Translate this page into:
Dermatoses due to Arabic cultural and traditional practices
Correspondence Address:
Fatimah Mohammad Budair
Department of Dermatology, King Fahd Teaching Hospital of the University, Imam Abdulrahman Bin Faisal University, Alkhobar
Kingdom of Saudi Arabia
| How to cite this article: Budair FM. Dermatoses due to Arabic cultural and traditional practices. Indian J Dermatol Venereol Leprol 2019;85:448-454 |
Abstract
A number of social and cultural practices are prevalent in the Middle-East celebrating various occasions or to treat health conditions. These often result in dermatoses that are unfamiliar and confusing to dermatologists outside this region. This paper reviews skin manifestations emanating from traditional and ritual practices in Arab countries, particularly those from Saudi Arabia.
Introduction
Arab countries are defined by their Islamic heritage and Bedouin traditions that have been handed down through generations. The application of various herbal preparations, cautery and cupping to treat medical issues, the use of traditional cosmetics such as henna and kohl as well as threading to celebrate religious and other occasions, and male circumcision, are some of the traditional customs prevalent in this region. The resulting adverse effects on the skin may lead to confusion among physicians unfamiliar with these practices. This review focuses on how Arabic cultural and traditional practices and remedies can result in various skin diseases.
Materials and Methods
A search for relevant literature was conducted using Scopus, PubMed, Web of Science and Google Scholar. Publications dating from the inception of these search engines up to 2014 were identified using the following key words: alternative medicine, dermatosis, cultural practices, adverse effects, traditional practices Saudi Arabia, henna allergy and traditional practice. All articles, including case reports, review articles, case series, observational studies and surveys on the use of complementary and alternative medicine in Saudi Arabia, as well as on the traditional practices were considered and were read in full. Adverse dermatologic effects were noted, and the history of origin, type of practices and their usage were recorded.
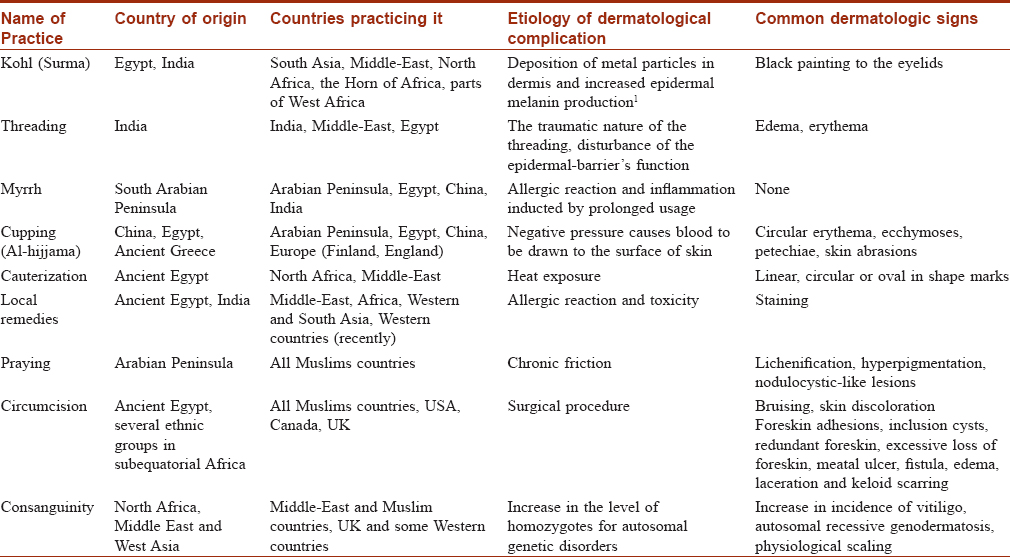
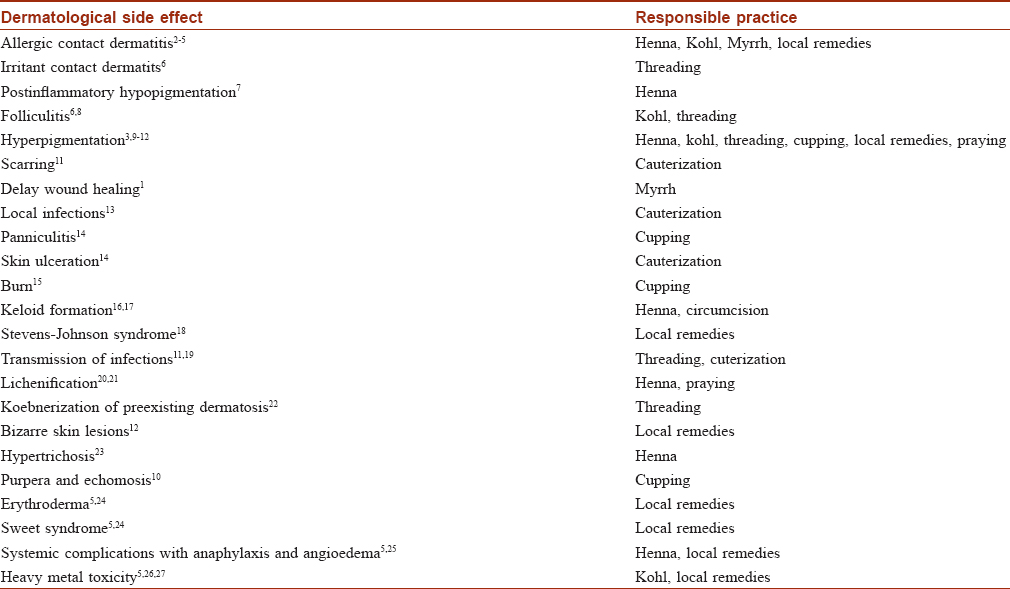
Results
A number of traditional cultural practices in Saudi Arabia were found to cause dermatological effects. These customs included the cosmetic use of henna, kohl and threading, as well as the use of myrrh, cupping therapy (Al-hijama), cauterization and the application of topical remedies for medical conditions. Circumcision and consanguinity are prevalent in the Arab world and were also responsible for a number of dermatologic conditions. [Table - 1]. Skin manifestations associated with these practices ranged from simple pigmentation to life-threatening erythroderma and Stevens–Johnson syndrome [Table - 2].
Traditional practices for cosmetic purposes
Henna
