Translate this page into:
Cutaneous epithelioid angiosarcoma: A rare aggressive neoplasm
Correspondence Address:
Akshay Bali
Postgraduate, Department of Pathology, K.L.E University's Jawaharlal Nehru Medical College, Belgaum - 590 010
India
| How to cite this article: Mastiholimath RD, Bali A, Panduranga C, Roy M, Chavan R. Cutaneous epithelioid angiosarcoma: A rare aggressive neoplasm. Indian J Dermatol Venereol Leprol 2012;78:494-496 |
Sir,
Angiosarcomas are rare, vascular malignant neoplasms, comprising less than 1% of all sarcomas. [1] Epithelioid angiosarcoma (EA) is a rare, highly aggressive subtype of angiosarcoma that most commonly arises in the deep soft tissues. However, skin as a rare primary site is also described in literature. [2] We report a case of recurrent cutaneous epithelioid angiosarcoma located on the chest wall.
An 80-years-old female patient had presented with a swelling over the left side of the chest and enlarged left axillary lymph nodes 4 years ago. She underwent wide resection of the mass and left axillary lymph node clearance. Histopathological examination revealed sheets of large epithelioid cells with pronounced nuclear atypia and frequent atypical mitoses. A histopathological diagnosis of poorly differentiated metastatic carcinoma was rendered. She declined immunohistochemistry and was lost on follow-up. She did not receive any chemo/radiotherapy.
A year later, she came back with complaints of another similar swelling at the same site. On palpation, a hard, fixed, non-tender mass, 8 × 5.5 × 3 cm in dimension, with overlying skin showing hyperemia was noted on the left side of the chest below the clavicle [Figure - 1]a. Systemic examination and investigations including complete blood count, fasting blood sugar level, liver function test, and renal function test were within normal limits. Hepatitis B virus surface antigen and human immunodeficiency virus enzyme-linked immunosorbent assay were non-reactive.
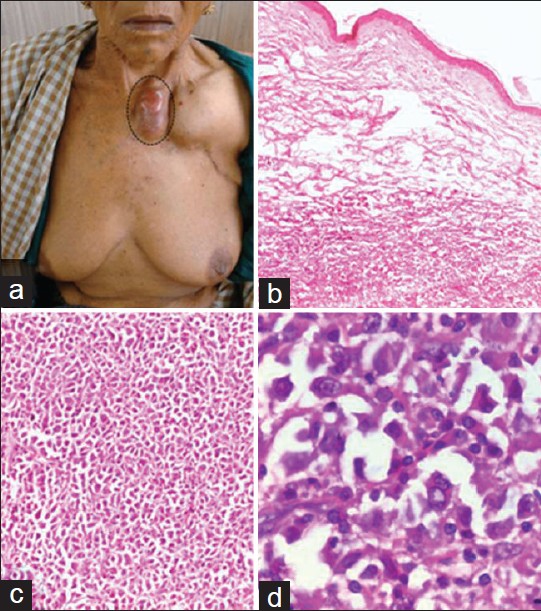 |
| Figure 1: (a) Clinical photograph showing a hard, fixed swelling on the left side of the chest wall below the clavicle. (b) Microscopy revealed a dermal neoplasm with extension into the subcutaneous tissue (H and E, ×40); (c) Lobules of neoplastic epithelioid cells in the dermis (H and E, ×100); d, Neoplasm composed of large pleomorphic oval or polygonal epithelioid cells with abundant, eosinophilic cytoplasm, and marked nuclear atypia (H and E, x400) |
Fine needle aspiration cytology of the mass revealed markedly atypical loosely cohesive clusters of large epithelioid cells with high nuclear/cytoplasmic ratio, vesicular irregular chromatin, conspicuous nucleoli and frequent atypical mitoses. A diagnosis of recurrent malignant tumor was offered, and biopsy was advised for definitive diagnosis. An attempt to achieve a wide resection of the tumor was unsuccessful as it extensively infiltrated the underlying subcutis, muscle and encased the subclavian vessels. Hence, only debulking of the tumor was undertaken and submitted for histopathological examination. Postoperatively, she refused to undergo radiotherapy treatment and requested to be discharged against medical advice.
