifungals can possibly better penetrate the thin nail plate of children and are used as first choice treatment by several authors. [27] Terbinafine, itraconazole and fluconazole have all been used in children safely.
Improvised Regimens
Sequential treatment with itraconazole and terbinafine increases cure rates; the regimen is two pulses of itraconazole 400 mg/day for 1 week a month followed by one or two pulses of terbinafine 500 mg/day for 1 week a month. [28]
Supplemental systemic therapy for onychomycosis of the toes should be considered when the nail has slow outgrowth; in case of a thick nail, lateral onychomycosis, severe onychomycosis or a patient with immunosuppression or peripheral vascular disease or diabetes. [29],[30] A terbinafine booster is administered for an extra period of 4 weeks between months 6 and 9 from the start of therapy; similarly, an extra pulse of itraconazole may be given. [31],[32]
Adjuvant Treatments
Surgical or chemical nail avulsion may be useful in patients with severe onycholysis, extensive nail thickening or longitudinal streaks or ′spikes′ in the nail. These nail changes can be caused by a granulated nidus of infection (dermatophytoma), which responds poorly to standard courses of medical therapy. [33],[34]
To improve treatment outcomes and prevent recurrence, nails should be cut short and kept clean. The feet need to be dried completely following a bath or shower. [29],[30] Recognizing and improving chronic health conditions (e.g., controlling diabetes, quitting smoking, etc.) may also affect the outcome of therapy. It would be appropriate to discard, or perhaps ′rest,′ old pairs of shoes, once cure of onychomycosis has been achieved.
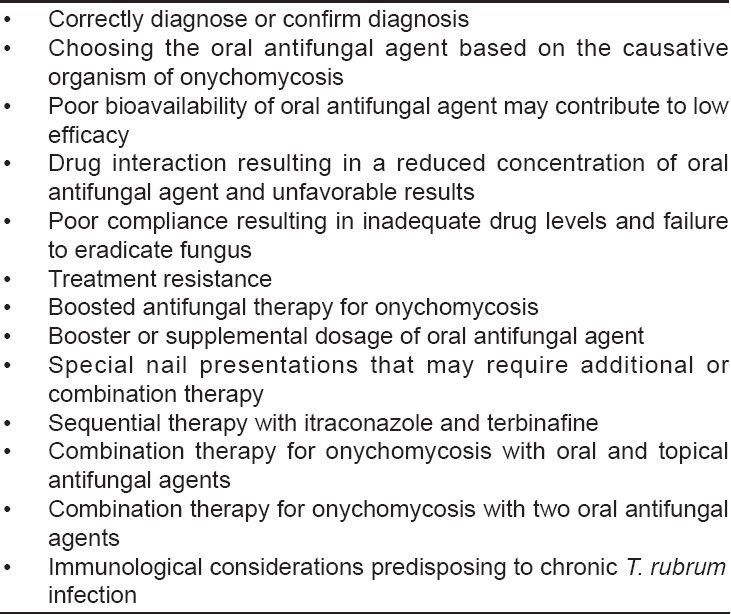
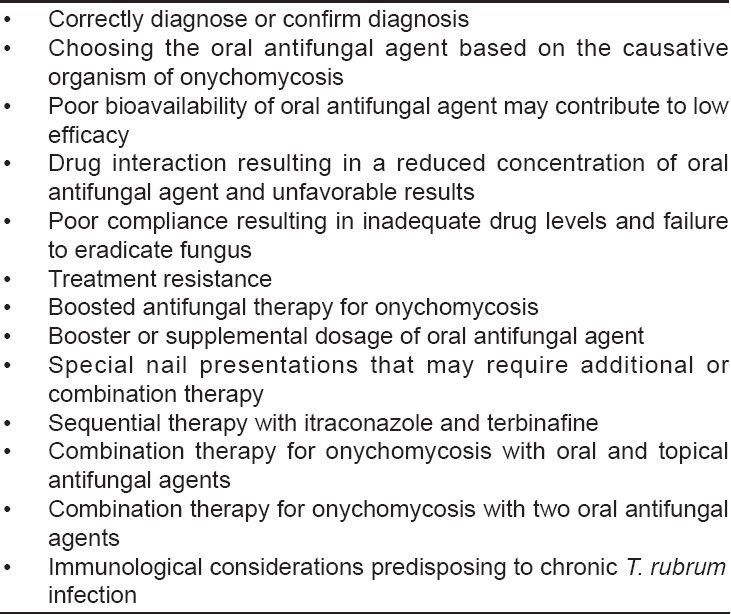
Measures that may be helpful in managing unsuccessful treatment or relapse are listed in [Table - 2]. There has been some concern about evolving drug resistance among fungal pathogens. However, the impact of antifungal resistance on the treatment of onychomycosis is not yet clear. Failure to respond to therapy for onychomycosis could be related to the presence of dormant chlamydospores and arthroconidia within the diseased nail plate. [35],[36]
| 1. |
Rodgers P, Bassler M. Treating onychomycosis. Am Fam Physician 2001;63:663-72,677-8.
