Translate this page into:
Dermoscopic criteria for differentiating exogenous ochronosis from melasma
Correspondence Address:
Niti Khunger
Department of Dermatology and STD, V.M. Medical College and Safdarjang Hospital, New Delhi - 110 029
India
| How to cite this article: Khunger N, Kandhari R. Dermoscopic criteria for differentiating exogenous ochronosis from melasma. Indian J Dermatol Venereol Leprol 2013;79:819-821 |
Sir,
There has been a sudden rise in the number of reported cases of exogenous ochronosis (EO), [1],[2],[3] and it may not be as uncommon as previously thought. In the early stages, it is clinically difficult to distinguish EO from melasma. A worsening of pigmentation due to EO can lead to paradoxical increased application of skin lightening agents, further aggravating the condition. Thus, it is essential to distinguish early EO from melasma. The gold standard for diagnosis of EO is a skin biopsy. Dermoscopy may be an important tool to differentiate EO from melasma, and may assist in choosing the appropriate site for biopsy in suspected cases. Two cases of EO following the use of skin lightening agents for the treatment of melasma are reported and dermoscopic criteria for diagnosis are being put forward.
A 48-year-old Indian woman, Fitzpatricks skin type IV, presented with erythema, and gradual deterioration of her melasma. She was using sunscreens and skin lightening agents containing 2% hydroquinone in an unsupervised manner since 8 years. She noted worsening of her melasma since the past 3 years.
The second case was a 42-year-old, Indian woman, skin type IV diagnosed with melasma 14 years back. She was treated with modified Kligman′s formula containing 2% hydroquinone, 0.025% tretinoin, 1% hydrocortisone, sunscreens, and glycolic acid peels. She continued use of skin lightening agents unsupervised for 13 years, and presented with worsening of her melasma.
On clinical examination, both cases revealed grayish brown macules with interspersed "confetti like" hypo-pigmented macular areas on the malar region, a speckled pattern of pigmentation [Figure - 1]a-d and a coarse texture with pinpoint, dark brown papules, which were more appreciable on palpation [Figure - 1]d. In addition, case one, revealed erythema and fine telangiectasias on bilateral malar areas, whereas case two revealed mild atrophy of the malar regions and a mild bluish black hue of bilateral zygomatic regions. There was no clinical or laboratory evidence of alkaptonuria in both cases. 