Gross inspection revealed a grey-brown, irregular, partly skin covered, nodular mass, measuring 8 × 5.5 × 3 cm, with a solid, fleshy, lobulated cut surface showing focal areas of hemorrhage and necrosis. Microscopy revealed a malignant neoplasm in the dermis extending into the subcutaneous tissue, comprised of large round to polygonal epithelioid cells with abundant eosinophilic cytoplasm, central to eccentrically placed markedly pleomorphic vesicular nuclei and prominent nucleoli. The cells were arranged in lobules with a focal alveolar pattern. Mitosis, including atypical, amounting to 6-7 mitotic figures/10 high power field, and areas of hemorrhage and necrosis were evident. No obvious vasoformative areas were evident. [Figure - 1](b-d). Hence, a histopathogical diagnosis of possible epithelioid sarcoma with poorly differentiated metastatic carcinoma as a differential diagnosis was offered, and immunohistochemistry was advised for confirmation.
The tumor cells were immunoreactive for vimentin, CD31, pancytokeratin, EMA [Figure - 2] and negative for E-cadherin, smooth muscle actin, desmin, S100, Melan-A, HMB-45, myogenin, CD34. Based on the immunophenotypic features, the final diagnosis was concluded as EA.
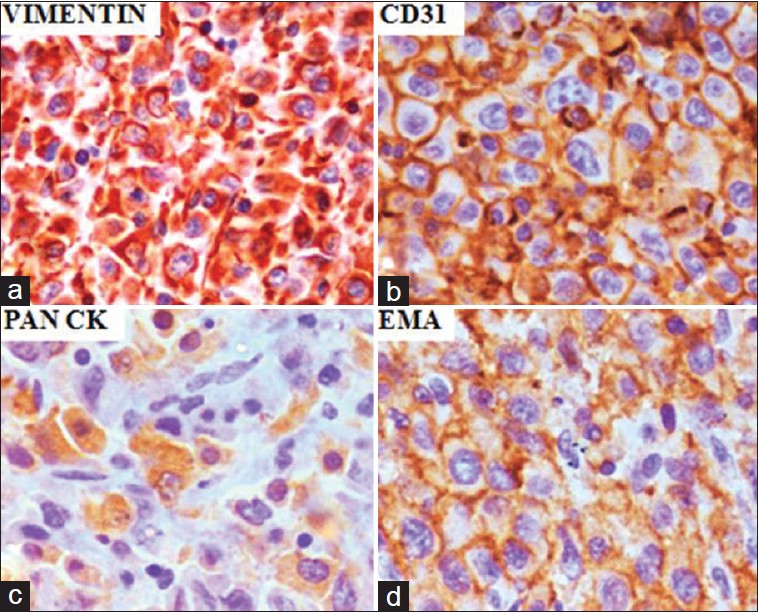 |
| Figure 2: Immunohistochemical staining: Neoplastic cells showing (a) strong and diffuse cytoplasmic positivity for vimentin (Vimentin, x400); (b) CD31 membranous immunostaining (CD 31, x400); (c) cytoplasmic positivity for cytokeratin (Pan CK, x400); (d) Membranous positivity for epithelial membrane antigen. (EMA, x400) |
Rosai and colleagues first described the epithelioid phenotype of angiosarcoma in 1976, which was later documented by Fletcher and colleagues in 1991. [3]
It most commonly occurs in deep soft tissue of the extremities, but a variety of other rare primary sites, including the skin, thyroid gland, adrenal glands, lungs and bones are also documented in the literature. [1] Bacchi et al.[4] reported the largest series of 18 cases of cutaneous EA and documented a predilection for elderly male with scalp being the commonest site.
