Translate this page into:
Cutaneous changes associated with prolonged plaster of Paris immobilization
Correspondence Address:
Joseph L Chongthu
Department of Orthopaedics, RIMS, Imphal, Manipur
India
| How to cite this article: Chongthu JL, Singh MA, Waikhom S, Khawlhring M. Cutaneous changes associated with prolonged plaster of Paris immobilization. Indian J Dermatol Venereol Leprol 2011;77:626 |
Sir,
Plaster of Paris (POP) immobilization is an accepted method of fracture management. [1] In a clinical study conducted between July 2008 and October 2009, in adult patients (n = 128, m:f = 3:2, 15-60 years) with limb immobilized in POP for ≥6 weeks (mean = 11 weeks), without pre-existing medical co-morbidities, skin lesion or known allergy to POP, we observed the cutaneous findings shown in [Table - 1]. Written informed consent from all participants and due ethical approval from the concerned authority was taken.
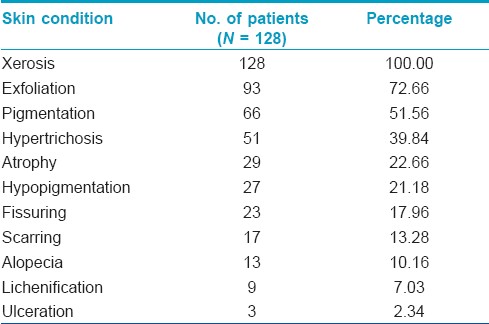
Data were analyzed for age and sex distribution of clinical findings. Xerosis was universally present. Skin exfoliation, pigment alteration (hyper/hypo) and hypertrichosis were equally distributed in all ages of both sexes without any significant regional difference. Skin atrophy, scarring, alopecia and ulcerations were however largely confined to the age group of 50-60 years which comprised 37.5% of the study population. Skin fissures were wholly confined to the soles and their incidence was 46.94% in all lower limb injuries. We could not find similar studies in the literature for an in-depth analysis and thereby to comment on the comparative statistical significance of our findings.
The skin is often subjected to unavoidable structural and physiological insult during injury and management of bony pathology because of its anatomical closeness. This may result in poor compliance to fracture management in cosmetically conscious patients.
The POP (Gypsum salt, CaSO 4 . H 2 O) hardens following an exothermic reaction after dipping in water, liberating some heat for a short period (5-10 min), the time depending on the product and water temperature. [1] This heat may add to the effect of initial hyperemia of injury, resulting in localized burns, vesicles and blisters leading to secondary bacterial infections of the raw skin surface resulting in atrophy and scarring [Figure - 1]a. The method and the casting materials used also affect such changes. [2],[3]
Padded POP immobilization alters and compromises the normal skin cycle and functions and/or leads to actual pathological changes. Xerosis and its sequelae (pruritus, exfoliation and fissuring) are common irrespective of age, sex and site [Figure - 1]b. Skin type, personal health and climatic conditions may also affect the severity. Pre-immobilization application of oil-based emollients has no long-term effects towards its prevention. Varying degree of pruritus experienced by all patients may be considered as a universally accepted associated problem.
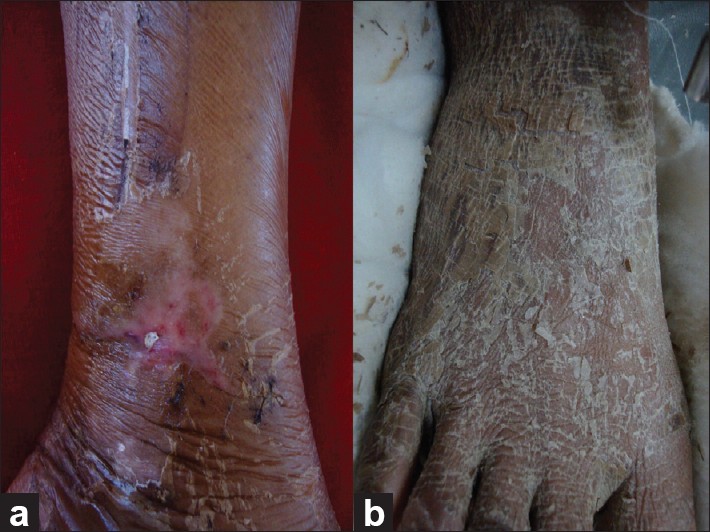 |
| Figure 1: (a) Skin atrophy and scarring. (b) Exfoliati |
Pigmentary changes and hypertrichosis [Figure - 2]a and b could be due to the increased vascularity as opined by others. [4] Warmth of insulated cotton padding may also enhance vascularity. Badly padded ill-fitting plaster and trapped foreign bodies result in irritation and pressure sores leading to localized abrasion, ulceration and scarring. [5] These combined effects can cause lichenification. These concealed complications finally result in unsightly appearance. [6] Plastering by an expert hand can avoid and reduce such problems of ill-fitting plasters.
