Translate this page into:
“Degeneration” in Dermatopathology
Corresponding author: Dr. Abhishek R. Parekh, Dermatology, Venereology and Leprosy, Baroda Medical College, Anandpura, Baroda-390001, India. om10abhi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Parekh AR, Shah HA. “Degeneration” in Dermatopathology. Indian J Dermatol Venereol Leprol 2023;89:916-22.
Degeneration is derived from the Latin word “degenerare,” which means to decline in quality.1 It is a process by which a tissue deteriorates and loses functional activity due to some injurious stimulus and may become converted into or replaced by other kinds of tissue. It is seen in many inflammatory, infective, drug-induced and neoplastic skin conditions. This article aims to enumerate and briefly describe the degeneration in dermatopathology which will be beneficial to residents. To simplify, degeneration in dermatopathology can be classified as follows [Figure 1]
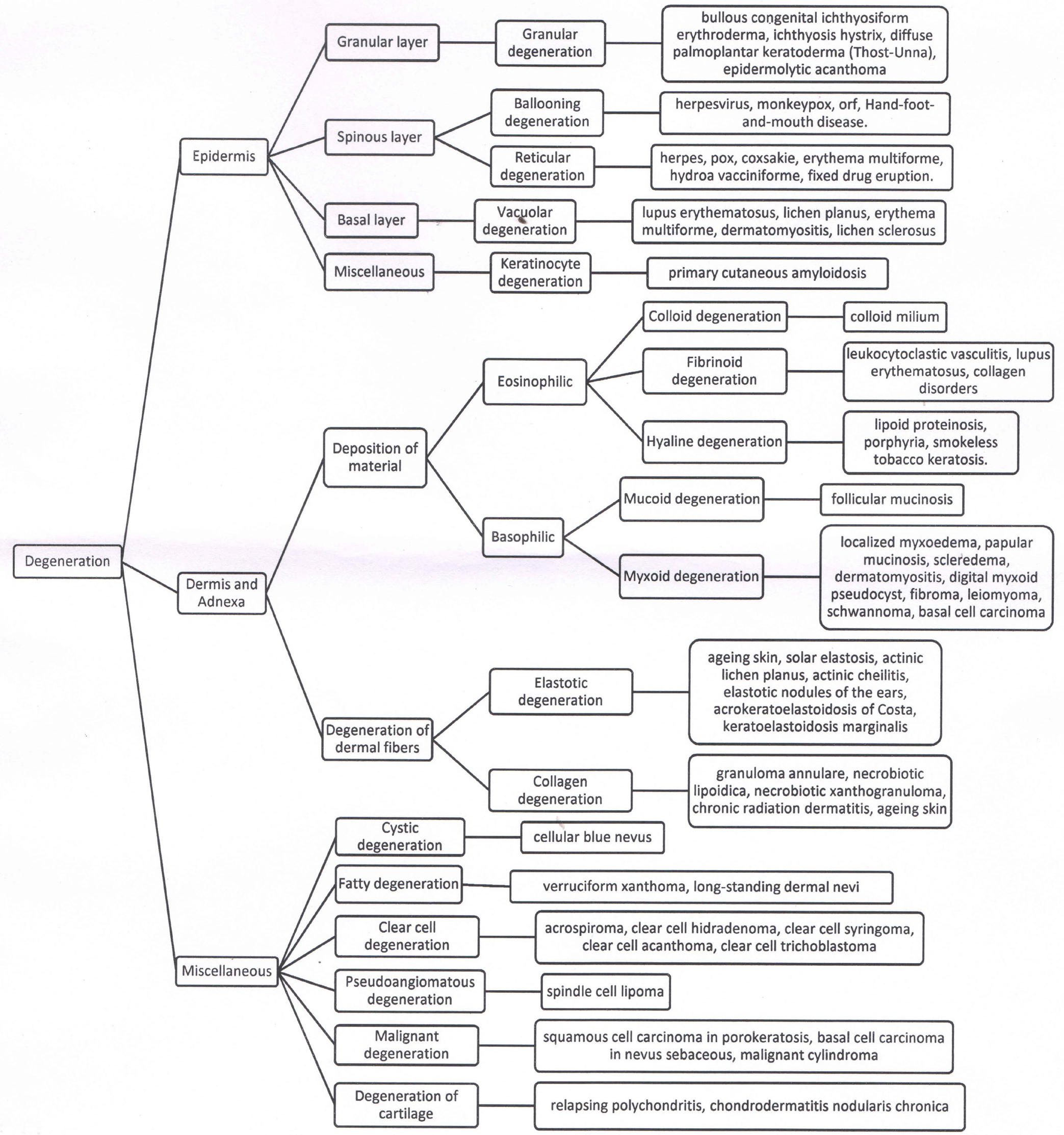
Algorithm for “Degeneration in Dermatopathology”
Degeneration in epidermis
Degeneration in dermis and adnexa
Miscellaneous degeneration
-
Degeneration in Epidermis:
-
Keratinocyte degeneration in the granular layer
Granular degeneration:
Here, keratinocytes exhibit an increase in keratohyalin granules, perinuclear vacuolization and feathery cell margins.2 This form of degeneration is also referred to as epidermolytic hyperkeratosis because all of these alterations take place in conjunction with clearly visible orthohyperkeratosis.2 It is seen in bullous congenital ichthyosiform erythroderma [Figure 2], ichthyosis hystrix, diffuse palmoplantar keratoderma (Thost-Unna) and epidermolytic acanthoma.2 Mutations in keratin 1 and 10, which are expressed in suprabasal keratinocytes, are thought to cause granular degeneration by weakening the keratinocytes and causing vacuolar changes in the upper layers of the epidermis.3
-
Keratinocyte degeneration in the spinous layer
-
Ballooning degeneration:
In ballooning degeneration, keratinocytes appear swollen, pale and round due to intracellular oedema and loss of intercellular bridges.2 It is observed in virus disorders affecting epithelia, such as herpesvirus, monkeypox, orf and hand-foot-and-mouth disease.3 It is the result of cytopathic effect of virus on keratinocytes. In herpes virus infection, affected cells aggregate to form a multinucleated cell with nuclear moulding and chromatin margination [Figure 3].2
-
Reticular degeneration:
As the ballooning degeneration progresses, the rupture of inflated keratinocytes results in the formation of round, vast intracellular spaces separated by remnants of the cellular wall. Because this epidermal pattern resembles a net, it is known as reticular degeneration.4 Though this pattern is most common in viral illnesses such as herpes, hand-foot-and-mouth disease [Figure 4], pox and coxsackie, it can also be present in non-infectious conditions such as erythema multiforme, hydroa vacciniforme and fixed drug eruption.4 It is also seen in tissues sent for histological examination after electrofulguration.