Histologically, EA is characterized by large pleomorphic oval or polygonal epithelioid cells with abundant, eosinophilic cytoplasm, and marked nuclear atypia displaying a predominantly sheet-like growth pattern. [1] Some cells may exhibit intracytoplasmic vacuoles containing red blood cells. Atypical mitosis, varying degrees of hemorrhage and necrosis are readily observed. [1] Bacchi et al.[4] reported presence of occasional pseudoglandular or alveolar arrangement, which was observed in our patient as well. Immunostaining with vimentin shows strong and diffuse positivity. The endothelial markers, CD31 and Factor VIII, are positive in nearly 100% cases. CD34 positivity ranges from 40% to 100%, and pancytokeratin stains more than 35% of EA. [1],[4]
An epithelioid morphology, lack of obvious vasoformative foci and frequent cytokeratin positivity may lead to an erroneous diagnosis of poorly differentiated metastatic (or primary) carcinoma. [5] Histopathological features, helpful in distinguishing EA from poorly differentiated metastatic (or primary) carcinoma, include occasional intracytoplasmic vacuoles with or without red blood cells, anastomosing vascular channels and the lack of a desmoplastic reaction in the former. [1] Furthermore, strong immunoreactivity for vimentin, coupled with endothelial cell marker (Factor VIII, CD31, CD34), positivity renders the diagnosis of metastatic carcinoma unlikely. [1],[2] The other differential diagnostic possibilities include malignant mesothelioma, malignant melanoma, epithelioid peripheral nerve sheath malignancies, epithelioid sarcoma and epithelioid hemangioendothelioma. [1] In addition to subtle histological differences, a panel of immunohistochemical markers, including positive staining for vascular markers and negative immunostaining for HMB-45, Melan-A, calretinin, S 100, CD45, CD30 readily excludes these diagnostic mimickers. Less aggressive epithelioid hemangioendothelioma is differentiated from EA mostly based on the latter having a greater degree of cytologic atypia and atypical mitoses. [1]
EA is notorious for local recurrence and early metastases with mortality rates in excess of 50% after 3 years. [1] Treatment modalities commonly employed include surgical resection of the primary tumor and radiation therapy. [1] Angiographic embolization and radiotherapy can be used to control recurrent hemorrhages. [6]
In conclusion, cutaneous EA is a rare, aggressive, diagnostically challenging neoplasm that requires a high index of suspicion and panel of immunohistochemical markers to distinguish it from common mimickers like poorly differentiated metastatic (or primary) carcinoma, or malignant melanoma.
| 1. |
Hart J, Mandavilli S. Epithelioid angiosarcoma. Arch Pathol Lab Med 2011;135:268-72.
[Google Scholar]
|
| 2. |
Mobini N. Cutaneous epithelioid angiosarcoma: a neoplasm with potential pitfalls in diagnosis. J Cutan Pathol 2009;36:362-9.
[Google Scholar]
|
| 3. |
Fletcher CD, Beham A, Bekir S, Clarke AM, Marley NJ. Epithelioid angiosarcoma of deep soft tissue: A distinctive tumor readily mistaken for an epithelial neoplasm. Am J Surg Pathol 1991;15:915-24.
[Google Scholar]
|
| 4. |
Bacchi CE, Silva TR, Zambrano E, Plaza J, Suster S, Luzar B, et al. Epithelioid angiosarcoma of the skin: A study of 18 cases with emphasis on its clinicopathologic spectrum and unusual morphologic features. Am J Surg Pathol. 2010;34:1334-43.
[Google Scholar]
|
| 5. |
Prescott RJ, Banerjee SS, Eyden BP, Haboubi NY. Cutaneous epithelioid angiosarcoma: A clinicopathological study of four cases. Histopathology 1994;25:421-9.
[Google Scholar]
|
| 6. |
Barber WA, Scriven P, Turner D, Hughes D, Wyld L. Epithelioid angiosarcoma: Use of angiographic embolisation and radiotherapy to control recurrent haemorrhage. JSCR 2010; 5:7-10.
[Google Scholar]
|
Fulltext Views
3,887
PDF downloads
1,857





