Translate this page into:
Cutaneous manifestations in renal failure patients: A case series
Correspondence Address:
S Banerjee
Consultant Dermatologist, Skin Centre, Military Hospital, Jalandhar Cantt - 144005
India
| How to cite this article: Banerjee S. Cutaneous manifestations in renal failure patients: A case series. Indian J Dermatol Venereol Leprol 2007;73:106-108 |
Abstract
Cutaneous involvement in renal disease is due to a host of factors ranging from metabolic disturbances to immunosuppressive drugs. Herein we report a series of six cases of renal failure with varied cutaneous manifestations ranging from infections to neoplasms due to prolonged immunosuppression. Our first case had cutaneous cryptococcosis where skin lesions gave a clue to the diagnosis of altered sensorium and underlying meningitis. The second case initially presented with florid warts and was treated successfully but later presented with an explosive recurrence of skin lesions due to malignant transformation. Our third case had basal cell carcinoma over the presternal region that was successfully treated with liquid nitrogen cryotherapy. Our fourth case had diabetic nephropathy that presented with septicemia and purpura fulminans. The last case had cutaneous manifestations of drug therapy because of heparin infusion. To conclude, cutaneous manifestations in patients with renal failure are varied and a high degree of suspicion is needed for early diagnosis and aggressive treatment to effectively combat mortality and morbidity.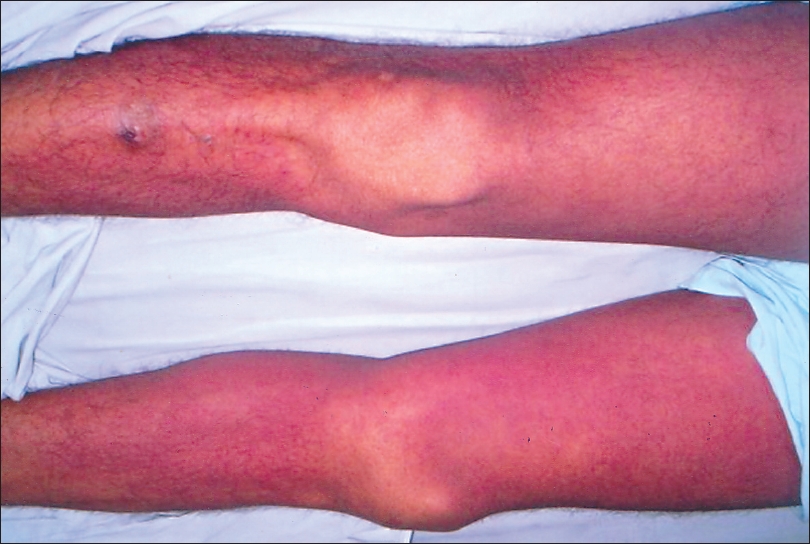 |
| Diffuse morbilliform erythematous rash due to heparin over both lower limbs in case 5 |
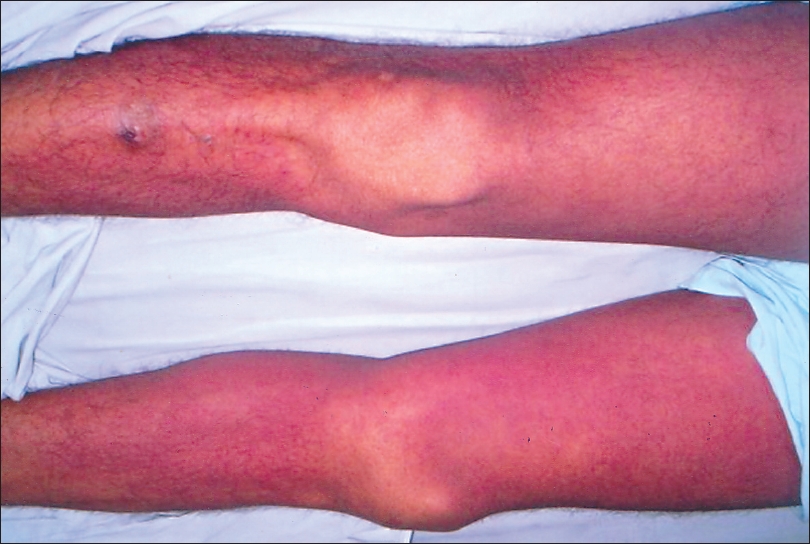 |
| Diffuse morbilliform erythematous rash due to heparin over both lower limbs in case 5 |
 |
| Multiple umbilicated nodules 0.5-2 cm with central necrosis over eyelids and face in case 1 |
 |
| Multiple umbilicated nodules 0.5-2 cm with central necrosis over eyelids and face in case 1 |
INTRODUCTION
Cutaneous involvement in renal disease is due to a host of factors ranging from uremia, metabolic disturbances and dialysis to the multitude of drugs used as immunosuppressive therapy in patients suffering from renal failure. Therefore, the cutaneous manifestations are varied, ranging from a multitude of skin infections to malignancies. Herein, we discuss five cases with cutaneous manifestations in patients with renal failure.
