Translate this page into:
Cutaneous metastasis from salivary duct carcinoma: A rare case and review of literature
Corresponding author: Prof. Sujay Khandpur, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. sujay_khandpur@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Pangti R, Khan I, Mridha AR, Khandpur S. Cutaneous metastasis from salivary duct carcinoma: A rare case and review of literature. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_774_2023
Dear Editor,
Salivary duct carcinoma is a rare, highly aggressive malignancy arising most commonly from the excretory duct of the parotid salivary gland and carries a poor prognosis. It is associated with a high rate of distant metastasis, but cutaneous metastasis is extremely rare. Salivary duct carcinoma and breast ductal carcinoma have a similar histopathological and immunophenotypical profile with positivity for androgen receptor, carcinoembryonic antigen and rarely human epidermal growth factor receptor 2 overexpression. Histologically, salivary duct carcinoma shows intraductal invasion, cribriform cell nest formation and comedonecrosis.1 This case highlights the rare cutaneous metastasis from a salivary duct carcinoma occurring in a middle-aged man.
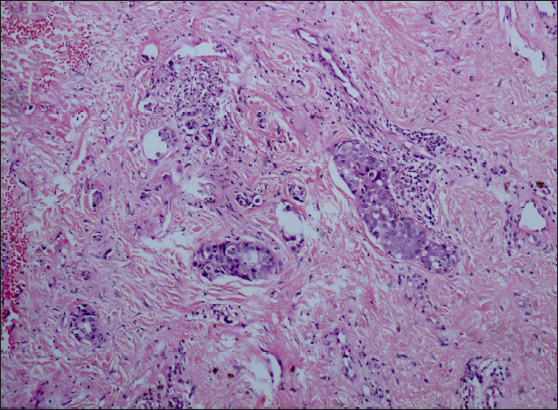
A 56-year-old man initially presented to the otorhinolaryngology department approximately 14 months ago with the complaint of an asymptomatic, progressively enlarging swelling on the left parotid gland, which had been evident for the preceding 2 months. Subsequent histopathological examination yielded a diagnosis of salivary duct carcinoma, specifically the adenocarcinoma subtype, along with evidence of extra nodal extension. Immunohistochemical analysis revealed positive markers for cytokeratin 7 (CK7) and Her2/neu. As part of the management, he underwent a total conservative left parotidectomy along with a modified radical neck dissection. Following the surgical intervention, 2 months later, he was started on radical radiotherapy. This radiotherapy regimen employed the simultaneous integrated boost-volumetric modulated arc therapy (SIB-VMAT) technique with a cumulative dose of 66 Gy administered over 33 fractions spanning 6.5 weeks, along with an additional 50 Gy administered over 25 fractions during a 5-week period. Upon the conclusion of his radiotherapy treatment, the patient exhibited the emergence of cutaneous manifestations within the irradiated field, prompting a referral to the dermatology department for further evaluation. Dermatological assessment revealed a well to ill-defined erythematous to purpuric plaque measuring 20 × 10 cm situated on the anterior and lateral aspects of the neck and upper chest with the left side more prominently affected than the right. Notably, the plaque displayed areas of superficial yellowish-white scale-crust and multiple whitish-yellow papules distributed across its surface. Importantly, the central portion of the plaque exhibited greater firmness compared to its periphery [Figure 1]. On dermoscopy, diffuse erythema in the background with yellowish globules and areas of blood vessels/telangiectasias in the periphery were noted [Figure 2]. Skin biopsies from two different sites on the plaque showed small and large nests of atypical tumour cells infiltrating the superficial and deep dermis. Large dermal lympho-vascular tumour emboli were seen [Figures 3a to 3c]. Immunohistochemistry (IHC) as similar to the primary tumour with diffuse cytoplasmic positivity for (CK7) and strong (3+) membranous positivity for Her2/neu [Figures 4a to 4d]. CK7 positivity has been found to be significantly higher in metastatic salivary gland carcinomas as compared to squamous cell carcinoma. Up to 80% of the patients with salivary duct carcinoma have been found to be positive for Her2/neu, which suggests the aggressive nature of the condition. Histopathological mimickers like dermal duct tumour were ruled out owing to the absence of ducts, poroid clear cells, and the presence of significant atypia. Metastasis from other sources was ruled out owing to a similar histopathology and IHC to the primary tumour. Thus, a diagnosis of cutaneous metastasis from salivary duct carcinoma was made. He was counselled regarding the poor prognosis and referred to medical oncology for palliative management.

- Erythematous to purpuric plaque over the anterior and lateral aspects of neck and upper chest with areas of superficial, yellowish-white scale-crust and multiple whitish-yellow papules.