Henna is commonly used by both sexes in Arabic countries. Women use henna to design exquisite temporary tattoos on their hands, arms and feet, whereas men commonly use it to colour their beards. The use of henna dates back to ancient Egypt, between 3000 and 1400 BCE, where it was used for medicinal purposes (Bryan, 1974, Ebers Papyrus, artifacts). In Syria and on the Arabian Peninsula it was used for its medicinal properties as well as for dyeing fingernails and hair, and for body art during bridal celebrations between 500 BCE and 700 CE (Josephus and the Jewish Encyclopedia). Henna is derived from a flowering plant (Lawsonia inermis) belonging to the lythraceae family. The leaves containing 2-hydroxy-1,4-naphthoquinone (Lawson molecules) are dried, ground into a powder and mixed with oil or water to form a paste for use as a dye. Although rare, pure henna has on occasion been recorded to cause allergic contact dermatitis.[1]
The addition of other substances such as p-phenylenediamine and indigo blue to deepen the colour of henna from red-orange to dark brown or black are more commonly responsible for skin lesions. p-Phenylenediamine was present in all black henna samples randomly collected from 15 henna salons in the United Arab Emirates in concentrations ranging from 0.4 and 29.5%, and in six of these samples the concentration exceeded that permitted by European Union directives i.e. 6.0%.[2] Allergic contact dermatitis caused by p-phenylenediamine at the application sites of black henna and hair dyes (eyebrows and hands of women and beards areas of men) is not uncommon[3] and may manifest as eczematous lesions, severe vesiculobullous or [Figure - 1], lichenoid reactions [4] and rarely, as a generalized eruption that may require treatment with oral corticosteroids.[5] Sequelae include hyperpigmentation [6], temporary hypertrichosis,[7] keloids [8], permanent post-inflammatory hypopigmentation [9], and sensitization to p-phenylenediamine with cross-reactions with other chemicals of the para group of sulfonamides and azoic and aniline-dyes,[10]
 |
| Figure 1: Allergic contact dermatitis at the site of applying henna |
Kohl (surma)
The use of kohl, or surma (derived from the word for antimony) has been popular in the Middle-East since ancient times. It is traditionally applied to the conjunctival surface of the eyelids. Kohl is applied on the eyelids of new-born babies to protect their eyes from infections. The content of kohl and methods used to prepare it vary greatly. In Arabic countries, kohl is usually prepared at home by grinding galena (lead sulfide), but amorphous carbon or organic charcoal is often used elsewhere.[11] The use of kohl is encouraged in Saudi Arabia owing to the general perception that is safe and healthy for the eyes. However, kohl may have serious adverse effects including lead poisoning and encephalopathy.[12],[13]
Pigmentation of the conjunctiva and the lacrimal sac, extending to the adjacent skin of the eyelids has been positively correlated with the duration of kohl application.[14] Watery, itchy eyes and allergies are also possible side effects of applying kohl to the eyelids of infants.[15] Because kohl is popular among immigrants in developed countries, it is important for dermatologists in developed nations to be aware of this practice and its implications.