-
-
Keratinocyte degeneration in the basal layer
Vacuolar degeneration:
It is also known as hydropic degeneration or liquefactive degeneration. Damage to the basal layer of the epidermis leads to the formation of vacuoles within the basal keratinocytes.2 A more severe process may lead to necrosis of keratinocytes and subsequently subepidermal blister formation. Though it can be seen in both vacuolar and lichenoid interface dermatitis, it is more visible in the former. In the latter, it is obscured by a band of lymphocytes.5 It is seen in lupus erythematosus [Figure 5], lichen planus, erythema multiforme, dermatomyositis and lichen sclerosus.2
-
Miscellaneous
Degeneration of keratin intermediate filaments has been observed in primary cutaneous amyloidosis under the electron microscope.6 In sections stained with haematoxylin & eosin (H&E), amyloid appears as amorphous eosinophilic material in the papillary dermis [Figure 6].1,2
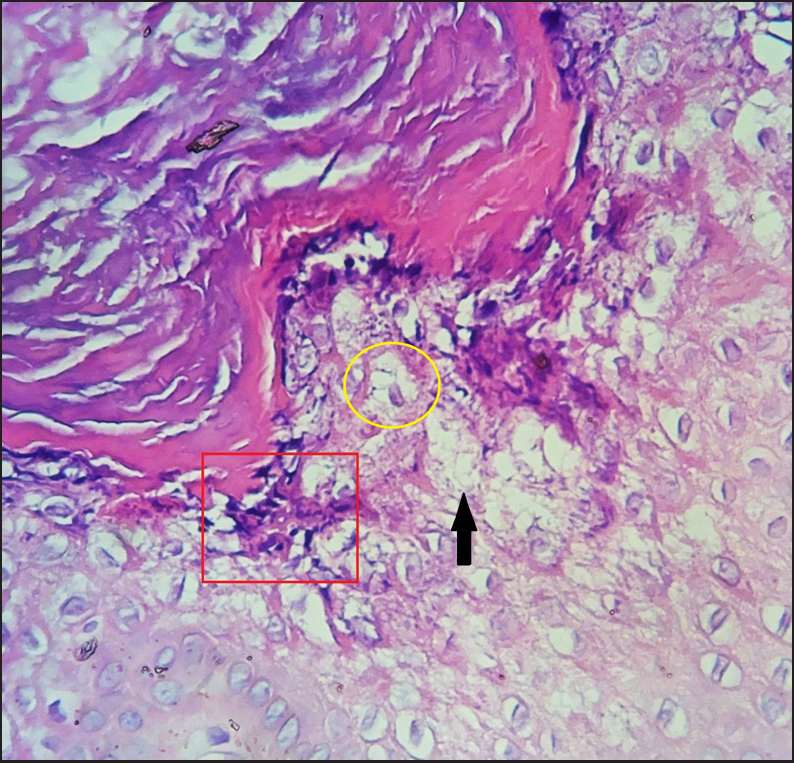 Figure 2
Figure 2- Granular degeneration in bullous congenital ichthyosiform erythroderma showing increased keratohyaline granules (red square), perinuclear vacuolization (yellow circle) and feathery cell margins (black arrow) (H and E, 400x)
 Figure 3
Figure 3- Ballooning degeneration in herpes virus infection (H and E, 100x). Inset image showing ballooned keratinocytes (red arrow), multinucleate giant cells with nuclear molding and margination of chromatin (yellow circle) (H and E, 400x)
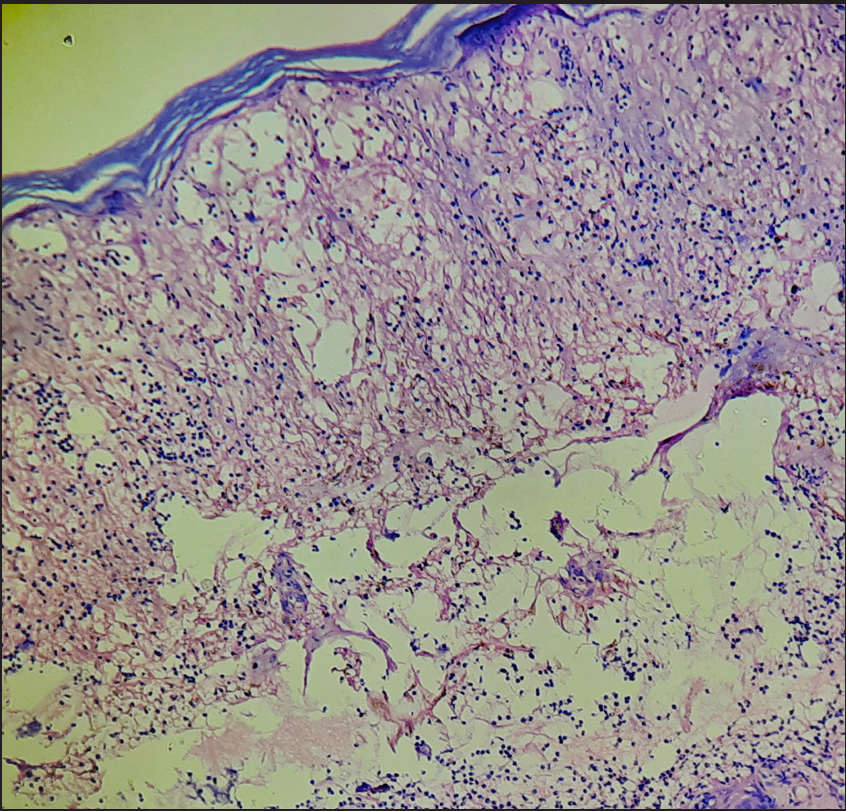 Figure 4
Figure 4- Reticular degeneration in hand-foot-mouth-disease (H and E, 100x)
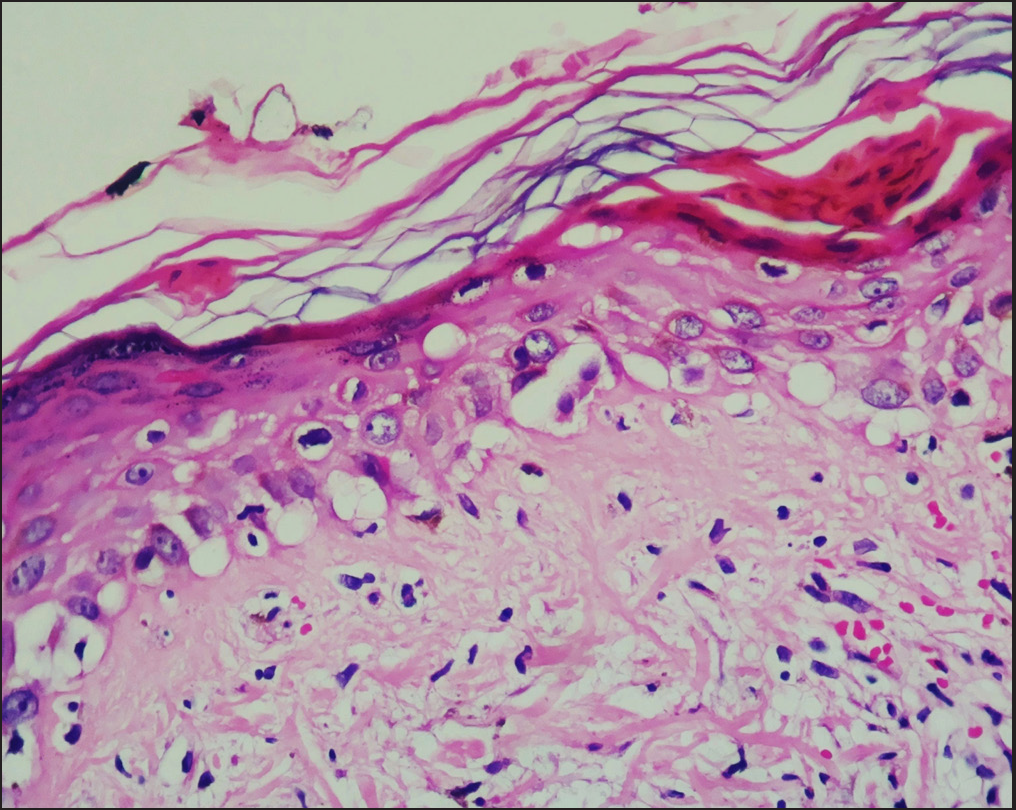 Figure 5
Figure 5- Vacuolar degeneration of the basal layer in lupus erythematosus (H and E, 400x)
-
-
Degeneration in Dermis and Adnexa:
-
Degeneration with deposition of material
-
1a)
