Translate this page into:
Cutaneous myeloid sarcoma- Deciphering clinical clues
Corresponding author: Dr. Neha Taneja, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. taneja.neha2908@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mehta N, Ahuja R, Patel V, Arava S, Taneja N. Cutaneous myeloid sarcoma - Deciphering clinical clues. Indian J Dermatol Venereol Leprol. 2025;91:388-90. doi: 10.25259/IJDVL_1392_2023
Dear Editor,
A 22-year-old lady presented with sudden onset asymptomatic reddish raised lesions on the face, abdomen, legs and genitalia of 3 weeks duration. The lesions started from the cheeks and rapidly progressed to involve the other sites over a week. The patient also had low-grade fever, night sweats, loss of appetite and significant weight loss. On examination, there were multiple firm erythematous discrete and coalescent plaques and nodules on the face, abdomen and legs [Figure 1a]. There was a prominent violaceous hue, especially in the plaques on the cheeks [Figure 1b]. Oral cavity showed similar nodules on lips with gingival hypertrophy and haemorrhagic plaques on the mucosa [Figure 1c]. There was a diffuse indurated swelling on the labia and clitoris [Figure 1d]. Additionally, there were annular scaly plaques on bilateral flexural aspect of the thighs suggestive of tinea cruris. There were multiple firm non-tender significantly enlarged cervical lymph nodes on both sides. Systemic examination showed no organomegaly. A complete hemogram showed initial leukocytosis followed by a leukemoid reaction and total counts increased rapidly from 20000 to 60000 over 1 week (with 85% blasts). Lactate dehydrogenase level was 6980 IU/L. Skin biopsy showed a dense diffuse dermal infiltrate beneath a well-formed Grenz zone with areas of Indian file arrangement composed of large lymphoid cells with hyperchromasia, mitotic figures and crush artefacts [Figure 2a]. On immunohistochemistry, the leukemic cells were positive for myeloid markers including CD13, CD33, CD117 [Figure 2b] and myeloperoxidase. With a diagnosis of myeloid sarcoma, the patient was further investigated for acute myeloid leukaemia (AML) and started on chemotherapy (Cytarabine and Daunorubicin). Although a magnetic resonance imaging of the central nervous system was planned, but it could not be done as her condition deteriorated rapidly and succumbed to her disease over the next 10 days.

- Firm erythematous plaques and nodules on face leading to a deformed appearance.
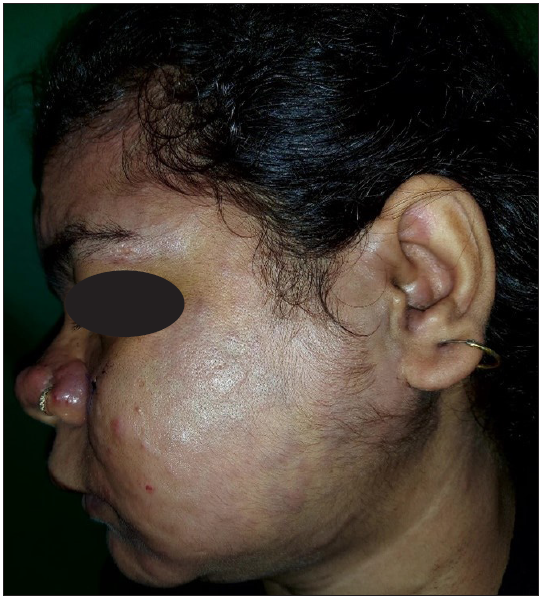
- Violaceous hue in plaques on the cheek.
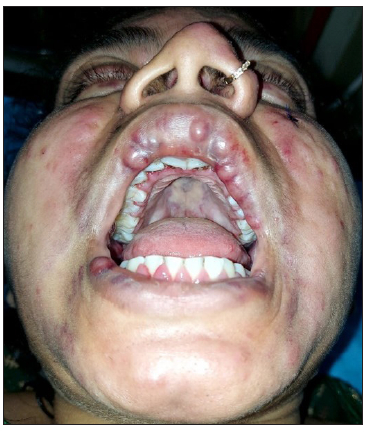
- Gum hypertrophy, mucosal nodules and haemorrhagic plaques.

- Diffuse indurated plaques on the vulva.