[Google Scholar]
|
| 2. |
Sobera JO, Elewski BE. Onychomycosis, Nails: diagnosis, therapy, surgery, 3 rd ed. Elsevier Saunders: China; 2005. p. 123-31.
[Google Scholar]
|
| 3. |
Gupta AK, Ryder JE, Baran R. The use of topical therapies to treat onychomycosis. Dermatol Clin 2003;21:481-9.
[Google Scholar]
|
| 4. |
Roberts DT, Taylor WD, Boyle J; British Association of Dermatologists. Guidelines for treatment of onychomycosis. Br J Dermatol 2003;148:402-10.
[Google Scholar]
|
| 5. |
Zaug M, Bergstraesser M. Amorolfine in onychomycosis and dermatomycosis. Clin Exp Dermatol 1992;17:61-70.
[Google Scholar]
|
| 6. |
Hay RJ, MacKie RM, Clayton YM. Tioconazole nail solution: An open study of its efficacy in onychomycosis. Clin Exp Dermatol 1985;10:111-5.
[Google Scholar]
|
| 7. |
Finnen MJ, Hennessy A, McLean S, Bisset Y, Mitchell R, Megson IL, et al . Topical application of acidified nitrite to the nail renders it antifungal and causes nitrosation of cysteine groups in the nail plate. Br J Dermatol 2007;157:494-500.
[Google Scholar]
|
| 8. |
Roberts DT, Bilsland DJ. Tinea unguium. In : Lebwohl MG, Heymann WR, Berth-Jones J, Coulson I, editors. Treatment of skin diseases-comprehensive therapeutic strategies, 2 nd ed. Mosby Elsevier: China; 2006. p. 651-3.
[Google Scholar]
|
| 9. |
Choi S. Fungal infections. In : Arndt KA, Hsu JT, editors. Manual of dermatologic therapeutics, 7 th ed. New Delhi: Lippincott Williams and Wilkins 2007. p. 83-93.
[Google Scholar]
|
| 10. |
Roberts DT. Oral terbinafine (Lamisil) in the treatment of fungal infections of the skin and nails. Dermatology 1997;194:37-9.
[Google Scholar]
|
| 11. |
Katz HI, Gupta AK. Oral antifungal drug interactions. Dermatol Clin 1997;15:535-44.
[Google Scholar]
|
| 12. |
Del Rosso JQ, Gupta AK. Oral antifungal agents: Recognition and management of adverse reactions. Todays Ther Trends 1997;15:75-84.
[Google Scholar]
|
| 13. |
Gupta AK, Ryder JE. The use of oral antifungal agents to treat onychomycosis. Dermatol Clin 2003;21:469-79.
[Google Scholar]
|
| 14. |
Gupta AK, De Doncker P, Scher RK, Haneke E, Daniel CR 3rd, Andre J, et al . Itraconazole for the treatment of onychomycosis. Int J Dermatol 1998;37:303-8.
[Google Scholar]
|
| 15. |
Hofmann H, Brautigam M, Weidinger G, Zaun H. Treatment of toenail onychomycosis: A randomized, double-blind study with terbinafine and griseofulvin. LAGOS II Study Group. Arch Dermatol 1995;131:919-22.
[Google Scholar]
|
| 16. |
Goodfield MJ, Andrew L, Evans EG. Short term treatment of dermatophyte onychomycosis with terbinafine. BMJ 1992;304:1151-4.
[Google Scholar]
|
| 17. |
Trepanier EF, Amsden GW. Current issues in onychomycosis. Ann Pharmacother 1998;32:204-14.
[Google Scholar]
|
| 18. |
Doncker PD, Gupta AK, Marynissen G, Stoffels P, Heremans A. Itraconazole pulse therapy for onychomycosis and dermatomycosis: An overview. J Am Acad Dermatol 1997;37:969-74.