Eosinophilic material
-
Colloid degeneration:
It refers to the deposition of extracellular, homogeneous, gelatinous material of varying composition.2 Typically seen in colloid milium [Figure 7], it may also be found in certain epithelial tumours.2 Prolonged exposure to sun is thought to be the probable etiological factor for colloid degeneration.7
-
Fibrinoid degeneration:
It refers to the deposition of eosinophilic, granular or fibrillary material in the vessel walls or collagen bundles.2 This fibrin-like material is made up of fibrinogen, plasma proteins or immunoglobulins.2 It is seen in leukocytoclastic vasculitis [Figure 8], lupus erythematosus and collagen disorders.2 In leukocytoclastic vasculitis, circulating immune complexes are deposited in the vessel wall and activate complement system, which results in chemotaxis of neutrophils and further activation of clotting system, leading to conversion of fibrinogen to fibrin.2
-
Hyaline degeneration:
It refers to the presence of amorphous, eosinophilic, PAS (periodic acid-Schiff) ve degenerative material in dermal connective tissue.2 It is seen in porphyria, lipoid proteinosis [Figure 9] and smokeless tobacco keratosis.2 Deposition of hyaline material is due to the defect in heme biosynthesis pathway in porphyria; while in lipoid proteinosis, it is due to mutation in ECM1, a gene regulating skin homeostasis.2 The term “hyaline degeneration” should only be used if deposited substance cannot be classified under other degenerations.8
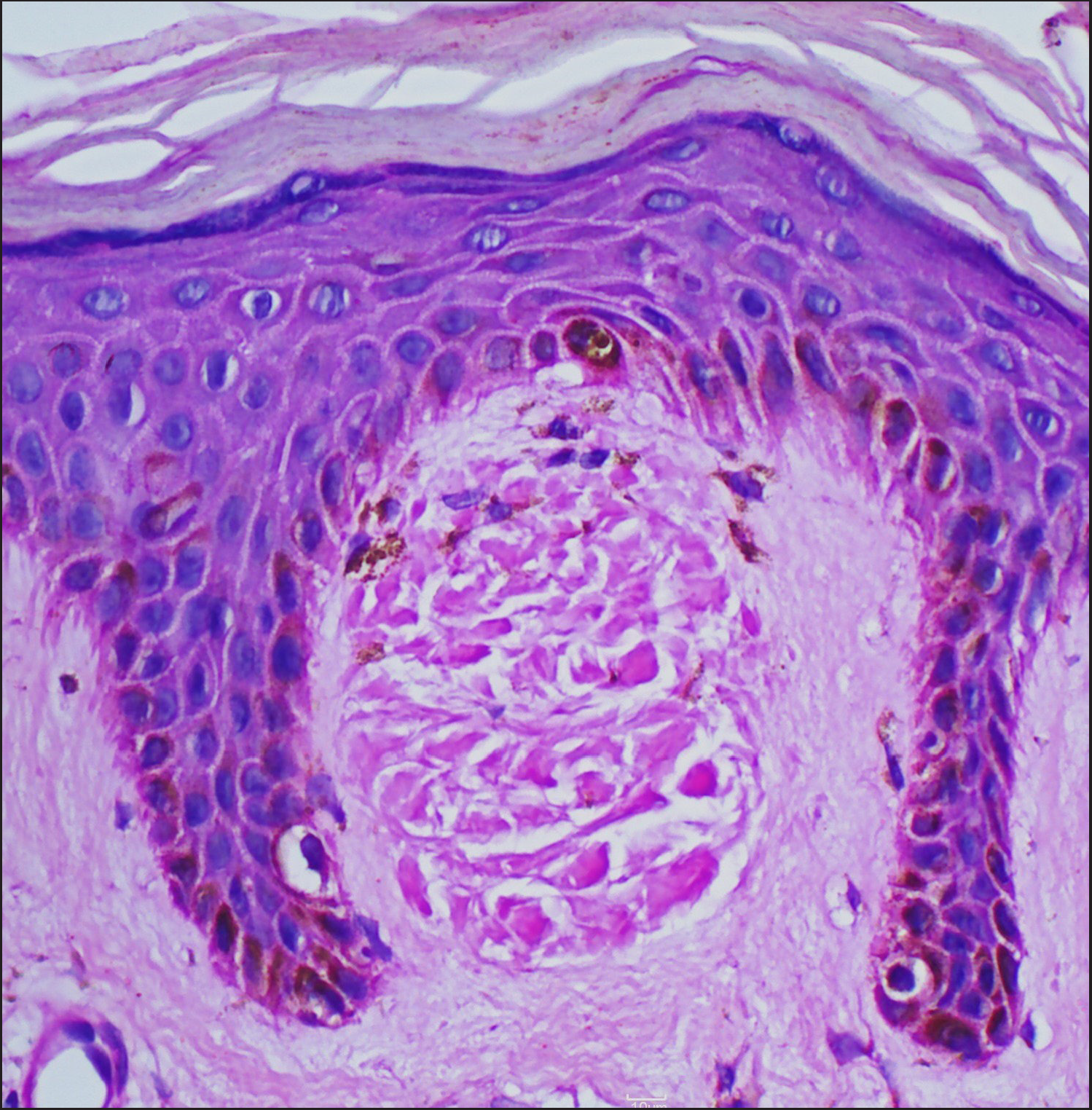 Figure 6
Figure 6- Primary cutaneous amyloidosis showing deposition of amorphous, eosinophilic material in widened papillary dermis (H and E, 400x)
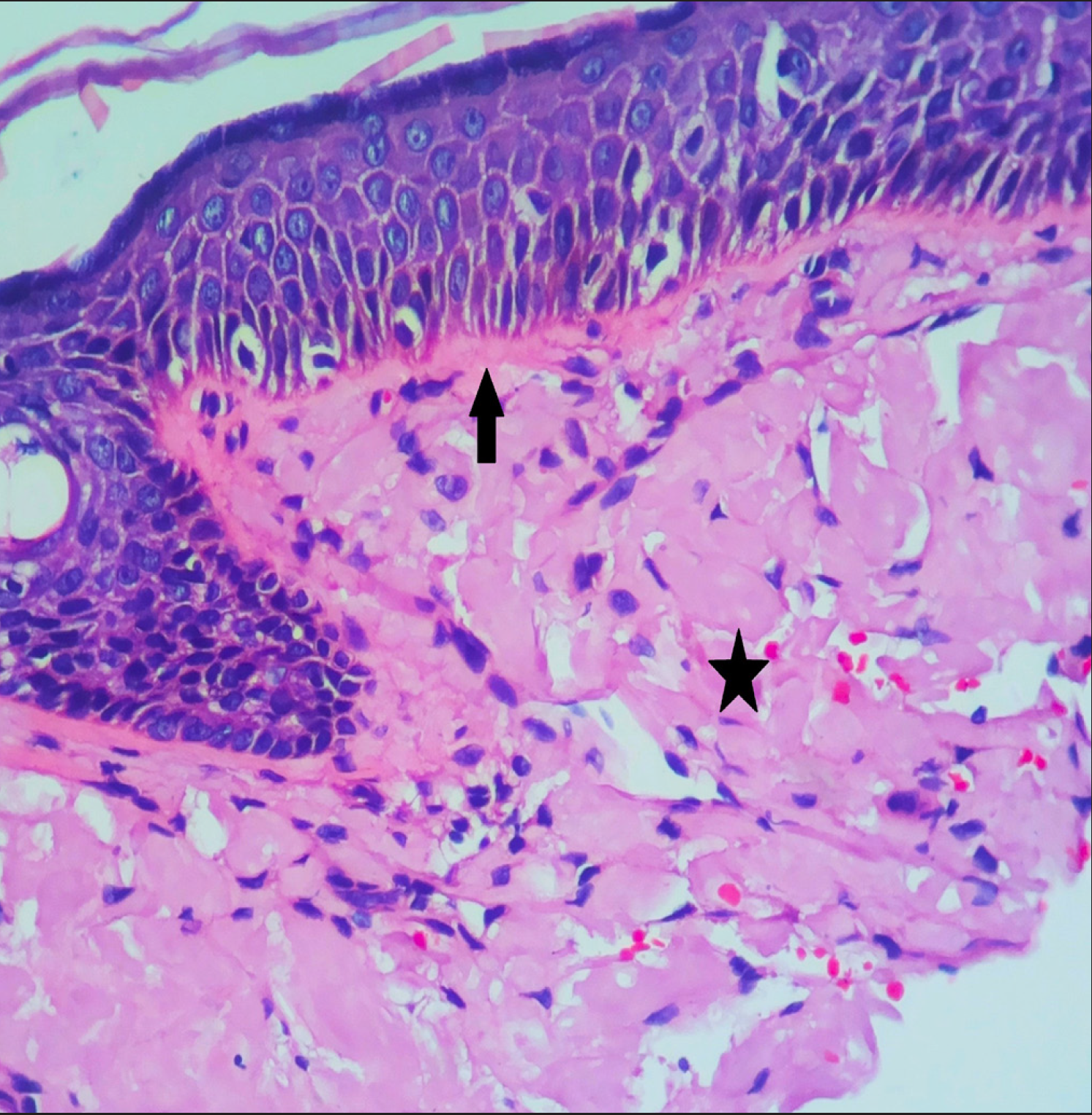 Figure 7