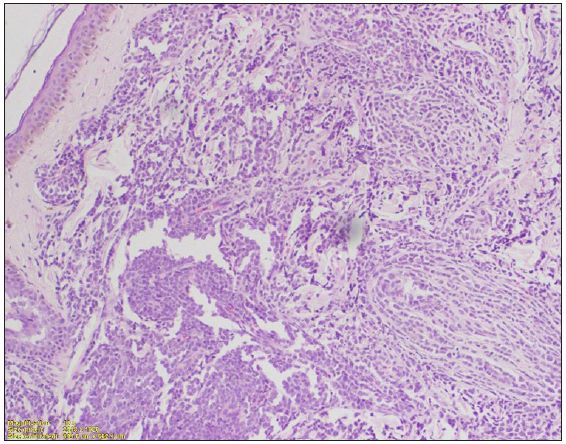
- Dense diffuse dermal infiltrate beneath a well-formed grenz zone, with areas of Indian file arrangement. Infiltrate is composed of large lymphoid cells with hyperchromasia, mitotic figure and crush artefacts. (Haematoxylin and eosin, 100x).
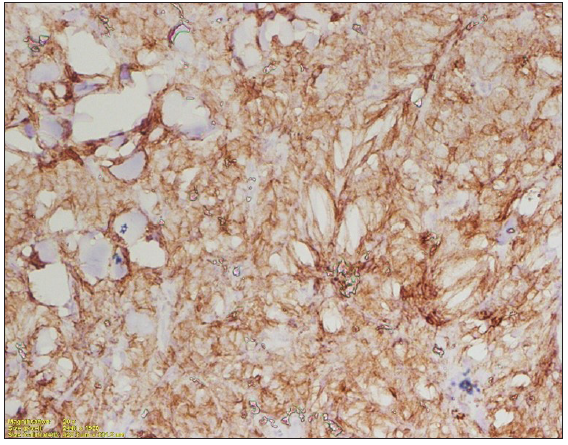
- Special stains positive for myeloid lineage in immunohistochemistry (CD117, membranous staining, 200x).
Myeloid sarcoma is the extramedullary infiltration of myeloid cells in AML and rarely in other myeloproliferative disorders. It commonly presents with or after the diagnosis of AML but can infrequently present in isolation.1 Isolated myeloid sarcoma patients frequently fulfil other criteria for AML diagnosis later, hence isolated myeloid sarcoma needs to be treated as AML.2 About 3–4% of AML cases show myeloid sarcomas, especially those with monoblastic or myelomonocytic differentiation (AML-M4 and AML-M5 subtypes of French-American-British classification) and relapsed cases.3 Extramedullary involvement is most commonly seen in the skin, where it can also be termed as leukaemia cutis. In the skin, it presents as erythematous to violaceous papules, nodules and plaques on the trunk, upper extremities, and/or head and neck in elderly patients.4 The lesions are characterised by a greenish hue, hence also termed chloroma, due to the activity of myeloperoxidase enzymes. Cutaneous myeloid sarcoma is frequently associated with gingival hyperplasia and central nervous system involvement. This may portend a poor prognosis, although there is conflicting evidence regarding this in the literature.3,5
Facial papules and nodules have a wide variety of differentials and generally end up requiring a biopsy. While the lepromatous spectrum of leprosy can also present with fever, lymphadenopathy and tender firm nodules and plaques (in type-2 reaction), the significant weight loss, the violaceous hue and the haemorrhagic plaques on the mucosa favoured an underlying malignancy. Other infiltrative disorders including Crohn’s (vulvar and extragenital) and orofacial granulomatosis (along with granulomatous vulvitis) have a more indolent course and often lack B-symptoms. On histological evaluation, the presence of non-caseating epithelioid cell granulomas is noted.6 In our patient, sudden onset, presence of B-symptoms, violaceous hue, mucosal involvement, firm consistency leading to a deformed appearance and significant lymphadenopathy were clinical pointers towards myeloid sarcoma. Such patients need rapid confirmation of diagnosis and chemotherapy, as they can decline rapidly within a few days. A good clinical history and examination can prompt this urgency even before the investigations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Myeloid sarcoma, chloroma, or extramedullary acute myeloid leukemia tumour: A tale of misnomers, controversy and the unresolved. Blood Rev. 2021;47:100773.
- [CrossRef] [PubMed] [Google Scholar]
- Myeloid Sarcoma: Current Approach and Therapeutic Options. Ther Adv Hematol. 2011;2:309-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Leukaemia Cutis: Clinical Features and Outcomes of 56 Patients. Acta Derm Venereol. 2022;102:adv00647.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association of Leukemia Cutis With Survival in Acute Myeloid Leukemia. JAMA Dermatol. 2019;155:826-32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Granulomatous cheilitis with granulomatous vulvitis: A rare association. Indian J Dermatol Venereol Leprol. 2013;79:799-801.
- [CrossRef] [PubMed] [Google Scholar]





