Translate this page into:
Cutaneous adverse drug reactions: An 8-year retrospective study on hospitalized patients in Southern China
2 Department of Clinical Medicine, Zhongshan School of Medicine, Sun Yat-sen University, Guangzhou, China
Correspondence Address:
Xingqi Zhang
Department of Dermatology, The First Affiliated Hospital, Sun Yat-sen University, No. 58, Zhongshan 2nd Road, Guangzhou, 510080
China
| How to cite this article: Wang F, Li Y, Mo Y, Shen C, Yang L, Zhang X. Cutaneous adverse drug reactions: An 8-year retrospective study on hospitalized patients in Southern China. Indian J Dermatol Venereol Leprol 2012;78:488-490 |
Sir,
Cutaneous adverse drug reactions (CADRs) are commonly seen among the hospitalized population. During the past few years, as more new drugs have been introduced into the market and the changes in drug use, it is important to document culprit drugs, clinical types and frequency of CADRs.
The purpose of this study was to assess recent trends of clinical types of CADRs and their causative agents in a hospital-based population for a period of 8 years in Southern China.
The clinical data of inpatients, diagnosed with CADR in our hospital from January 2003 to December 2010, were retrospectively analyzed. All reactions were reviewed by dermatologists and diagnosed in accordance with the definition of CADR provided by WHO. [1] Exfoliative dermatitis (ED), Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS) were classified as severe (S)- CADRs, and other cases with CADRs that did not fall into the S-CADRs category were termed non-severe (NS)-CADRs.
Data collected from inpatients of dermatological department were compared to those in a previous study, involving 198 CADRs cases from the same ward in the period from May 1984 to May 1994. [2] All statistical tests were performed with software Stata 10.0. Differences in prevalence of CADRs were assessed by Fisher exact probability test. Correlations were regarded as significant when P < 0.05.
During the 8-year period, a total of 524 patients were diagnosed with CADRs among 364,636 hospitalized patients. The prevalence of CADRs among hospitalized patients was 1.4/1000. Among all 524 patients, 208 (39.7%) were from the dermatological department while the rest 316 patients (60.3%) were from other departments. The average age of patients enrolled in this study was 43.85 years (with a range from 1 month to 93 years).
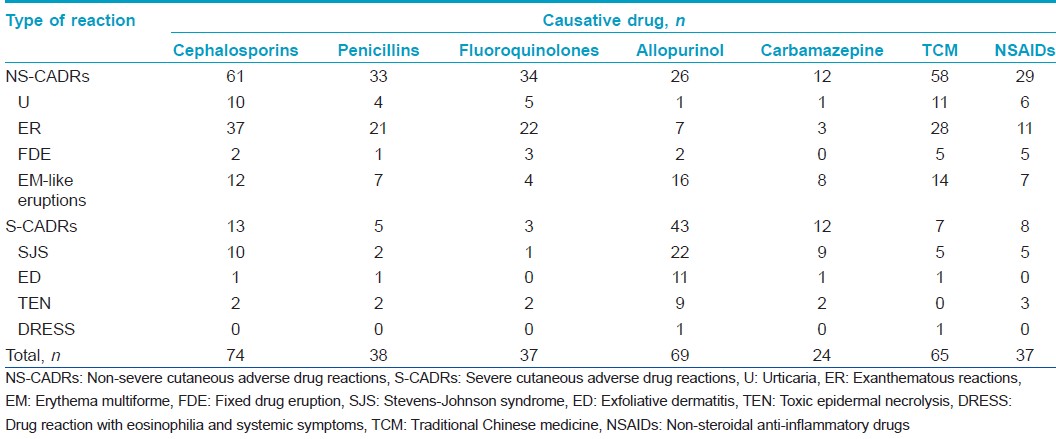
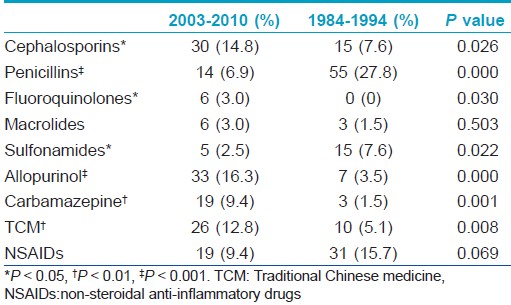
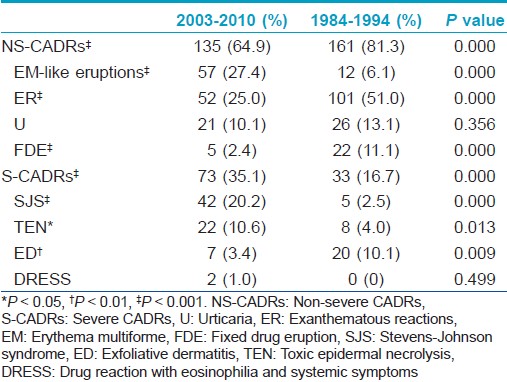
Analysis of culprit drugs was focused on patients who had taken a single medication before the skin symptoms appeared (N = 494). The 7 most common single drugs linked to the development of different types of CADRs were listed in [Table - 1]. Compared to the previous study, [2] the percentages of CADRs caused by allopurinol, carbamazepine, traditional Chinese medicine (TCM), cephalosporins, and fluoroquinolones were significantly higher (P<0.05, respectively) [Table - 2], and incidences of EM-like eruptions, SJS, and TEN were also higher in this study (P < 0.05, respectively) [Table - 3].