CASE REPORTS
Case 1: Disseminated cryptococcosis
An 18-year-old girl, a renal transplant recipient presented with severe headache and altered sensorium of two weeks duration. Physical examination revealed multiple (0.5-2 cm) umbilicated nodules with central necrosis on her face, eyelids, torso, arms and legs [Figure - 1]. Central nervous system (CNS) examination showed obtunded sensorium with evidence of meningeal irritation. A single lesion was lanced and a serosanguineous fluid sample was obtained. It showed encapsulated yeasts in India ink preparation, a finding also seen on cerebrospinal fluid (CSF) examination and blood culture. The patient was diagnosed as a case of disseminated cryptococcosis with involvement of the CNS.
She was treated with Inj. amphotericin B lipid complex (0.8 mg/kg/d) and intravenous fluconazole (200 mg bid). The patient failed to respond to the therapy and she succumbed to her infection after one week.
Case 2: Malignant transformation of condyloma acuminata
A 59-year-old male patient, a recipient of a renal transplant in December 1994 following chronic renal failure (CRF), presented with multiple verrucous outgrowths over the perianal region and inguinal fold of six months duration.
General and systemic examination revealed an obese individual with multiple verrucous sessile and pedunculated lesions with whitish moist surface over genital and inguinal folds suggestive of condyloma acuminata. He also had multiple itchy hyperpigmented papules and nodules over the trunk, which had a scaly surface with intermittent serosanguineous discharge suggestive of Kyrle′s disease. The patient was treated with cryotherapy and intralesional interferon resulting in complete remission of the genital lesions. Two months later, the patient had recurrence of the growth at the same site. This time the lesion was florid, measuring about 10 x 8 cm, rapidly progressive with a cauliflower-like appearance and the surface showed serosanguineous discharge and pinpoint bleeding. Subsequently, biopsy from the edge of the ulcer revealed evidence of squamous cell carcinoma (SCC). The patient was diagnosed as a case of SCC following malignant transformation of perianal warts and was further referred to an oncosurgeon for excision of the lesion.
Case 3 : Basal cell carcinoma
A 47-year-old male patient, a renal transplant recipient in May 2000 following chronic renal failure and maintained on oral immunosuppressive and cytotoxics (cyclosporin 100 mg bid, prednisolone 10 mg OD, azathioprine 100 mg OD, amlodipine 5 mg OD), presented with single raised hyperkeratotic verrucous lesion over the presternal region of six months duration. There was a history of insidious progression with intermittent serosanguineous discharge.
Clinical examination revealed a 5 x 4 cm sessile hyperpigmented keratotic plaque with peripheral raised rim and rolled margins. The surface showed shallow erosions with serosanguineous discharge and secondary impetiginizatio. Skin biopsy was consistent with keratotic basal cell carcinoma (BCC).
The patient was treated with cryosurgery using liquid nitrogen and a freeze-thaw cycle of two minutes till a peripheral rim of freezing was formed about 1 cm beyond the margin. The lesion showed complete resolution with scarring and no evidence of recurrence during follow-up.
Case 4: Purpura fulminans
A 56-year-female patient, an old case of non-insulin dependent diabetes mellitus (NIDDM) for the past 15 years along with diabetic renal failure, presented with intermittent high-grade fever along with a painful swelling and discoloration of both legs since three days.
Clinical examination revealed a febrile, toxic patient with localized massive ecchymosis over both lower limbs with sharp irregular geographic borders and surrounding zone of erythema along with hemorrhagic blebs. Investigations revealed azotemia with a blood urea of 143 mg%, serum creatinine of 3.5 mg/dl and blood sugar 350 mg%. Color doppler of lower leg veins and coagulation profile including prothrombin time, partial thromboplastin time with kaolin, and fibrin degradation products were deranged. The patient was diagnosed as a case of purpura fulminans with diabetic nephropathy.
The patient was treated with high dose broad-spectrum antibiotics, heparin infusion, insulin infusion and peritoneal dialysis with good clinical recovery.
Case 5: Heparin induced maculopapular rash
A 26-year-old male patient, a driver by profession, presented with acute renal failure following ingestion of ethylene glycol (engine coolant) along with neurological symptoms of altered sensorium and seizures. Investigations revealed azotemia with raised blood urea of 109 mg% and serum creatinine of 7.4 mg%. The patient was put on hemodialysis and on the third day, he developed a diffuse morbilliform erythematous rash over both lower limbs which was attributed to the unfractionated heparin used in the dialysate [Figure - 2]. The patient was treated with low molecular weight heparin and topical steroids resulting in subsidence of rash within seven days.