Figure 7- Colloid degeneration in colloid milium showing deposition of amorphous eosinophilic material in upper dermis (asterisk) separated from epidermis by normal connective tissue (arrow) (H and E, 400x)
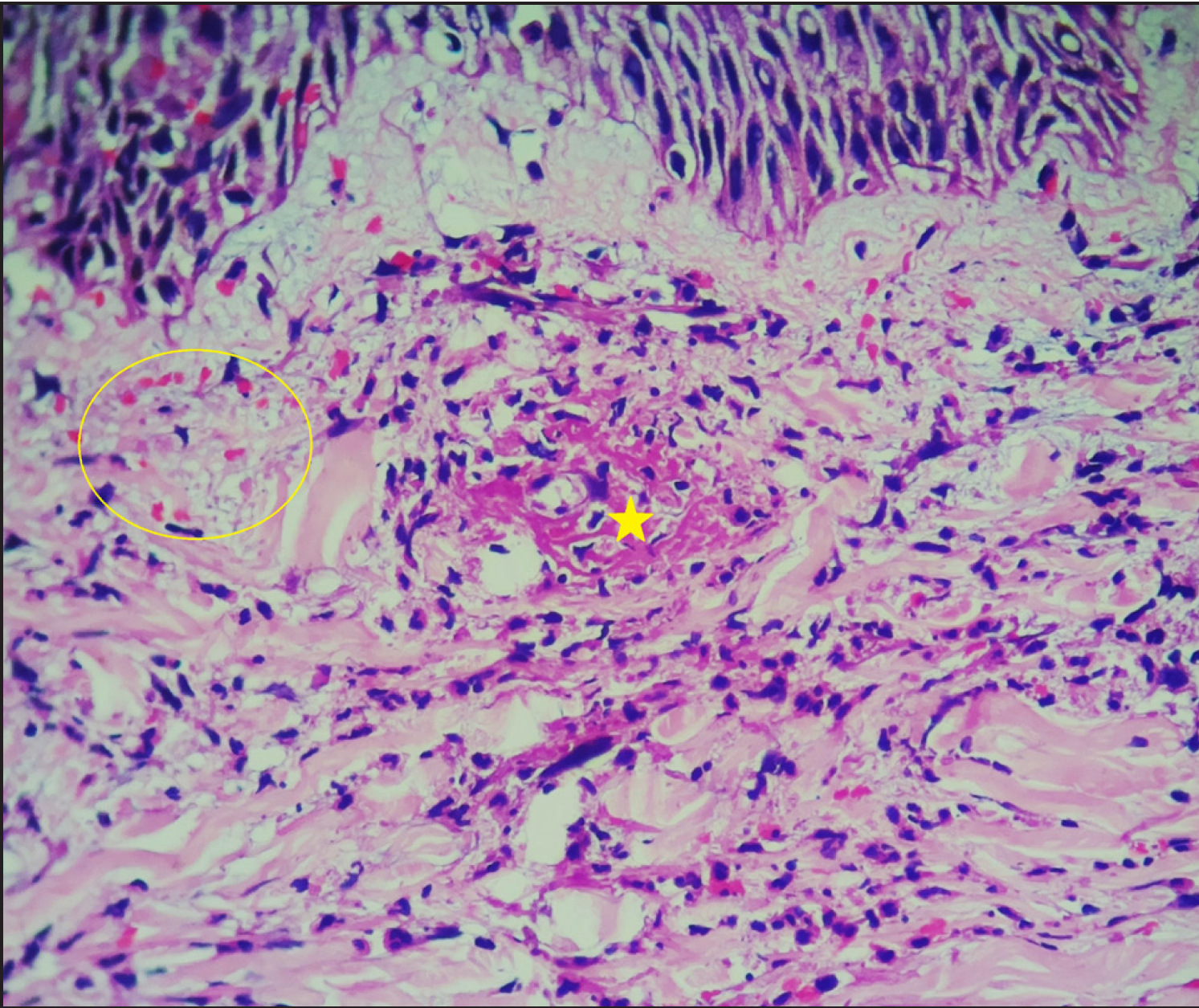 Figure 8
Figure 8- Fibrinoid degeneration in leukocytoclastic vasculitis showing deposition of amorphous, eosinophilic material in vessel walls and collagen fibers in upper dermis (yellow asterisk) and extravasation of erythrocytes (yellow circle) (H and E, 400x)
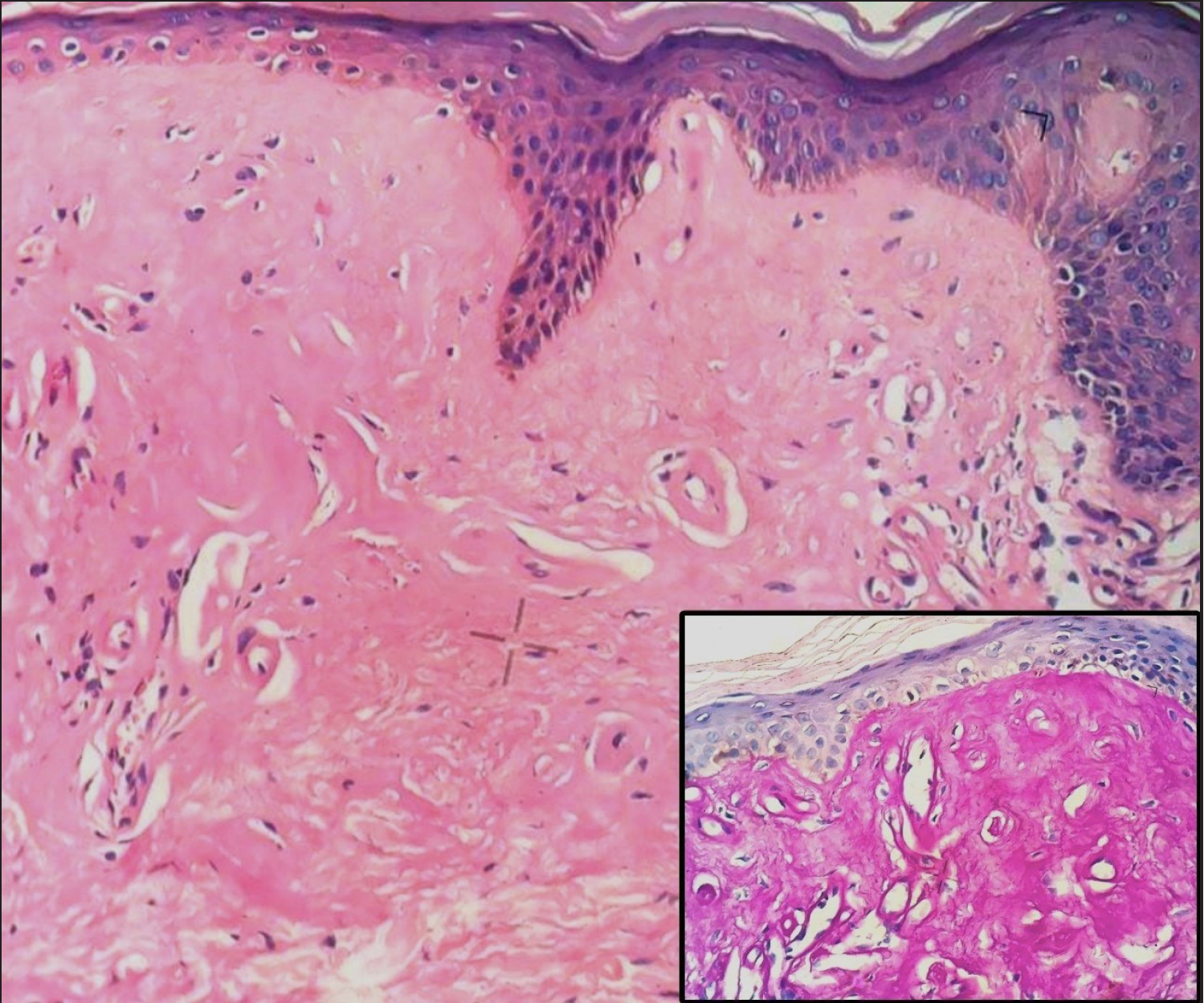 Figure 9
Figure 9- Hyaline degeneration in lipoid proteinosis (H and E, 400x), which is PAS +ve (Inset image, PAS stain, 400x)
-
-
1b)
Basophilic material
-
Mucoid degeneration:
It refers to the deposition of epithelial mucin, which is hardly detectable in normal skin.9 However, in pathological states such as follicular mucinosis, mucin deposition is evident in the infundibulum of the hair follicles, as well as in sebaceous glands [Figure 10].9 Mucin is thought to be produced as a result of cellular changes in the affected structures.10
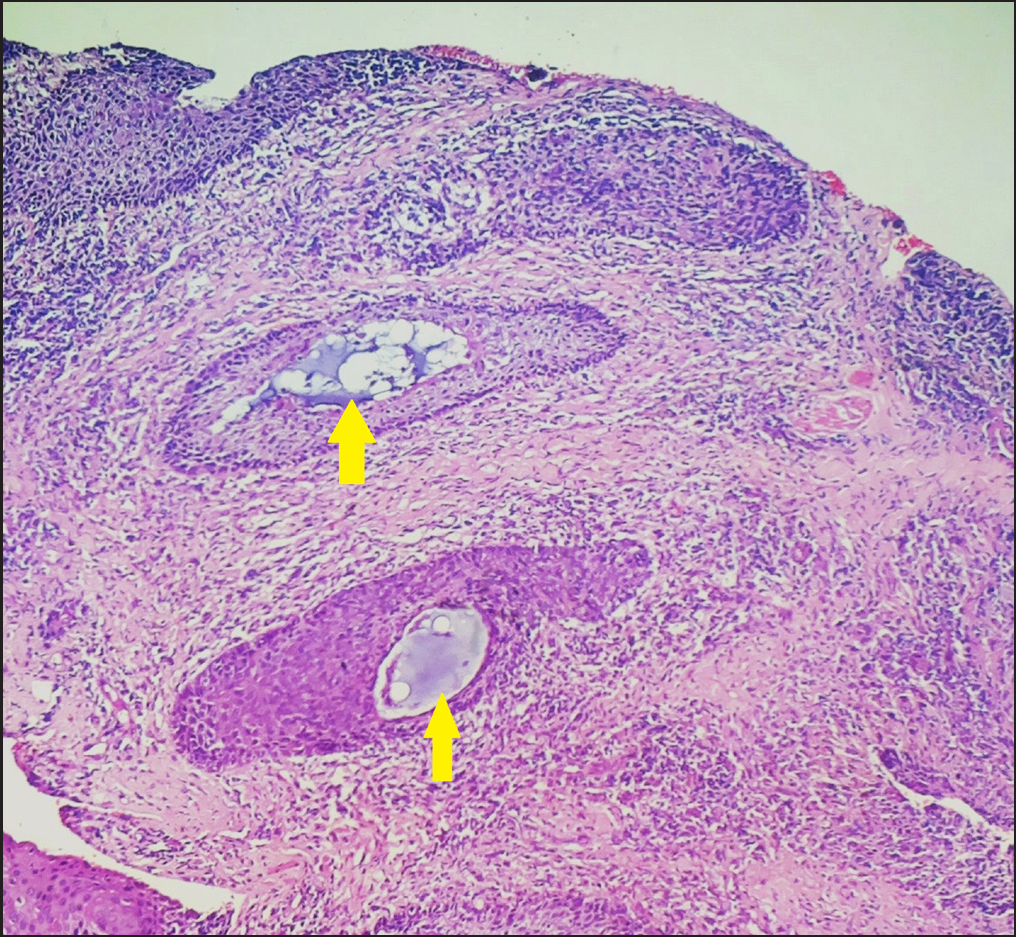 Figure 10
Figure 10- Mucoid degeneration in follicular mucinosis showing deposition of basophilic material in follicular infundibulum (yellow arrows) (H and E, 100x)
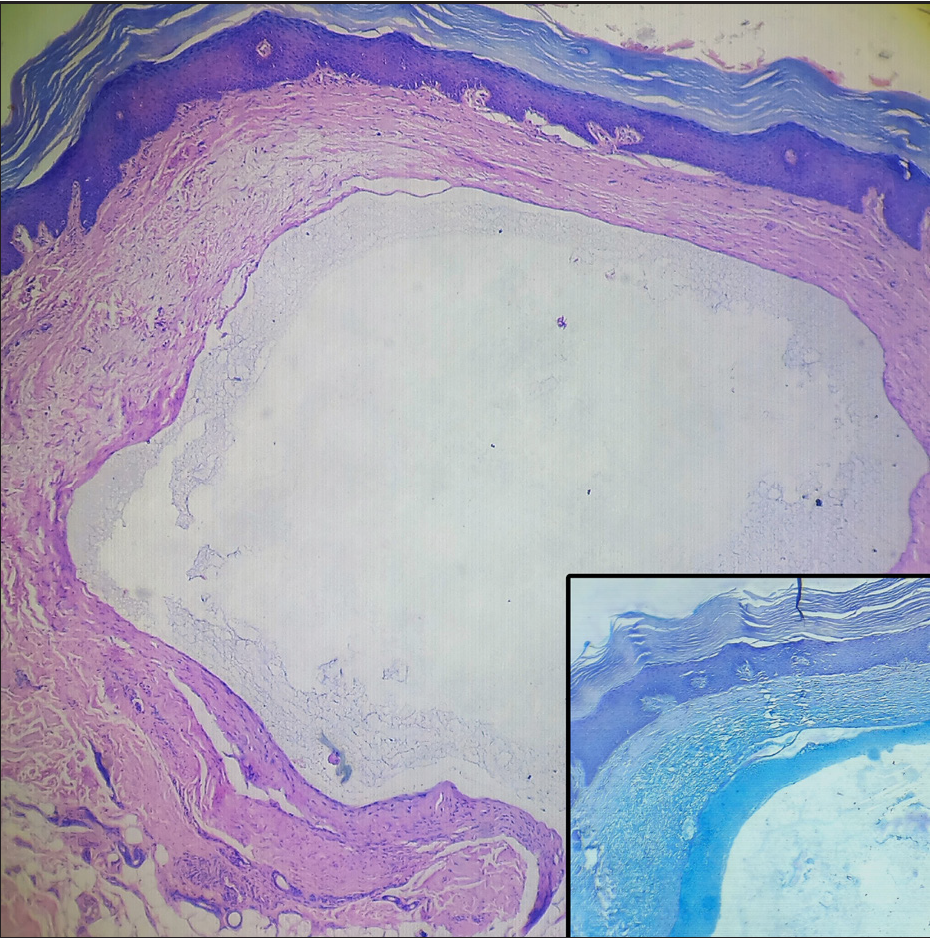 Figure 11
Figure 11- Myxoid degeneration in digital myxoid pseudocyst (H and E, 40x). Bluish, stringy material attached to cyst wall (Inset image, Alcian blue, 100x)
-
Myxoid degeneration:
It refers to the deposition of basophilic granular, stringy and feathery material in dermal connective tissue.9 It stains with Alcian blue at pH 2.5, but not at pH 1.0.1 It is seen in localized myxoedema, papular mucinosis, focal mucinosis, digital myxoid pseudocyst [Figure 11], scleredema, dermatomyositis, lupus erythematosus and various neoplasms such as fibroma, leiomyoma, schwannoma and basal cell carcinoma.2,9