[Google Scholar]
|
| 19. |
Havu V, Brandt D, Heikkila H, Hollmen A, Oksman R, Rantanen T, et al . A double-blind, randomised study comparing itraconazole pulse therapy with continuous dosing for the treatment of toe-nail onychomycosis. Br J Dermatol 1997;136:230-4.
[Google Scholar]
|
| 20. |
De Doncker P, Decroix J, Pierard GE, Roelant D, Woestenborghs R, Jacqmin P, et al . Antifungal pulse therapy for onychomycosis: A pharmacokinetic and pharmacodynamic investigation of monthly cycles of 1-week pulse therapy with itraconazole. Arch Dermatol 1996;132:34-41.
[Google Scholar]
|
| 21. |
Scher RK. Onychomycosis: Therapeutic update. J Am Acad Dermatol 1999;40:S21-6.
[Google Scholar]
|
| 22. |
Gupta AK, Scher RK, Rich P. Fluconazole for the treatment of onychomycosis:an update. Int J Dermatol 1998;37:815-20.
[Google Scholar]
|
| 23. |
Scher RK, Breneman D, Rich P, Savin RC, Feingold DS, Konnikov N, et al . Once-weekly fluconazole (150, 300 or 450 mg) in the treatment of distal subungual onychomycosis of the toenail. J Am Acad Dermatol 1998;38:S77-86.
[Google Scholar]
|
| 24. |
Ling MR, Swinyer LJ, Jarratt MT, Falo L, Monroe EW, Tharp M, et al . Once-weekly fluconazole (450 mg) for 4, 6 or 9 months of treatment for distal subungual onychomycosis of the toenail. J Am Acad Dermatol 1998;38:S95-102.
[Google Scholar]
|
| 25. |
Drake L, Babel D, Stewart DM, Rich P, Ling MR, Breneman D, et al . Once-weekly fluconazole (150, 300 or 450 mg) in the treatment of distal subungual onychomycosis of the fingernail. J Am Acad Dermatol 1998;38:S87-94.
[Google Scholar]
|
| 26. |
Tosti A, Piraccini BM, Lorenzi S, Iorizzo M. Treatment of nondermatphyte mold and Candida onychomycosis. Dermatol Clin 2003;21:491-7.
[Google Scholar]
|
| 27. |
Tosti A, Piraccini BM, Iorizzo M. Management of onychomycosis in children. Dermatol Clin 2003;21:507-9.
[Google Scholar]
|
| 28. |
Gupta AK, Lynde CW, Konnikov N. Single blind randomized study of sequential itraconazole and terbinafine pulse compared with terbinafine pulse for the treatment of toenail onychomycosis. J Am Acad Dermatol 2001;44:485-91.
[Google Scholar]
|
| 29. |
Gupta AK, Baran R, Summerbell R. Onychomycosis: Strategies to improve efficacy and reduce recurrence. J Eur Acad Dermatol Venereol 2002;16:579-86.
[Google Scholar]
|
| 30. |
Gupta AK, Ryder JE. How to improve cure rates for the management of onychomycosis. Dermatol Clin 2003;21:499-505.
[Google Scholar]
|
| 31. |
Gupta AK, Daniel CR. Onychomycosis: Strategies to reduce failure and recurrence. Cutis 1998;62:189-91.
[Google Scholar]
|
| 32. |
Gupta AK, Konnikov N, Lynde CW. Single-blind, prospective study evaluating the efficacy and safety of terbinafine and itraconazole for the treatment of dermatophyte toenail onychomycosis in the elderly. J Am Acad Dermatol 2000;44:479-84.
[Google Scholar]
|
| 33. |
Roberts DT, Evans EG. Subungual dermatophytoma complicating dermatophyte onychomycosis. Br J Dermatol 1998;138:189-90.
[Google Scholar]
|
| 34. |
Baran R, Hay RJ. Partial surgical avulsion of the nail in onychomycosis. Clin Exp Dermatol 1985;10:413-8.
[Google Scholar]
|
| 35. |
Piιrard GE, Piιrard-Franchimont C, Arrese JE. The boosted antifungal topical treatment (BATT) for onychomycosis. Med Mycol 2000;38:391-2.
[Google Scholar]
|
| 36. |
Piιrard GE, Piιrard-Franchimont C, Arrese JE. The boosted oral antifungal topical treatment for onychomycosis beyond the regular itraconazole pulse dosing regimen. Dermatology 2000;200:185-7.
[Google Scholar]
|
Fulltext Views
31,056
PDF downloads
3,809