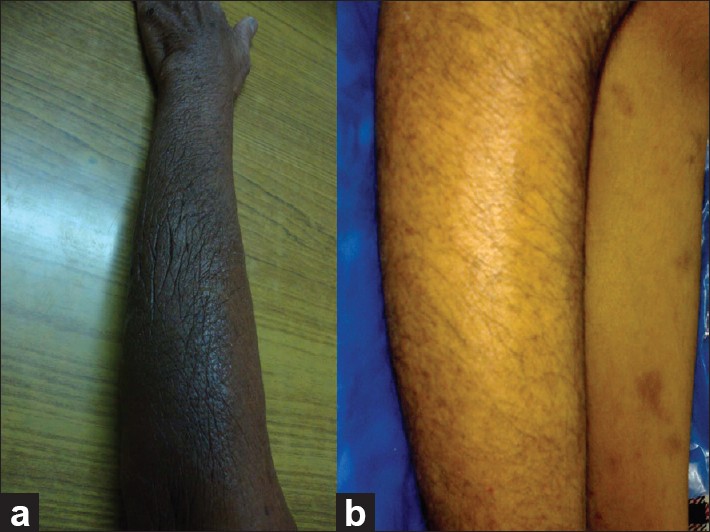 |
| Figure 2: (a) Hyperpigmentation of forearm. (b) Hypertrichosis of right leg |
Allergic reaction to the materials used is a possibility; however, no study subject showed any features. Such reaction can be detected early by regular examination of the skin at the proximal and distal margin of the plaster where all components of the materials used are in repeated direct contact with the skin. Newer fiber-cast products offer advantages in terms of lightness and water resistance, but cutaneous outcomes are unlikely to differ. Further study of pathological skin changes under the stress of plaster immobilization and innovative counter measures to such changes without compromise to the fracture immobilization may be considered.
Cutaneous self-limiting conditions that regress over time may not pose many problems in several patients, but management of the some cosmetically conscious individuals may pose a challenge. Adequate pre-casting counselling of the possible cutaneous outcomes and referrals to the concerned speciality for timely intervention should be advocated. This will definitely increase the patient′s compliance to the primary management. All our patients agreed to re-undergo the POP immobilization if required, and most readily accepted the cutaneous effects, while a few liked to avoid them as far as possible.
In the consideration of certain management regimens, treating patients as individuals with an integrated inter-speciality approach will definitely result in an anatomically, physiologically and aesthetically favourable and acceptable outcome as expected by the present-day demanding beneficiary.
| 1. |
Charnley J. The closed treatment of common fractures. Cambridge: Colt Books; 1999.
[Google Scholar]
|
| 2. |
Kaplan SS. Burns following application of plaster splint dressings. Report of two cases. J Bone Joint Surg Am 1981; 63:670-2.
[Google Scholar]
|
| 3. |
Halanski MA, Halanski AD, Oza A, Vanderby R, Munoz A, Noonan KJ. Thermal injury with contemporary cast application techniques and methods to circumvent morbidity. J Bone Joint Surg Am 2007;89:2369-77.
[Google Scholar]
|
| 4. |
Rathi SK. Localised acquired hypertrichosis following cast application. Indian J Dermatol Venereol Leprol 2007;73:367.
[Google Scholar]
|
| 5. |
Forni C, Zoli M, Loro L, Tremosini M, Mini S, Pirini V, et al. Cohort study of the incidence of heel pressure sores in patients with leg cast at the Rizzoli Orthopaedic Hospital and of the associated risk factors. Assist Inferm Ric. 2009;28:125-30.
[Google Scholar]
|
| 6. |
Halanski M, Noonan KJ. Cast and splint immobilization: Complications. J Am Acad Orthop Surg 2008;16:30-40.
[Google Scholar]
|
Fulltext Views
4,717
PDF downloads
2,102