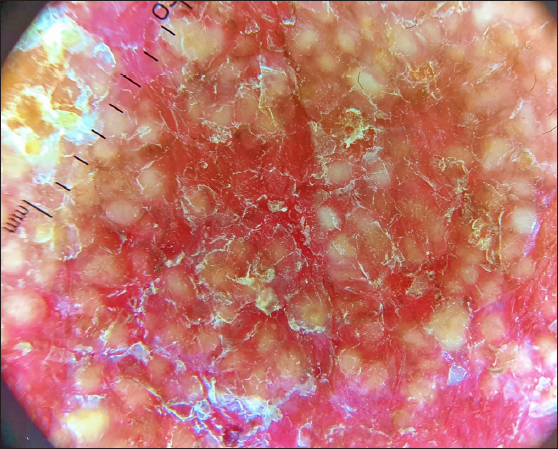
- Polarised Dermoscopy showing diffuse erythema in the background with yellowish globules (10x).
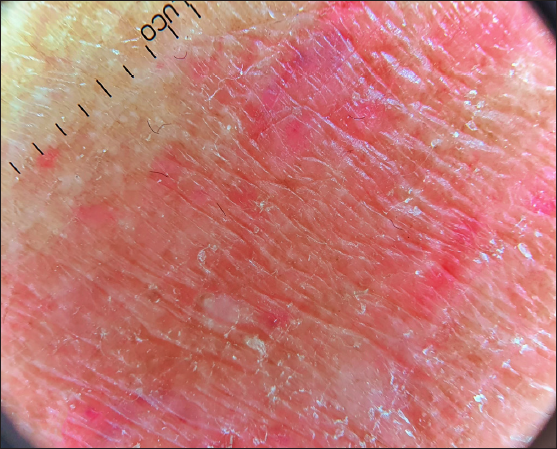
- Dermoscopy showing areas of blood vessels/telangiectasias in the periphery.
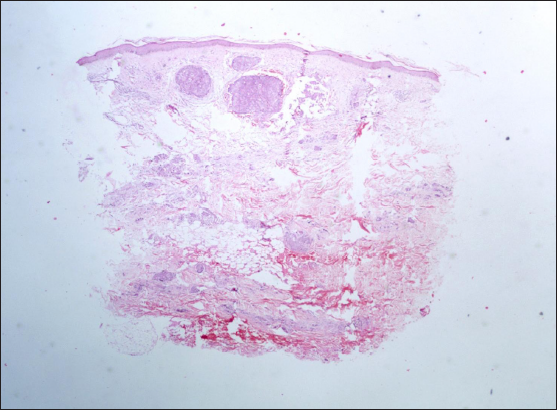
- Photomicrographs from biopsies of the chest plaque showing infiltration of superficial and deep dermis by nests of atypical cells along with lympho-vascular emboli (Haematoxylin & Eosin, 20x).
- Photomicrographs from biopsies of the chest plaque showing nests of atypical cells infiltrating between collagen bundles (Haematoxylin & Eosin, 100x).
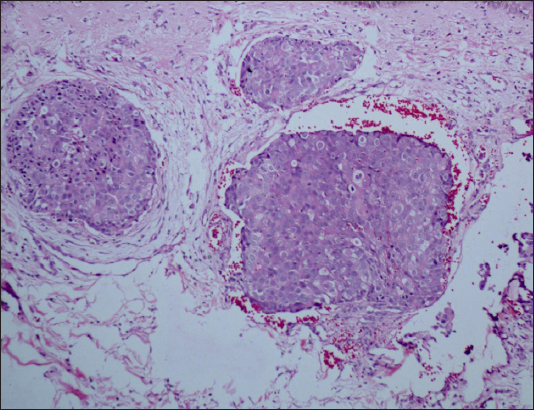
- Photomicrographs from biopsies of the chest plaque showing dermal lympho-vascular channels with tumour emboli (Haematoxylin & Eosin, 200x).
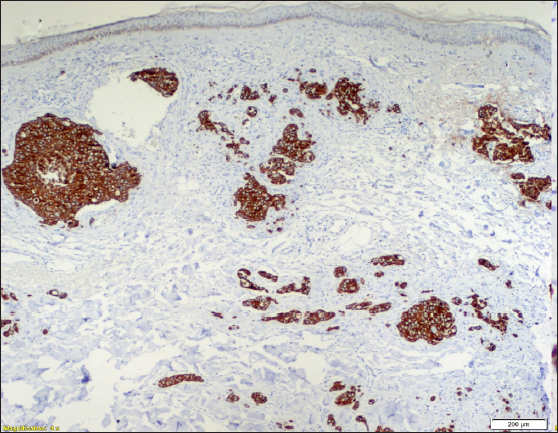
- Photomicrographs from biopsies of the chest plaque showing diffuse cytoplasmic positivity with CK-7 (40x).