Threading
Threading is commonly practiced in the Arab world as a fast, effective and inexpensive way of removing unwanted facial hair and is performed by hairdressers or beauticians. In Saudi Arabia both men and women use threading to remove unwanted vellus hairs from their cheeks, ears, beard, upper lips, eyebrows and forehead.
Following threading an immediate mild erythema and edema may develop sometimes followed by an irritant dermatitis or hyperpigmentation.[16] Infections such as molluscum contagiosum, plane warts [Figure - 2] and bullous impetigo may be transmitted by threading [17],[18] either by the thread used, the powder applied before the procedure, or through the beautician's hands, and may be facilitated by the traumatic nature of the procedure that breaches the epidermal barrier. Beauticians performing threading should be trained in aseptic techniques to minimize the risk of side effects. Koebnerization of preexisting conditions owing to trauma caused by threading may occur and there is a report of vitiligo affecting the eyebrow area after threading.[19]
 |
| Figure 2: Flat warts at the site of eyebrows threading |
Traditional practices for treating health conditions
Myrrh
Myrrh, is the dried oleo-gum-resin of the Commiphora spp of the burseraceae family that grows in the Arabian Peninsula. Myrrh or mur was a common treatment for wounds and sepsis through the 4th century BC. It is still used in China it to treat mouth and skin infections, and in Arab countries for its antiparasitic and antimicrobial effects.[20] The effects of myrrh have been more recently studied in fascioliasis, schistosomiasis, Pseudomonas, Staphylococcus aureus and Escherichia coli infections.[21] Some recent studies in animals have suggested that myrrh may possess wound healing activity by downregulating the expression of proinflammatory mediators.[22] Dermatologists have used myrrh to treat aphthous ulcers and atopic eczema.[23],[24] Although myrrh is generally nonirritating, there are several reports of allergic contact dermatitis after frequent exposures.[25]
Cupping therapy (Al-hijama)
Cupping is a common traditional practice in East Asian and Arab countries that has been performed for thousands of years. It involves using a flame to achieve negative pressure inside the cups (dry cupping) applied on the skin of the back and neck. In wet cupping or Al-hijama, skin incisions are made such that the suction draws out a small quantity of blood. Al-hijama is a common Saudi practice with the cup and vacuum in a place for 10–15 min. Modern cupping may use suction devices to create negative pressure. It is thought that the negative pressure induces therapeutic effects by dilating local blood vessels to improve microcirculation, promotes capillary endothelial cell repair, accelerates granulation and angiogenesis and shortens healing times by reducing bacterial burden and septic complications. It has been suggested that cup placement over selected acupoints on the skin produces hyperemia or hemostasis with therapeutic results.[26]