DISCUSSION
The sequelae of renal failure are complex and involve multiple systems. Moreover, renal transplantation has its own drawback due to prolonged and chronic immunosuppression leading to decreased immune surveillance and an increased susceptibility to infections, malignancy and drug effects. [1] The mucocutaneous lesions of cryptococcosis are protean ranging from molluscum contagiosum like umbilicated nodules, acneiform lesions, nodules, pustules and chancriform lesions. Recently, Schupbach et al reported five patients who were immunosuppressed presenting with disseminated cryptococcosis in the form of cellulitis and herpes-like vesiculation. [2] The treatment of disseminated disease consists of intravenous amphotericin B (0.7-1 mg/kg/day) with IV flucytosine (100 mg/kg/day) for two weeks followed by oral fluconazole (400 mg/day) for ten weeks.
Barr et al in 1989 studied 202 renal allograft recipients over a period of three years. [3] Almost 77% patients who had survived their grafts for more than five years, had viral warts showing significant epidermal dysplasia. These patients also showed evidence of cutaneous carcinomas with ratio of SCC to BCC being 15:1 with most of the SCC cases showing evidence of the presence of human papillomavirus (HPV) 5 and HPV8 DNA suggesting the etiological role of HPV in the development of cutaneous carcinoma. [3] These findings were later corroborated by Stockfleth et al . [4] Similarly, Rudlinger et al studied 120 renal transplant recipients and found 48% had warts, the incidence of which increased with the duration of immunosuppression although HPV DNA sequencing led to frequent detection of HPV1 and HPV3. [5]
Purpura fulminans is a group of widespread blood clotting disorders which are associated with a host of clinical conditions which may range from bacterial sepsis to extensive tissue damage, severe infections, obstetric complications, immune reactions, malignant disease and snake bites to giant hemangiomas. Uncontrolled activation of coagulation leads to thrombosis and the consumption of clotting factors leads to varied clinical manifestations. The skin lesions may range from massive ecchymosis with sharp irregular geographic borders and deep purple to blue or black gangrenous patches and, autoamputation along with bleeding from multiple sites. Coagulation studies are usually deranged with elevated fibrin degradation products while treatment consists of antibiotics, heparin, pentoxyphyllin to protein C in special circumstances.
The cutaneous side effects of heparin include alopecia, urticarial type I reaction, skin necrosis caused by vasculitis (type III Arthus reaction) and lipodystrophy at the injection site and rare reports of diffuse exanthema as in our case. [6] Therefore, LMWH and heparinoids (danaparoid) are being increasingly used due to their improved bioavailability, longer half life, predictable dose response and lower incidence of osteopenia and thrombocytopenia. [7] Most reactions are benign however discontinuation of treatment is recommended for type I reaction manifesting as cutaneous necrosis and thrombocytopenia.
Thus, cutaneous manifestations in renal failure patients can vary from infections to neoplasms. Their clinical course is usually more severe resulting in high morbidity or mortality. A high degree of suspicion is needed for early diagnosis and aggressive treatment, which would go a long way in reducing morbidity and mortality in renal failure.
| 1. |
Dreno B, Mansat E, Legoux B, Litoux P. Skin cancers in transplant patients. Nephrol Dial Transplant 1998;13:1374-9.
[Google Scholar]
|
| 2. |
Schupbach CW, Wheeler CE Jr, Briggaman RA, Warner NA, Kanof EP. Cutaneous manifestations of disseminated cryptococcosis. Arch Dermatol 1976;112:1734-40.
[Google Scholar]
|
| 3. |
Barr BB, Benton EC, Mclaren K, Bunney MH, Smith SW, Blessing K, et al . Human papilloma virus infection and skin cancers in renal allograft recipients. Lancet 1989;1:124-9.
[Google Scholar]
|
| 4. |
Stockfleth E, Nindl I, Stary W, Ulrich C, Schnook T, Meyer T. Human papillomaviruses in transplant associated skin cancer. Dermatol Surg 2004;30:604-9.
[Google Scholar]
|
| 5. |
Rudlinger R, Smith SW, Bunney MH, Hunter JA. Human papillomavirus infections in a group of renal transplant recipients. Br J Dermatol 1986;115:681-92.
[Google Scholar]
|
| 6. |
Havenburg J, Hunle G, Wang L, Hoffmann U, Bayerl C, Kerowgan M. Association of heparin induced skin lesions, intracutaneous tests and heparin induced IgG. Allergy 1999;54:473-7.
[Google Scholar]
|
| 7. |
Aguilar D, Goldhaber SZ. Clinical uses of low-molecular-weight heparins. Chest 1999;115:1419-23.
[Google Scholar]
|
Fulltext Views
3,584
PDF downloads
3,907