-
-
-
Degeneration of dermal fibers
-
Elastotic degeneration:
It refers to the deposition of elastotic material (abnormal or disorganized elastic fibres) in the upper dermis replacing normal collagen fibres due to actinic damage.11 In sections stained with H & E, the elastotic material is basophilic and separated from the epidermis by a narrow band of normal‐staining connective tissue.2 It is seen in ageing skin, solar elastosis [Figure 12], actinic lichen planus, actinic cheilitis and elastotic nodules of the ears.11 Elastorrhexis (fragmented elastic fibres) is seen in acrokeratoelastoidosis of Costa and keratoelastoidosis marginalis.11,12
-
Collagen degeneration:
Degeneration of collagen is seen in various necrobiotic disorders such as granuloma annulare [Figure 13], necrobiotic lipoidica and necrobiotic xanthogranuloma.12 Necrobiosis is also known as collagenolysis as the normal wavy pattern of collagen bundles is replaced by disorganised, broken, smudgy collagen fibres having altered staining pattern.12 The term degeneration, rather than necrosis is preferred for such changes as necrosis is possible only for cells that are viable.1 It is also seen in chronic radiation dermatitis, ageing skin and tissue sent for histological examination after electrofulguration.
-
-
Miscellaneous degeneration:
-
Cystic degeneration:
It is also known as “encystification.” It is seen in cellular blue nevus and is characterised by edema, myxoid stromal alteration, diminished cellularity and scattered macrophages in the centre of the lesion.6
-
Fatty degeneration:
It refers to the formation of microscopically visible droplets of fat in the cytoplasm of cells (also known as foamy cells) as seen in verruciform xanthoma [Figure 14] or the development of metaplastic adipose cells as seen in long-standing dermal nevi.6