Cupping has been used for painful conditions, respiratory symptoms, hypertension and herpes zoster.[27] In Saudi Arabia cupping is often used to treat various chronic illnesses including cancer and diabetes.[28] It has been suggested to be effective in acne vulgaris, atopic dermatitis, chronic idiopathic urticaria and eczema.[29],[30]
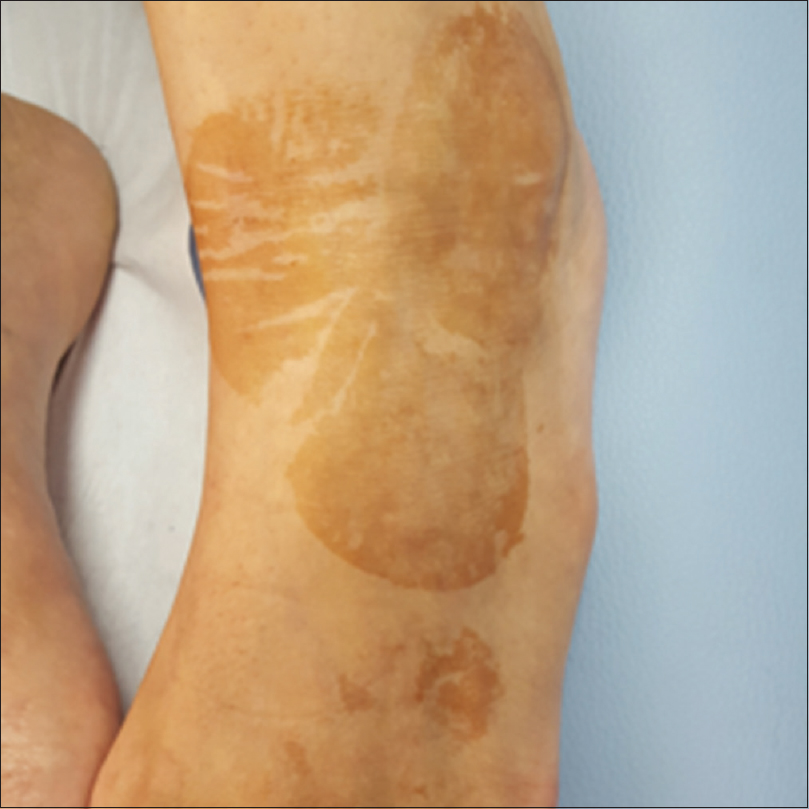
Cupping may lead to a variety of cutaneous artefacts including erythema, edema, purpura and ecchymosis in a characteristic circular arrangement. Pigmentation, bullae and burns are not uncommon, and factitial panniculitis has been reported.[31],[32],[33] It has occasionally been mistaken for child abuse.[34]
Cauterization (Kaiy)
Cauterization or kaiy is a custom in which a red-hot iron, a pinch of hot cinders or a burning coal is applied to the skin to cause burns for treating a variety of different health conditions, including abdominal pain, lower back pain, sadness, depression, headache, and for exorcism. Kaiy is the most commonly used alternative medicine practiced in Saudi Arabia.[35]
Cauterization causes sharply demarcated circular or oval (sometimes linear) burns arranged in symmetrical patterns [Figure - 3], often leading to permanent scarring. Other complications such as edema, infection, nonhealing ulcers are frequent and sometimes transmission of viruses such as hepatitis B virus may occur.[36] It is not unusual to note old healed cautery scars on immigrants from Saudi Arabia.
 |
| Figure 3: Circular and sharply demarcated lesion in the abdomen of a man who have been doing cauterization to treat hepatitis C infection |
Local remedies
Topical application of herbal and other preparations for treating skin conditions is a common practice in the Middle East and is generally perceived to be safe as they are considered “natural”. Although some treatments may have antiinflammatory and antibacterial effects [37] a “natural”status does not necessarily indicate safety, and it is essential for doctors and patients to understand the risk of complications. Such applications may cause discoloration [Figure - 4], allergic contact dermatitis, erythroderma, Stevens–Johnson syndrome, Sweet's syndrome, pellagra, arsenic dermatosis and exogenous ochronosis (due to skin whitening creams with a high concentration of hydroquinone). Systemic reactions can also occur, including respiratory, cardiovascular, gastrointestinal, hepatic, renal impairment and reproductive effects.[38],[39],[40],[41]
 |
| Figure 4: Hyperpigmentation occurring at the site of applying local remedies to treat itching |
Ritual practices
Prayer
In the Arab world, the majority of the population is Muslim, and Islam is the state religion. Prayer is mandatory five different times every day during which different postures are adopted, namely, standing, bowing, prostration and sitting and thickening, lichenification, hyperpigmentation and nodulocystic-like lesions or “prayer marks” develop owing to friction [Figure - 5]. These callosities are commonly seen in approximately 75% of men and 25% of women especially in those older than [42] The lower frequency of prayer nodules in women is partly due to their spending less time in prayer as well as the greater amount of subcutaneous fat over the bony prominences.
