Translate this page into:
Cutaneous aspergilloma in an immunocompetent patient treated with itraconazole
2 Department of Pathology, All India Institute of Medical Sciences (AIIMS), New Delhi, India
Correspondence Address:
Vinod K Sharma
Department of Dermatology, Venereology, and Leprology, All India Institute of Medical Sciences (AIIMS), New Delhi-110 029
India
| How to cite this article: Sharma VK, Krishna SG, Gupta C, Kumawat M. Cutaneous aspergilloma in an immunocompetent patient treated with itraconazole. Indian J Dermatol Venereol Leprol 2011;77:626 |
Sir,
Aspergillosis is an uncommon opportunistic fungal infection caused by a variety of species, of which Aspergillus fumigatus and Aspergillus niger are the common ones. It is generally seen in immunocompromised patients. [1],[2] We report a immunocompetent patient of cutaneous aspergilloma with associated allergic bronchopulmonary aspergillosis who showed excellent response to itraconazole.
A 45-year-old housewife presented with an erythematous, tender, indurated plaque with central ulceration and pus discharge on the right cheek since 2 years. The disease had started as an asymptomatic, single, hard erythematous nodule. It had recurred after excision and had enlarged rapidly for the past 6 months. It then became erythematous and swollen and later ulcerated, with pus discharge. There was no history of trauma, epistaxis, or ocular problems. The patient had history of asthma-like symptoms for 1 year (episodic dyspnea, dry cough), which had been relieved with bronchodilators and steroids. She received several courses of oral and intravenous antibiotics, as well as potassium iodide (1 g/ml) for 3 weeks, with no improvement.
Examination revealed a single erythematous tender plaque on the right cheek below the eye, measuring 5 cm Χ 3 cm. It was woody hard over the periphery, with a well-defined margin. There was central necrosis, with loss of underlying tissue [Figure - 1]a. General and systemic examination, including chest examination, were within normal limits. There was no clinical evidence of immunosuppression and ELISA for HIV was negative. The CD 4 count (646/μl) and immunoglobulin A, G, and M were within normal limits. The total IgE level was raised to 489 IU/ml and the absolute eosinophil count was slightly increased at 468/μl. The skin biopsy showed a moderate to dense collection of lymphocytes and histiocytes admixed with giant cells and eosinophils in the dermis. Many of the giant cells contained fungal elements, which showed septations and branching hyphae. Periodic acid-Schiff (PAS) and silver methenamine stains showed branching fungal hyphae [Figure - 2]a and b. Skin biopsy sent twice for fungal culture did not show any growth. The chest x-ray showed nonhomogenous opacities in the right middle zone and the left lower zone. high resolution computerized tomography (HRCT) of the chest showed cystic bronchiectasis with bronchoceles, and inspissated mucus plugs in the airways with areas of collapse and consolidation in both lungs. These radiological features were suggestive of allergic bronchopulmonary aspergillosis. Contrast enhanced computerized tomography (CECT) of the paranasal sinuses revealed maxillary sinusitis. Bronchial washings showed macrophages, polymorphs, and a few eosinophils. Stain for acid-fast bacillus (AFB) and fungal culture were negative.
 |
| Figure 1: (a)Erythematous plaque with necrotic center, untreated Figure 1b: Healing ulcer after 1 month of itraconazole |
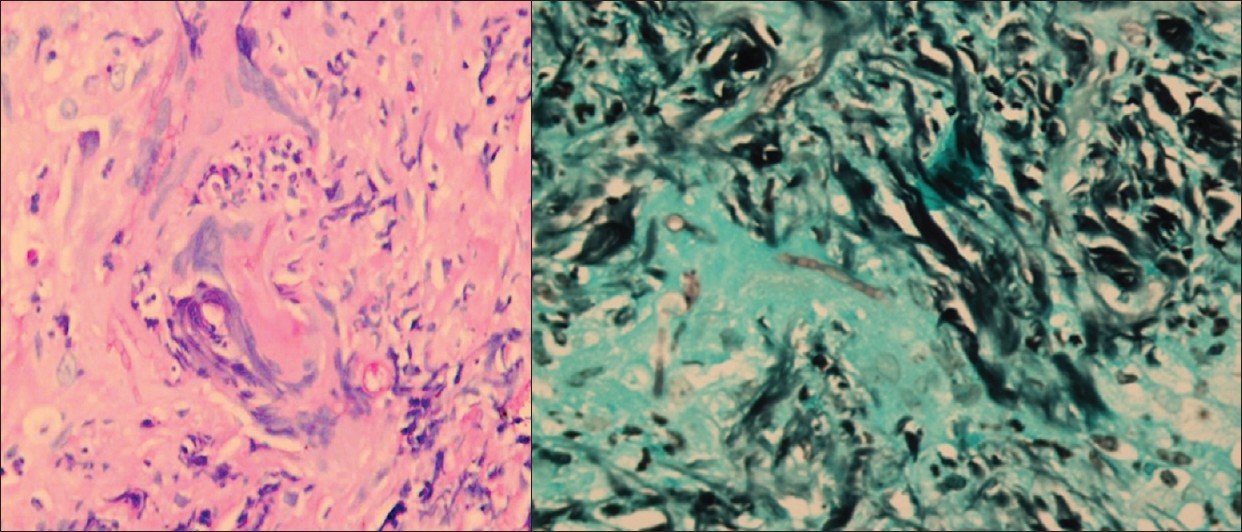 |