Incidences of CADRs varied from 1.6/1000 to 30/1000 in several previous studies conducted in hospital settings. [3],[4] The prevalence of 1.4/1000 in our study is close to that of a French survey (3.6/1000) [3] and that of a study in Northern China (1.6/1000), [4] which indicated CADRs were not uncommon in China.
Compared to the study from 1984 to 1994, disparity of culprit drugs was noted. The high incidences of cephalosporins-induced CADRs and fluoroquinolones-induced CARDs may be associated with increased exposure to cephalosporins and fluoroquinolones in certain populations because of florid usage of those antibiotics. The decline in use of sulfonamides in recent years could result in the low incidence of sulfonamides-induced CARDs. Carbapenems, which were reserved to treat grave bacterial infections, were found responsible for 22 cases (4.5% of 494 single drug-induced CADRs). Therefore, carbapenems should not be neglected as the incriminated drug causing CADRs. The phenomenon of high incidences of allopurinol- or carbamazepine-induced CADRs could be due to an increased use of allopurinol to treat gout or the increased use of carbamazepine to relieve pain.
TCM has been widely used in China, especially in Southern China. In agreement with previous studies, [5] TCM was found involved in CADRs and even in S-CADRs in this study. However, due to the complex composition, the causative ingredient of TCM was difficult to identify. But still, TCM has been considered as a therapeutic choice in an actual clinical practice as it induced more NS-CADRs rather than S-CADRs. 6 cases with CADRs were caused by biological agents, including gammaglobulin and monoclonal antibodies, such as rituximab. With the development of new biological agents, an increase in biologic-induced CADRs could be expected.
The prevalences of ER or FDE in hospitalized patients were decreased compared to that of the previous study. The reason might be that more patients with ER and FDE were not hospitalized in recent years. The increased administration of allopurinol and cabamazepine in recent years could be the reason for the increased incidences of EM-like eruptions and S-CADRs, especially SJS and TEN.
Briefly, our study emphasized that CADR couldn′t be overlooked in a hospital environment. Percentages of CADRs caused by allopurinol, carbamazepine, cephalosporins, and TCM were increased. Higher percentages of EM-like eruptions, SJS and TEN were also seen.
| 1. |
Edwards IR, Aronson JK. Adverse drug reactions: defnitions, diagnosis and management. Lancet 2000;356:1255-9.
[Google Scholar]
|
| 2. |
Lu NJ, Tong JZ. Clinical analysis of 198 patients with drug eruptions. South China J Dermatol Venereol 1995;2:9-10.
[Google Scholar]
|
| 3. |
Fiszenson-Albala F, Auzerie V, Mahe E, Durand-Stocco C, Crickx B, Descamps V. A 6-month prospective survey of cutaneous drug reactions in a hospital setting. Br J Dermatol 2003;149:1018-22.
[Google Scholar]
|
| 4. |
Li LF, Ma C. Epidemiological study of severe cutaneous adverse drug reactions in a city district of China. Clin Exp Dermatol 2006;31:642-7.
[Google Scholar]
|
| 5. |
Dasgupta A. Review of abnormal laboratory test results and toxic effects due to use of herbal medicines. Am J Clin Pathol 2003;120:127-37.
[Google Scholar]
|
Fulltext Views
2,351
PDF downloads
1,204