-
Clear cell degeneration:
The term “clear cell” has been used to describe a variety of cell types such as epithelial cells of apocrine, eccrine or trichilemmal differentiation, epithelial cells of spinous differentiation and malignant mesenchymal cells of unknown differentiation.13 These cells are loaded with mucin, glycogen or lipids that totally dissolve during processing, which accounts for their clear cytoplasm.13 It is seen in acrospiroma, clear cell hidradenoma, clear cell syringoma [Figure 15], clear cell acanthoma and clear cell trichoblastoma.13
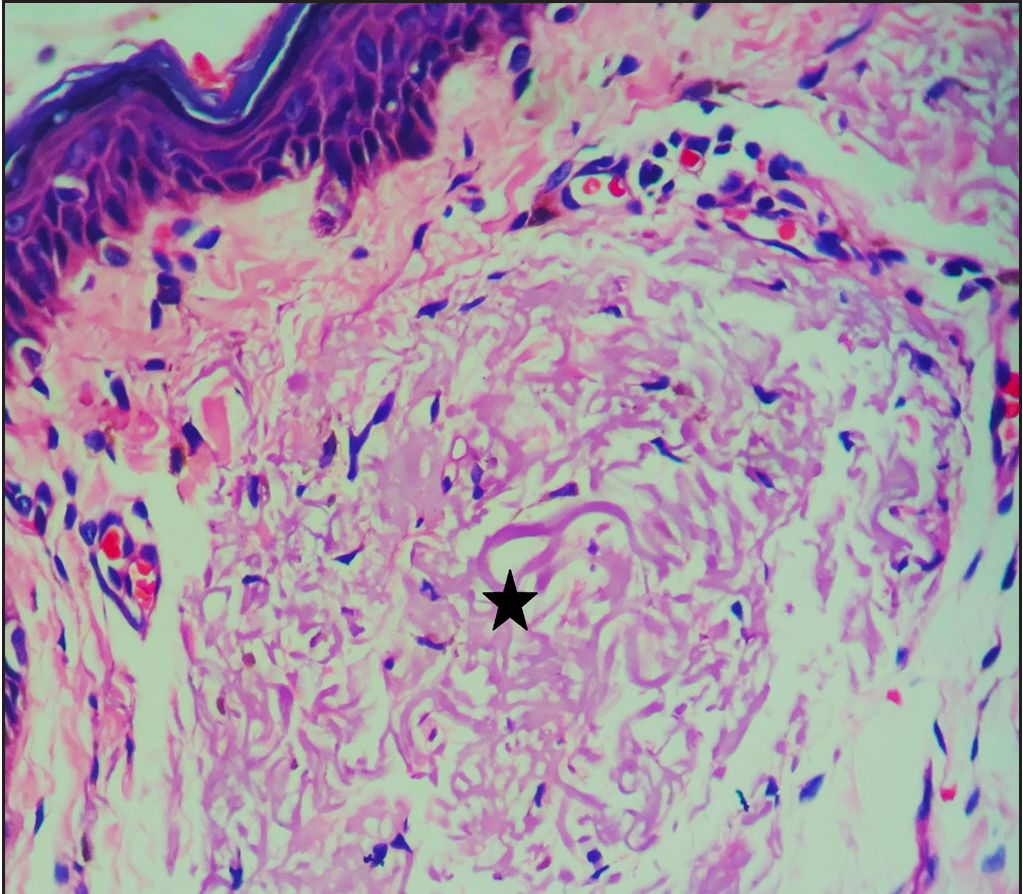 Figure 12
Figure 12- Basophilic elastotic degeneration in solar elastosis (asterisk) (H and E, 400x)
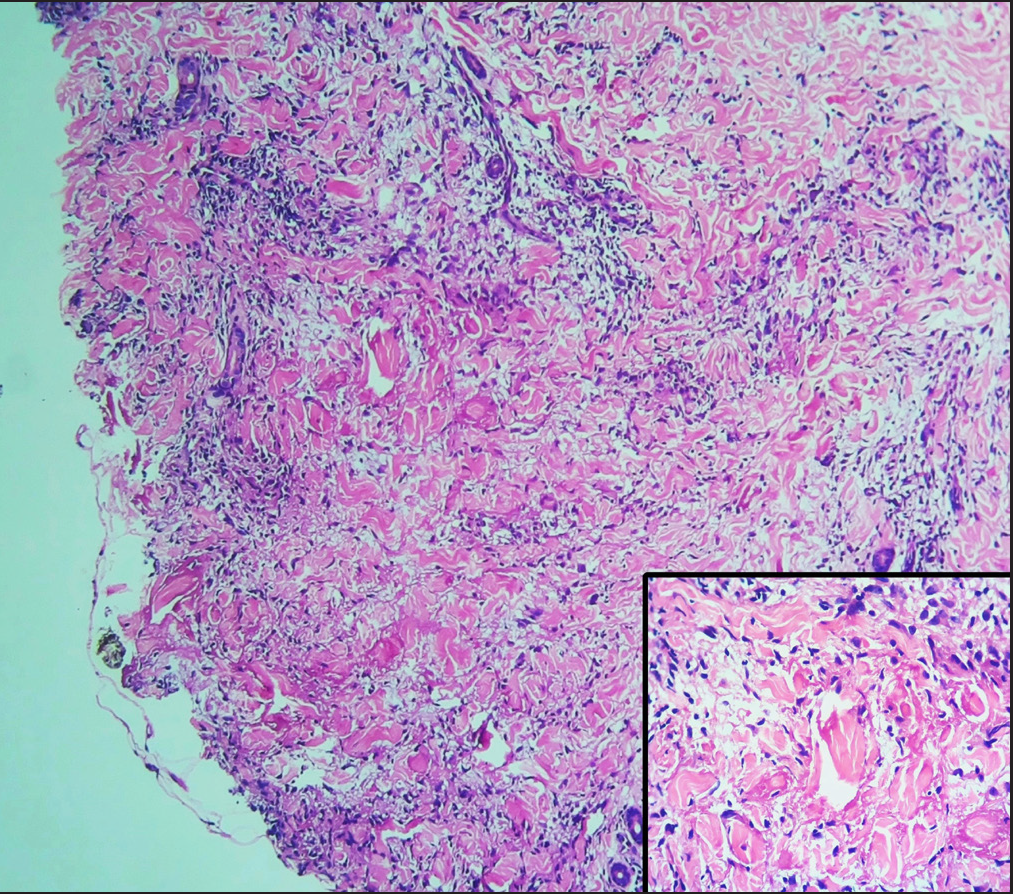 Figure 13
Figure 13- Collagen degeneration of granuloma annulare in lower dermis (H and E, 100x) Better visualised in inset image (H and E, 400x)
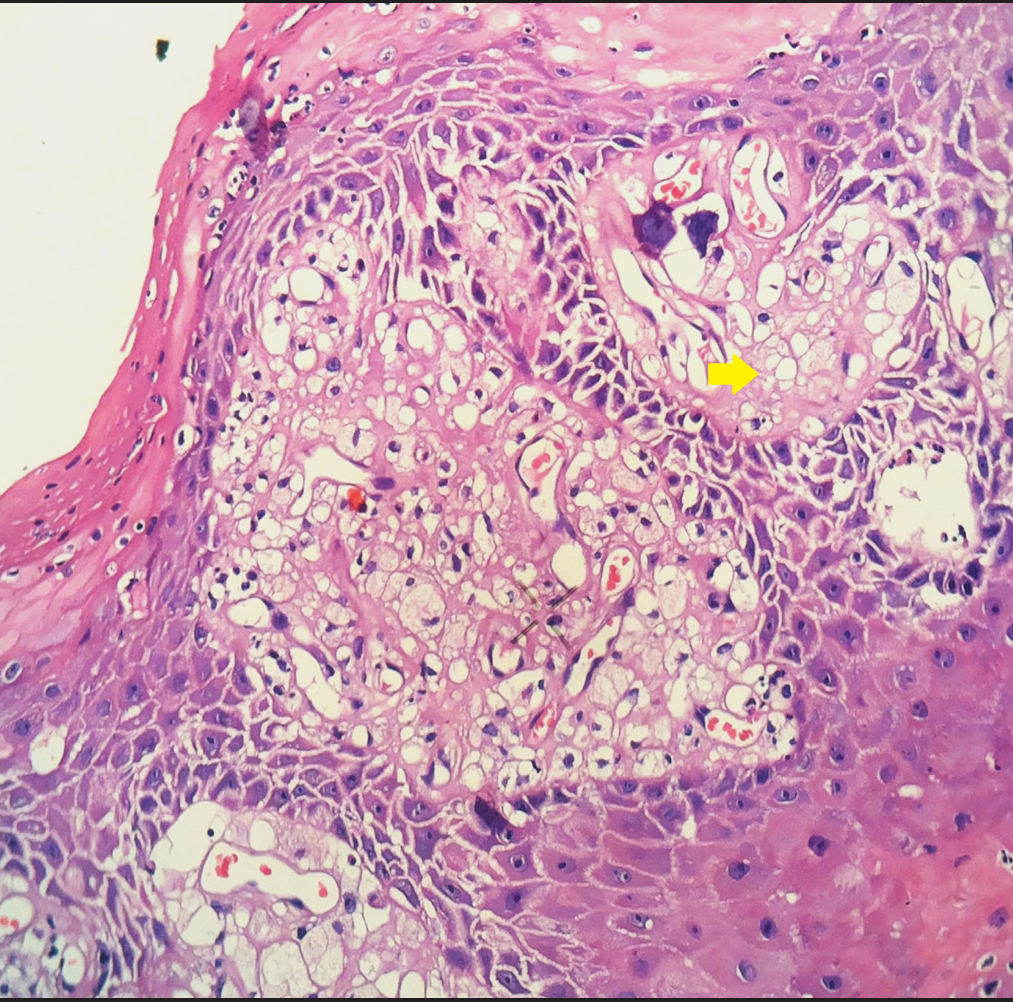 Figure 14
Figure 14- Fatty degeneration in verruciform xanthoma showing foamy cells in dermal papillae (yellow arrow) (H and E, 400x)
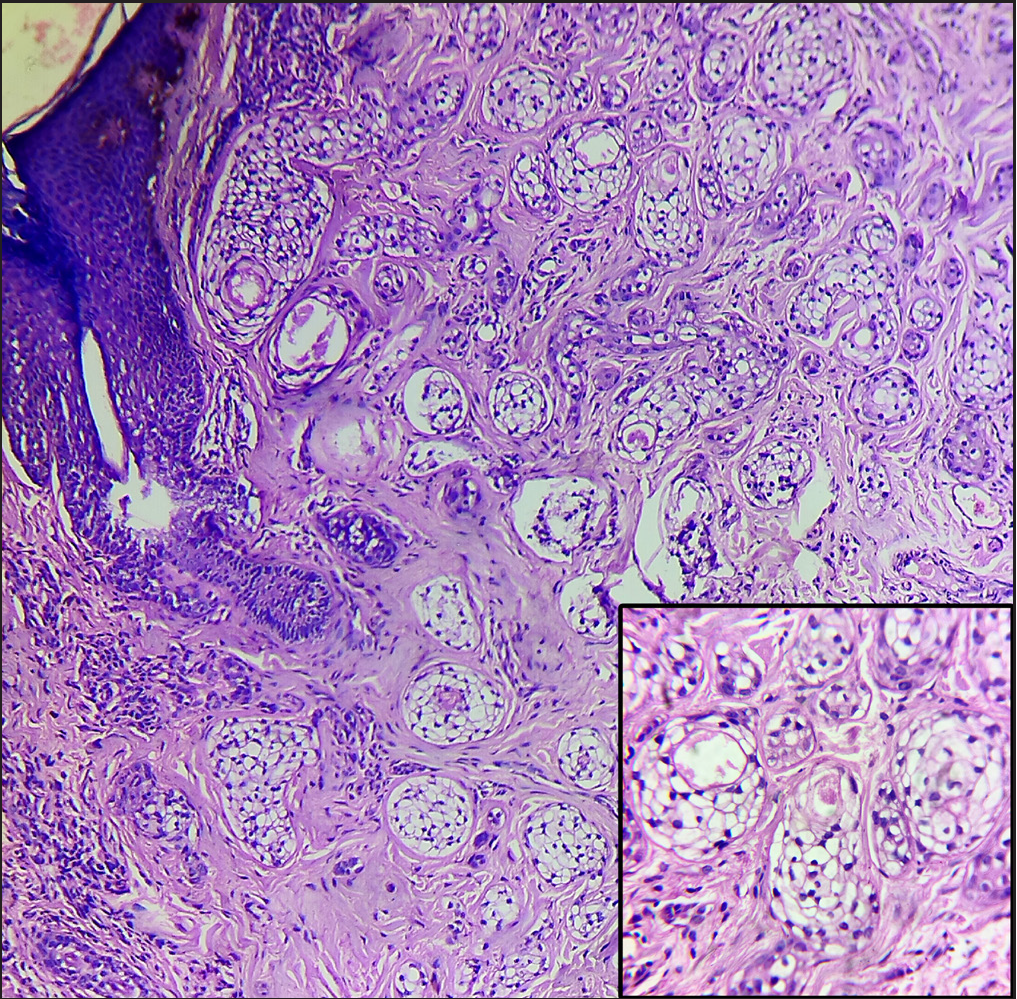 Figure 15
Figure 15- Clear cell degeneration in clear cell syringoma showing nests and cords of ductal epithelial cells with clear cell cytoplasm (H and E, 100x). Better appreciated in inset image (H and E, 400x)
-
Pseudoangiomatous degeneration:
It is seen in a variant of spindle cell lipoma. Numerous irregularly branched sinusoidal channels lined by flattened endothelial cells with villiform connective tissue projections divide tumour into lobules giving a striking angiomatoid appearance.6,14
-
Malignant degeneration:
Here, cells undergo malignant changes such as cellular pleomorphism, increased nuclear-to-cytoplasmic ratio, atypical mitotic figures and prominent nucleoli.15 Development of squamous cell carcinoma in porokeratosis, basal cell carcinoma in nevus sebaceous and malignant cylindromas are examples of malignant degeneration.6,15–17