| Figure 2: (a)Microphotograph showing branching fungal hyphae. Note the acute-angle branching (PAS stain, ×100) Figure 2b: Microphotograph showing fungal hyphae (silver methenamine stain, ×100) |
Our diagnosis was cutaneous aspergilloma with sinus and lung involvement, and the patient was treated with itraconazole 100 mg twice daily. Within a week of starting treatment the patient showed improvement and within 1 month the cutaneous lesion had completely healed, leaving an area of depressed skin [Figure - 1]b; however, there was no significant change in the lung symptoms. Itraconazole was continued for 6 months and the improvement was sustained. At the last follow-up visit, 1 year after completion of treatment, there was no recurrence.
Cutaneous lesions are rare in aspergillosis. Primary cutaneous aspergillosis may present as macules, papules, plaques, or hemorrhagic bullae, which may progress to form necrotic ulcers covered by a heavy black eschar. [1],[2] Skin lesions occur in 5%-10% of patients with disseminated aspergillosis. Primary cutaneous aspergillosis occurs much less commonly. In these instances, the usual cause is implantation of the fungus following trauma, for example, at the site of intravenous cannulas or venipuncture, especially those that have been covered with occlusive dressings. [3]
Cutaneous aspergillosis is caused by infection with the ubiquitous soil- and water-dwelling saprophytes of the Aspergillus genus. A fumigatus is the most common pathogen associated with disseminated disease with cutaneous involvement, whereas A. flavusor A. terreus most often cause the less frequent primary infections of the skin. A. niger and A ustus have also been cultured from cutaneous lesions. The diagnosis is based on the clinical features and the results of skin biopsy, fungal culture, serology, and chest imaging. In tissue sections, narrow septate hyphae with delicate chitinous walls, bubbly blue cytoplasm, and acute-angle branching can be demonstrated, especially with special staining (as in our patient). Our patient had clinical features similar to those described in the literature. Pulmonary and paranasal involvement was confirmed on HRCT. Increased IgE and eosinophil counts pointed towards the presence of allergic bronchopulmonary aspergillosis. Response to itraconazole supports the fungal etiology. Till date, very few cases of cutaneous aspergillosis in immunocompetent patients have been reported. [3],[4] Our case is one of the few such cases. The dramatic response to itraconazole highlights the drug′s efficacy in the treatment of aspergillosis. Newer antifungals like voriconazole and caspofungin are used in resistant cases. [5]
| 1. |
Prasad PV, Babu A, Kaviarasan PK, Anandhi C, Viswanathan P. Primary cutaneous aspergillosis. Indian J Dermatol Venereol Leprol 2005;71:133-4.
[Google Scholar]
|
| 2. |
Chakrabarti A, Gupta V, Biswas G, Kumar B, Sakhuja VK. Primary cutaneous aspergillosis: Our experience in 10 years. J Infect 1998;37:24-7.
[Google Scholar]
|
| 3. |
Mohapatra S, Xess I, Swetha JV, Tanveer N, Asati D, Ramam M, et al. Primary cutaneous aspergillosis due to Aspergillus niger in an immunocompetent patient. Indian J Med Microbiol 2009;27:367-8.
[Google Scholar]
|
| 4. |
Ajith C, Dogra S, Radotra BD, Chakrabarti A. Primary cutaneous aspergillosis in an immunocompetant individual. J Eur Acad Dermatol Venerol 2006;20:738-9.
[Google Scholar]
|
| 5. |
Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, et al. Treatment of aspergillosis: Clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 2008;46:327-60.
[Google Scholar]
|
Fulltext Views
2,851
PDF downloads
2,116