 |
| Figure 5: Well-circumscribed hyperkeratotic and hyperpigmented lesion in the forehead of a man with history of frequent friction during prayer |
Prayer marks usually develop on the forehead, knees, ankles and dorsa of the feet, especially the dorsum of left foot due to the characteristic posture adopted when sitting in prayer. Histologic findings include hyperkeratosis, hypergranulosis, acanthosis and mild inflammatory infiltration in the upper dermis with no collagen bundles perpendicular to the epidermis (unlike lichen simplex chronicus) and mucin deposition may be seen.[43] These marks may be treated with 40% urea cream, using protective clothing (e.g. caps, socks) or using soft prayer mats. Such skin changes are mostly benign, as there is no risk of ulceration, bleeding, bullous formation or infections.
Circumcision
Circumcision is one of the most common of medical procedures performed in the world. It is estimated that about one-third of the world's male population is circumcised.[44] Male circumcision is nearly universal in the Arab world, and is usually performed during neonatal period for religious or tribal reasons.[45]
The incidence of complications associated with circumcision ranges from 0.1 to 16%, and is more likely to occur if circumcision is performed at an older age, under nonsterile conditions or without expert supervision.[46],[47]
Hematomas often occur within 48h of surgery associated with considerable bruising and skin discoloration. Wound infection with visible signs such as redness or purulent discharge, foreskin adhesions, inclusion cysts, redundant foreskin, excessive loss of foreskin, meatal ulcers, fistulas, edema of the glans penis, lacerations, keloid scarring, and, rarely, Fournier's gangrene are all possible dermatological complications that have been reported.[48]
Although it has been suggested that circumcision prevents or protects against penile cancer and inflammatory dermatoses such as lichen planus, psoriasis, seborrheic dermatitis, lichen sclerosus and sexually acquired infections,[49],[50] and genital warts were found to be more likely to occur in circumcised men.[51]
Other traditional practices
Consanguinity
Consanguineous marriage i.e. marriage between blood relatives is common among Arabs and is especially popular and widespread in Saudi Arabia owing to the tribal organization based on common ancestry. It is defined as marriage between people who are second cousins or closer.[52]
Consanguinity increases the incidence of diseases associated with genetic factors. In a study conducted by Alenizi in northern part of Saudi Arabia, vitiligo incidence was shown to be increased by consanguinity and genetic counseling was recommended by these workers as a means of lowering the prevalence of vitiligo.[53] Other skin conditions with an increased prevalence attributable to consanguinity include physiological scaling (benign superficial skin desquamation that commonly occur in neonates),[54] xeroderma pigmentosum, epidermolysis bullosa and lamellar ichthyosis.[55],[56] The risk for developing recessive conditions related to inbreeding was proportional to the degree of consanguinity.[57]
A detailed family history should be obtained when examining patients originating from areas with a high rate of consanguinity and family counseling may be attempted to discourage this practice.
Discussion
This review highlights various religious and traditional practices in Saudi Arabia and adjacent regions that are often regarded as harmless. Despite the rapid development of medical services in Arab countries, traditional healing practices are still commonly used, particularly in suburban areas. Patients frequently prefer to use traditional treatments first before turning to Western medicine. A lack of awareness of these practices among Western physicians may compromise the quality of care they can provide and may affect the accuracy of health histories and clinical diagnoses as exemplified by the case where skin lesions caused cupping were misinterpreted by conscientious healthcare workers as child abuse. Also, the use of these traditional practices and customs to treat heath conditions may delay effective therapy with disastrous consequences.
Limitation of the study
Although the article clearly reviews the dermatosis that result from the cultural and traditional practices in Arab countries, it does not provide a full explanation for how some of these skin findings may occur.
Conclusion
Widespread migration of Arabs necessitates that dermatologists familiarize themselves with Arabic cultural practices, such as the use of henna, threading and cupping and the effects of these practices on the skin. Because Saudi Arabia has unique religious and cultural traditions that are not shared with other non-Arab ethnic groups, such as the use of myrrh, cauterization and Al-hijama, this review may be important for dermatologists in non-Arab countries encountering with cases resulting from these practices.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Belhadjali H, Akkari H, Youssef M, Mohamed M, Zili J. Bullous allergic contact dermatitis to pure henna in a 3-year-old girl. Pediatr Dermatol 2011;28:580-1.