3 mm punch biopsies taken from the pinpoint papular lesions revealed characteristic short, stout, curvilinear, "banana-shaped," ochre-colored fibers of varying thickness in the papillary dermis [Figure - 1]f. Methylene blue staining showed dark blue staining of the ochronotic fibers [Figure - 1]e. There was evidence of solar elastosis in both cases. Both cases were clinical stage II as per Dogliotti staging. [4] Dermoscopic examination of both patients in areas with melasma without ochronosis revealed an accentuation of the normal pseudo-rete of the facial skin. In areas with ochronosis, greyish brown dark amorphous structures in the perifollicular region and some obliterating the follicular openings were observed. The pattern was curvilinear and "worm like" in some areas [Figure - 2]. There was a clear demarcation between melasma and exogenouss ochronosis on dermoscopy [Figure - 3]a-d.
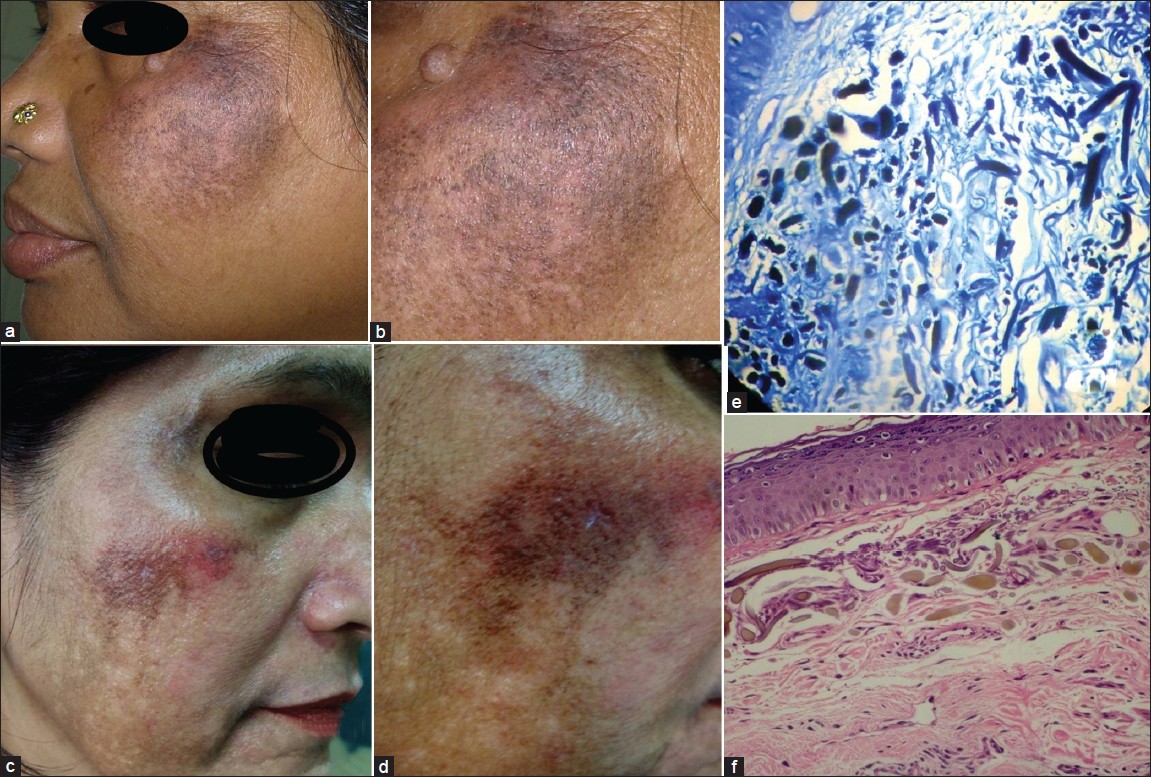 |
| Figure 1: (a) Ochronosis in case 1 showing grayish brown macules with interspersed "confetti like" depigmented macular areas with erythema on the cheeks. (b) Close-up view showing speckled pattern of hyperpigmentation with a coarse texture and pinpoint, dark brown papules. (c) Bluish grey to brown macules and papules with interspersed "confetti like" depigmented macular areas. (d) Tiny pinpoint caviar like brown papules with telangiectasia. (e) Methylene blue staining showing ochronotic fi bers stained dark blue. (f) Characteristic short, stout, curvilinear, "banana-shaped," ochre-colored fi bers of varying thickness in the papillary and upper dermis |
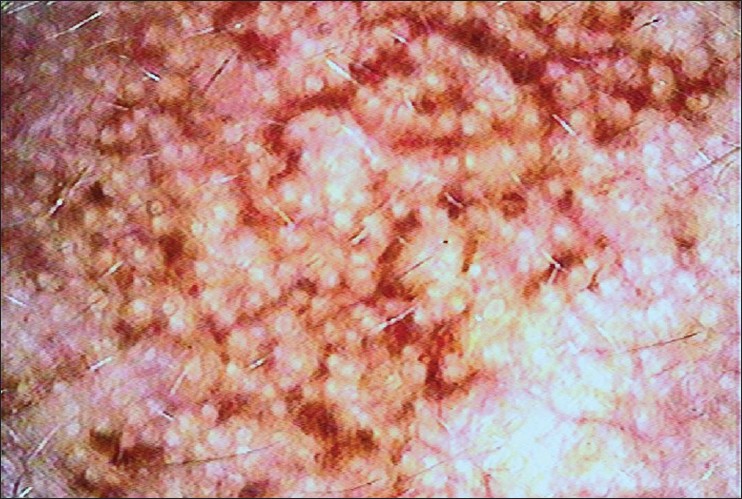 |
| Figure 2: Dermoscopic features of ochronosis showing dark brown globules, elongated and curvilinear-worm like structures conjoined together in a reticulate pattern of ochronosis |
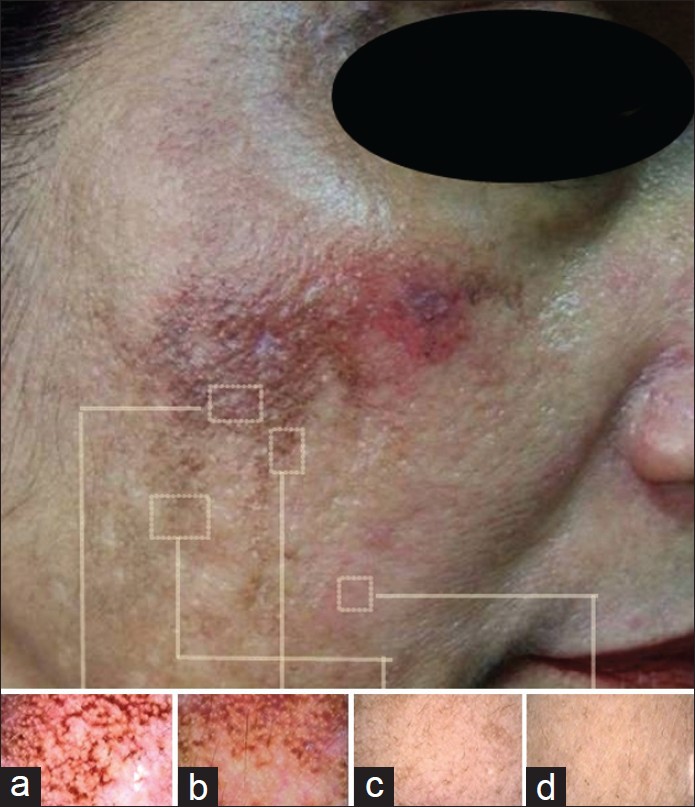 |
| Figure 3: (a) Ochronosis. (b) Sharp contrast between ochronosis in the upper half and melasma in the lower half. (c) Areas of melasma without ochronosis, showed accentuation of the normal pseudo-rete pattern with a diffuse brown pigmentation. (d) Normal skin |
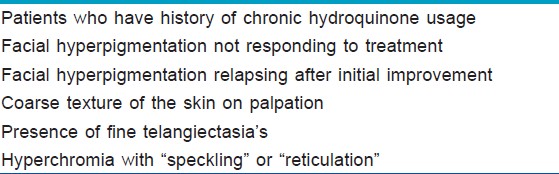
EO is clinically characterized by an asymptomatic hyperchromia of the skin, usually on the sun exposed areas of the face, back, and the extensor surfaces of the extremities. Tan et al. [5] recently reported variable clinical presentations of EO. Due to its varied presentation and striking similarity to melasma, especially in the early stages, clinicians require a high index of suspicion in order to make a diagnosis [Table - 1]. An early diagnosis is important as worsening of pigmentation may lead to application of increased concentration of hydroquinone rather than terminating it immediately.