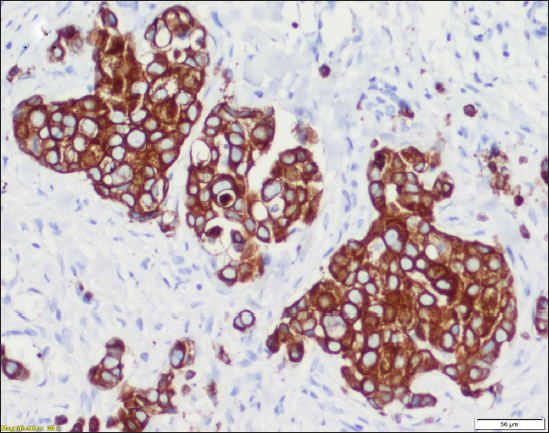
- Photomicrographs from biopsies of the chest plaque showing diffuse cytoplasmic positivity with CK-7 (200x).

- Photomicrographs from biopsies of the chest plaque showing strong (3+) membranous positivity with Her2/neu (100x).
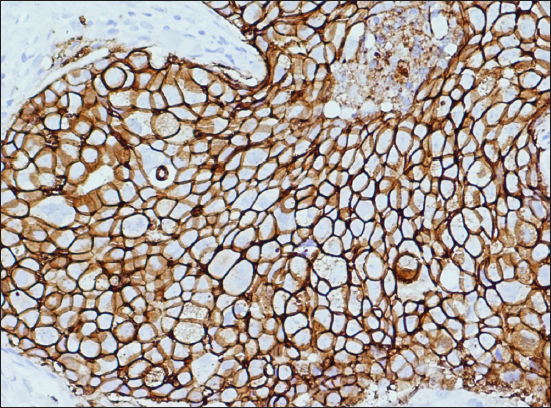
- Photomicrographs from biopsies of the chest plaque showing strong (3+) membranous positivity with Her2/neu (200x).
Cutaneous metastasis accounts for approximately 10% of distant metastatic occurrences originating from internal malignancies such as breast, large intestine, ovary, lungs and kidney.2 These skin metastases can manifest in a diverse array of clinical appearances, including firm papules or nodules, subcutaneous nodules, erythematous plaques, ulcers, hair loss (referred to as alopecia neoplastica), and in some cases, they may mimic various dermatological conditions such as granuloma annulare, pyogenic granuloma, acute paronychia, varicella-zoster, scleroderma, epidermoid cysts, keratoacanthoma and more.
Salivary duct carcinoma is a rare and highly aggressive malignancy, most frequently originating from the parotid gland, followed by the submandibular gland and other minor salivary glands. Salivary duct carcinoma carries a substantial risk of metastasizing to various organs, albeit skin metastasis being an exceptionally rare occurrence. To date, only ten documented cases of cutaneous metastasis from salivary duct carcinoma exist in the medical literature. The clinical presentations resembled radiation recall dermatitis,3 basal cell carcinoma,4 telangiectatic lesions5 or carcinoma haemorrhagiectoides with some cases displaying a distinctive ‘shield sign’ in which the skin metastasis resembled the shield of a medieval knight on the chest.6
In our case, the initial working diagnoses included cutaneous metastasis (often referred to as carcinoma en cuirasse) and chronic radiation dermatitis. However, histopathological examination confirmed the diagnosis of cutaneous metastasis of the adenocarcinoma subtype from the salivary duct carcinoma. Latter is indicative of an unfavourable prognosis with a 5-year survival rate of approximately 43%.7
It is essential to underscore the significance of recognising cutaneous metastasis as the primary or concurrent presentation of an underlying systemic malignancy, as early detection and intervention are crucial.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Cancers of the major salivary gland. J Oncol Pract. 2018;14:99-108.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous metastases of internal malignancies: A single‐institution experience. Histopathology. 2022;81:329-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A Case of Cutaneous Metastases of salivary duct carcinoma mimicking radiation recall dermatitis. Ann Dermatol. 2020;32:436-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous metastases from salivary duct carcinoma of the submandibular gland. Case Rep Dermatol. 2017;9:254-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Telangiectatic metastasis from ductal carcinoma of the parotid gland. J Am Acad Dermatol. 1993;28:113-4.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous Metastatic Cancer: Carcinoma hemorrhagiectoides presenting as the Shield Sign. Cureus. 2021;13:e12627.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- SEER*Explorer: An interactive website for SEER cancer statistics. Surveillance Research Program, National Cancer Institute; 2023 Apr 19 [accessed on 2024 Feb 5]. Available from: https://seer.cancer.gov/statistics-network/explorer/