[Google Scholar]
|
| 2. |
Al-Suwaidi A, Ahmed H. Determination of para-phenylenediamine (PPD) in henna in the United Arab Emirates. Int J Environ Res Public Health 2010;7:1681-93.
[Google Scholar]
|
| 3. |
Redlick F, Dekoven J. Allergic contact dermatitis to paraphenylendiamine in hair dye after sensitization from black henna tattoos: A report of 6 cases. CMAJ. 2007;176:445-6.
[Google Scholar]
|
| 4. |
Rubegni P, Fimiani M, de Aloe G, Andreassi L. Lichenoid reaction to temporary tattoo. Contact Dermatitis 2000;42:117-8.
[Google Scholar]
|
| 5. |
Evans CC, Fleming JD. Images in clinical medicine. Allergic contact dermatitis from a henna tattoo. N Engl J Med 2008;359:627.
[Google Scholar]
|
| 6. |
Bukhari IA. Cutaneous hyperpigmentation following nonpermanent henna tattoo. Saudi Med J 2005;26:142-4.
[Google Scholar]
|
| 7. |
del Boz J, Martín T, Samaniego E, Vera A, Morón D, Crespo V. Temporary localized hypertrichosis after henna pseudotattoo. Pediatr Dermatol 2008;25:274-5.
[Google Scholar]
|
| 8. |
Gunasti S, Aksungur VL. Severe inflammatory and keloidal, allergic reaction due to para-phenylenediamine in temporary tattoos. Indian J Dermatol Venereol Leprol 2010;76:165-7.
[Google Scholar]
|
| 9. |
Wöhrl S, Hemmer W, Focke M, Götz M, Jarisch R. Hypopigmentation after non-permanent henna tattoo. J Eur Acad Dermatol Venereol 2001;15:470-2.
[Google Scholar]
|
| 10. |
Marcoux D, Couture-Trudel PM, Riboulet-Delmas G, Sasseville D. Sensitization to para-phenylenediamine from a streetside temporary tattoo. Pediatr Dermatol 2002;19:498-502.
[Google Scholar]
|
| 11. |
Nouioui MA, Mahjoubi S, Ghorbel A, Ben Haj Yahia M, Amira D, Ghorbel H, et al. Health risk assessment of heavy metals in traditional cosmetics sold in Tunisian local markets. Int Sch Res Notices 2016;2016:6296458.
[Google Scholar]
|
| 12. |
Al-Ashban RM, Aslam M, Shah AH. Kohl (surma): A toxic traditional eye cosmetic study in Saudi Arabia. Public Health 2004;118:292-8.
[Google Scholar]
|
| 13. |
Shaltout A, Yaish SA, Fernando N. Lead encephalopathy in infants in Kuwait. A study of 20 infants with particular reference to clinical presentation and source of lead poisoning. Ann Trop Paediatr 1981;1:209-15.
[Google Scholar]
|
| 14. |
Omar SS, Inas FG, Laila R, Hany S. Periorbital pigmentation by lead in kohl. J Egypt Womens Dermatol Soc 2006;3:4-18.
[Google Scholar]
|
| 15. |
Goswami K. Eye cosmetic 'surma': Hidden threats of lead poisoning. Indian J Clin Biochem 2013;28:71-3.
[Google Scholar]
|
| 16. |
Abdel-Gawad MM, Abdel-Hamid IA, Wagner RF Jr. Khite: A non-western technique for temporary hair removal. Int J Dermatol 1997;36:217.
[Google Scholar]
|
| 17. |
Ghosh SK, Bandyopadhyay D. Molluscum contagiosum after eyebrow shaping: A beauty salon hazard. Clin Exp Dermatol 2009;34:e339-40.
[Google Scholar]
|
| 18. |
Bloom MW, Carter EL. Bullous impetigo of the face after epilation by threading. Arch Dermatol 2005;141:1174-5.
[Google Scholar]
|
| 19. |
Verma SB. Vitiligo koebnerized by eyebrow plucking by threading. J Cosmet Dermatol 2002;1:214-5.
[Google Scholar]
|
| 20. |
Massoud A, El Sisi S, Salama O, Massoud A. Preliminary study of therapeutic efficacy of a new fasciolicidal drug derived from Commiphora molmol (myrrh). Am J Trop Med Hyg 2001;65:96-9.