-
Degeneration of cartilage:
In relapsing polychondritis and chondrodermatitis nodularis chronica helicis, chondrocytes undergo pyknosis, vacuolar changes and are eventually replaced by fibrous tissue.6 As per perichondrial vasculitis theory18, degeneration of cartilage starts with pressure on the auricle and further aggravated by same-side sleeping and prominauris. It leads to arteriolar narrowing in the perichondrium of helix causing ischemia, necrosis and protrusion of the underlying cartilage.
-
-
Conclusion
Dermatopathology is an integral part of the diagnostic workup of skin lesions. We have compiled important conditions showing degeneration in dermatopathology. This article describes the approach to degeneration in histopathological sections.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflict of interest.
References
- Definition of terms. In: Ackerman B, Boer A, Bennin B, Gottlieb G, eds. Histologic diagnosis of inflammatory skin diseases (3rd ed). New York (NY): Lippincott Williams and Wilkins; 2005. p. :129-70.
- [Google Scholar]
- Histopathology of the Skin: General Principles. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook’s textbook of dermatology (9th ed). Oxford: John Wiley & Sons; 2016. p. :3.1-3.41.
- [Google Scholar]
- Dermatopathology: An abridged compendium of words. A discussion of them and opinions about them. Part 2. Dermatol Pract Conc. 2013;3:3-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermatopathology: An abridged compendium of words. A discussion of them and opinions about them. Part 9 (T-Z) Dermatol Pract Conc. 2015;5:1-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Barnhill RL, Crowson AN, Magro CM, Piepkorn MW, eds. Dermatopathology (3rd ed). New York (NY): McGraw-Hill Medical; 2010.