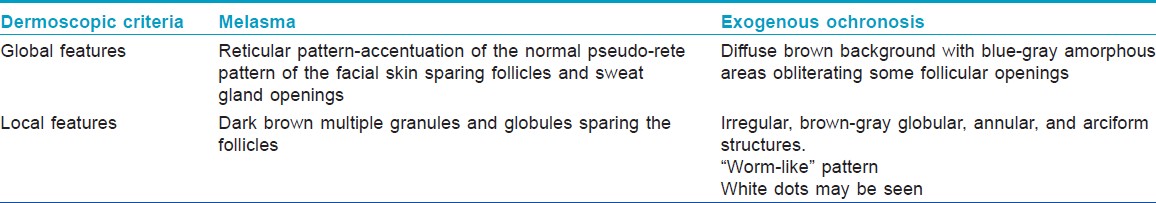
Charlín et al. [3] reported dermoscopic features of two patients with EO, wherein they observed blue-gray amorphous areas obliterating some follicular openings. Gil et al. [6] reported the dermoscopic features as irregular, brown-gray, globular, annular, and arciform structures. This was confirmed using a reflectance confocal microscope. Berman et al. [7] reported dark brown globules and globular-like structures on a diffuse brown background, in patients having EO, whereas those with melasma demonstrated a fine brown reticular pattern on a background of a faint light brown structure less area. Our dermoscopic findings were similar to previously reported findings. In addition, we observed a characteristic "worm-like" pattern. Thus, the dermoscopic features of EO are clearly distinct from melasma [Table - 2].
Hence, dermoscopy can be employed as a rapid screening test for EO. The clinical presence of coarse texture of the skin, fine telangiectasias and hyperchromia with "speckling" or "reticulation" [3] should alert the clinician to resort to a dermoscopic examination, particularly in patients who are reluctant to get a facial biopsy.
To conclude, dermoscopy can be used as a rapid, non-invasive tool to detect EO, and may be a useful guide in the selection for the appropriate site for biopsy in patients with pre-existing melasma.
| 1. |
Tan SK. Exogenous ochronosis in ethnic Chinese Asians: A clinicopathological study, diagnosis and treatment. J Eur Acad Dermatol Venereol 2011;25:842-50.
[Google Scholar]
|
| 2. |
Ribas J, Schettini AP, Cavalcante Mde S. Exogenous ochronosis hydroquinone induced: A report of four cases. An Bras Dermatol 2010;85:699-703.
[Google Scholar]
|
| 3. |
Charlín R, Barcaui CB, Kac BK, Soares DB, Rabello-Fonseca R, Azulay-Abulafia L. Hydroquinone-induced exogenous ochronosis: A report of four cases and usefulness of dermoscopy. Int J Dermatol 2008;47:19-23.
[Google Scholar]
|
| 4. |
Dogliotti M, Leibowitz M. Granulomatous ochronosis - A cosmetic-induced skin disorder in Blacks. S Afr Med J 1979;56:757-60.
[Google Scholar]
|
| 5. |
Tan SK. Exogenous ochronosis - A diagnostic challenge. J Cosmet Dermatol 2010;9:313-7.
[Google Scholar]
|
| 6. |
Gil I, Segura S, Martínez-Escala E, Lloreta J, Puig S, Vélez M, et al. Dermoscopic and reflectance confocal microscopic features of exogenous ochronosis. Arch Dermatol 2010;146:1021-5.
[Google Scholar]
|
| 7. |
Berman B, Ricotti C, Vieira M, Amini S. Differentiation of exogenous ochronosis from melasma by dermoscopy. J Am Acad Dermatol. 2009;60(Suppl 1):AB2.
[Google Scholar]
|
Fulltext Views
17,490
PDF downloads
4,744