[Google Scholar]
|
| 21. |
Massoud AM, El Ebiary FH, Abd El Salam NF. Effect of myrrh extract on the liver of normal and bilharzially infected mice. An ultrastructural study. J Egypt Soc Parasitol 2004;34:1-21.
[Google Scholar]
|
| 22. |
Fatani AJ, Alrojayee FS, Parmar MY, Abuohashish HM, Ahmed MM, Al-Rejaie SS. Myrrh attenuates oxidative and inflammatory processes in acetic acid-induced ulcerative colitis. Exp Ther Med 2016;12:730-8.
[Google Scholar]
|
| 23. |
Albishri J. The efficacy of MYRRH in oral ulcer in patients with behcet's disease. American Journal of Research Communication. 2017;5:23-8.
[Google Scholar]
|
| 24. |
El Ashry ES, Rashed N, Salama OM, Saleh A. Components, therapeutic value and uses of myrrh. Pharmazie 2003;58:163-8.
[Google Scholar]
|
| 25. |
Al-Suwaidan SN, Gad el Rab MO, Al-Fakhiry S, Al Hoqail IA, Al-Maziad A, Sherif AB. Allergic contact dermatitis from myrrh, a topical herbal medicine used to promote healing. Contact Dermatitis 1998;39:137.
[Google Scholar]
|
| 26. |
Cui S, Cui J. Progress of researches on the mechanism of cupping therapy. Zhen Ci Yan Jiu 2012;37:506-10.
[Google Scholar]
|
| 27. |
Gao LW. Practical Cupping Therapy. Beijing: Academy Press; 2004.
[Google Scholar]
|
| 28. |
Jazieh AR, Al Sudairy R, Abulkhair O, Alaskar A, Al Safi F, Sheblaq N, et al. Use of complementary and alternative medicine by patients with cancer in Saudi Arabia. J Altern Complement Med 2012;18:1045-9.
[Google Scholar]
|
| 29. |
El-Domyati M, Saleh F, Barakat M, Mohamed N. Evaluation of cupping therapy in some dermatoses. Egypt Dermatol Online J 2003;9:2.
[Google Scholar]
|
| 30. |
Wang Q. 54 cases of eczema treated with acupuncture, bloodletting and cupping. Shang J Acupunct 2004;2:37-8.
[Google Scholar]
|
| 31. |
Tuncez F, Bagci Y, Kurtipek GS, Erkek E. Suction bullae as a complication of prolonged cupping. Clin Exp Dermatol 2006;31:300-1.
[Google Scholar]
|
| 32. |
Kose AA, Karabaǧli Y, Cetin C. An unusual cause of burns due to cupping: Complication of a folk medicine remedy. Burns 2006;32:126-7.
[Google Scholar]
|
| 33. |
Lee JS, Ahn SK, Lee SH. Factitial panniculitis induced by cupping and acupuncture. Cutis 1995;55:217-8.
[Google Scholar]
|
| 34. |
Asnes RS, Wisotsky DH. Cupping lesions simulating child abuse. J Pediatr 1981;99:267-8.
[Google Scholar]
|
| 35. |
Al-Awamy BH. Evaluation of commonly used tribal and traditional remedies in Saudi Arabia. Saudi Med J 2001;22:1065-8.
[Google Scholar]
|
| 36. |
Qureshi NA, Al-Amri AH, Abdelgadir MH, EL-Haraka E. Traditional cautery among psychiatric patients in Saudi Arabia. Transcult Psychiatry 1998;35:75-83.
[Google Scholar]
|
| 37. |
Bakhotmah BA, Alzahrani HA. Self-reported use of complementary and alternative medicine (CAM) products in topical treatment of diabetic foot disorders by diabetic patients in Jeddah, Western Saudi Arabia. BMC Res Notes 2010;3:254.
[Google Scholar]
|
| 38. |
Budair F. Non-drug related cutaneous hyperpigmentation in a patient with malaria, Saudi. J Dermatol Dermatol Surg 2014;18:49-51.
[Google Scholar]
|
| 39. |
Alsanad S, Aboushanab T, Khalil M, Alkhamees OA. A descriptive review of the prevalence and usage of traditional and complementary medicine among Saudi diabetic patients. Scientifica (Cairo) 2018;2018:6303190.