- Nodular colloid degeneration of the skin: Report of three cases with review and update. Indian Dermatol Online J. 2014;5:36-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermatopathology: An abridged compendium of words. A discussion of them and opinions about them. Part 5. Dermatol Pract Conc. 2014;4:1-9.
- [Google Scholar]
- Dermatopathology: An abridged compendium of words. A discussion of them and opinions about them. Part 7 (M-O) Dermatol Pract Conc. 2015;5:1-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermatopathology: An abridged compendium of words. A discussion of them and opinions about them. Part 4. Dermatol Pract Conc. 2014;4:1-7.
- [Google Scholar]
- Calonje E, Brenn T, Lazar A, McKee PH, eds. McKee’s pathology of the skin (4th ed). Edinburgh: Elsevier/Saunders; 2012.
- Dermatopathology: An abridged compendium of words. A discussion of them and opinions about them. Part 3. Dermatol Pract Conc. 2014;4:3-9.
- [Google Scholar]
- Pseudoangiomatous variant of spindle cell lipoma: Report of a rare case. Indian J Pathol Microbiol. 2016;59:376-8.
- [CrossRef] [PubMed] [Google Scholar]
- Porokeratosis and malignant skin tumors. J Cancer Res Clin Oncol. 1991;117:55-60.
- [CrossRef] [PubMed] [Google Scholar]
- Tumors arising in nevus sebaceous: A study of 596 cases. J Am Acad Dermatol. 2000;42:263-8.
- [CrossRef] [PubMed] [Google Scholar]
- Benign vs. malignant skin adnexal neoplasms: How useful are silhouettes? Indian J Dermatol. 2013;58:30-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Advances in the understanding of chondrodermatitis nodularis chronica helices: The perichondrial vasculitis theory. Clin Otolaryngol. 2009;34:147-50.
- [CrossRef] [PubMed] [Google Scholar]