[Google Scholar]
|
| 40. |
Bedi MK, Shenefelt PD. Herbal therapy in dermatology. Arch Dermatol 2002;138:232-42.
[Google Scholar]
|
| 41. |
al-Saleh I, al-Doush I. Mercury content in skin-lightening creams and potential hazards to the health of Saudi women. J Toxicol Environ Health 1997;51:123-30.
[Google Scholar]
|
| 42. |
Abanmi AA, Al Zouman AY, Al Hussaini H, Al-Asmari A. Prayer marks. Int J Dermatol 2002;41:411-4.
[Google Scholar]
|
| 43. |
O'Goshi KI, Aoyama H, Tagami H. Mucin deposition in a prayer nodule on the forehead. Dermatology 1998;196:364.
[Google Scholar]
|
| 44. |
Buchwald D, Caralis PV, Gany F, Hardt EJ, Muecke MA, Putsch RW. The medical interview across cultures. Patient Care 1992;27:141-66.
[Google Scholar]
|
| 45. |
World Health Organization & UNAIDS. Male circumcision: global trends and determinants of prevalence, safety and acceptability. Geneva: World Health Organization. 2008. Available from: http://www.who.int/iris/handle/10665/43749. [Last retrieved on 2009 Mar 04]
[Google Scholar]
|
| 46. |
Ben Chaim J, Livne PM, Binyamini J, Hardak B, Ben-Meir D, Mor Y, et al. Complications of circumcision in Israel: A one year multicenter survey. Isr Med Assoc J 2005;7:368-70.
[Google Scholar]
|
| 47. |
Rehman J, Ghani M, Shehzad K, Sheikh I. Circumcision – A comparative study. Pak Armed Forces Med J 2007;57:286-8.
[Google Scholar]
|
| 48. |
Weiss HA, Larke N, Halperin D, Schenker I. Complications of circumcision in male neonates, infants and children: A systematic review. BMC Urol 2010;10:2.
[Google Scholar]
|
| 49. |
Wolbarst AL. Circumcision and penile cancer. Lancet 1932;219:150-3.
[Google Scholar]
|
| 50. |
Mallon E, Hawkins D, Dinneen M, Francics N, Fearfield L, Newson R, et al. Circumcision and genital dermatoses. Arch Dermatol 2000;136:350-4.
[Google Scholar]
|
| 51. |
Cook LS, Koutsky LA, Holmes KK. Clinical presentation of genital warts among circumcised and uncircumcised heterosexual men attending an urban STD clinic. Genitourin Med 1993;69:262-4.
[Google Scholar]
|
| 52. |
Darr A. Consanguineous Marriage and Inherited Disorders. University of Bradford: City of Bradford. Available from: https://www.bradford.gov.uk/media/1901/hgsg-briefing-paper-consanguineous-marriage.pdf. [Last retrieved on 2016 Aug 31].
[Google Scholar]
|
| 53. |
Alenizi DA. Consanguinity pattern and heritability of vitiligo in Arar, Saudi Arabia. J Family Community Med 2014;21:13-6.
[Google Scholar]
|
| 54. |
Budair F, Aljabre S, Alquorain N, Al-Nafea N, Aljabre A, AL-Buraey A. A survey of cutaneous findings in newborns in Saudi Arabia. J Dermatol Dermatol Surg 2017;21:53-7.
[Google Scholar]
|
| 55. |
Nakano A, Lestringant GG, Paperna T, Bergman R, Gershoni R, Frossard P, et al. Junctional epidermolysis bullosa in the Middle East: Clinical and genetic studies in a series of consanguineous families. J Am Acad Dermatol 2002;46:510-6.
[Google Scholar]
|
| 56. |
Al-Naamani A, Al-Waily A, Al-Kindi M, Al-Awadi M, Al-Yahyaee SA. Transglutaminase-1 mutations in Omani families with lamellar ichthyosis. Med Princ Pract 2013;22:438-43.
[Google Scholar]
|
| 57. |
Ben Halim N, Hsouna S, Lasram K, Rejeb I, Walha A, Talmoudi F, et al. Differential impact of consanguineous marriages on autosomal recessive diseases in Tunisia. Am J Hum Biol 2016;28:171-80.
[Google Scholar]
|
Fulltext Views
10,168
PDF downloads
2,732





