Translate this page into:
Dermoscopic features of trichilemmal carcinoma
2 Department of Plastic and Reconstructive Surgery, Celal Bayar University, Manisa, Turkey
3 Department of Pathology, Faculty of Medicine, Celal Bayar University, Manisa, Turkey
Correspondence Address:
Aylin Türel Ermertcan
Department of Dermatology, Faculty of Medicine, Celal Bayar University, 45010 Manisa
Turkey
| How to cite this article: Arslan Z, Bali Z U, Evrenos M K, Temiz P, Ermertcan AT. Dermoscopic features of trichilemmal carcinoma. Indian J Dermatol Venereol Leprol 2019;85:321-323 |
Sir,
Trichilemmal carcinoma is a rare skin tumor that originates from the external root sheath of the hair follicle, commonly located on the scalp, forehead, neck, trunk or the upper extremities, affecting predominantly the sun-exposed areas of the skin. It usually manifests in the elderly and more commonly in females than males.[1]
A 72-year-old man with the complaint of bleeding mass on his left neck since 2 years presented to our dermatology clinic. He explained that his lesion had been bleeding for 2 months and enlarging slowly. Dermatologic examination revealed an erythematous, hemorrhagic and ulcerated nodule on the left neck region of size 4 × 4 cm [Figure - 1].
 |
| Figure 1: Erythematous, hemorrhagic and ulcerated nodule on the left neck region |
Dermoscopic examination was performed with MoleMax 3, a nonpolarized, computer-based video dermoscope with ×30 magnification. It revealed multiple large and thin vessels with a yellowish white structureless area behind the vessels. There was no pigmented area [Figure - 2]. Dermoscopic view of the tumor suggested a basal cell carcinoma. Excisional skin biopsy was performed by Plastic and Reconstructive Surgery Department with a margin of 1 cm.
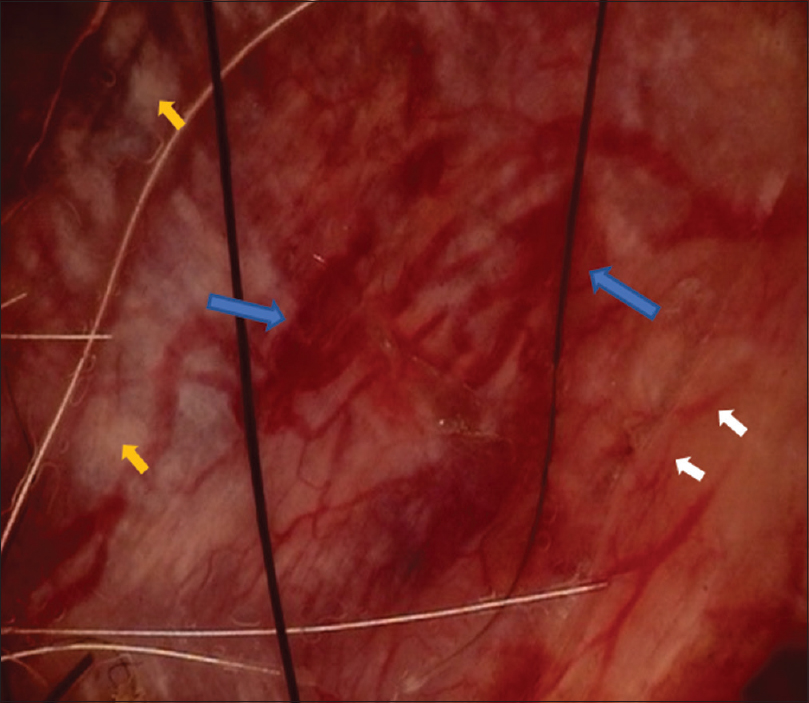 |
| Figure 2: Dermoscopic examination revealing multiple large and thin vessels and yellowish white structureless area behind the vessels. Blue arrows: large vessels, white arrows: thin vessels, yellow arrows: yellowish-white structureless area. (MoleMax 3, non-polarized videodermoscope, ×30 magnification) |
On histopathological examination, diffuse, trabecular or island-like infiltrative tumoral lesion was seen under ulcerated epidermis. The tumor was composed of mostly basaloid cells and cells with clear cytoplasm [Figure - 3] and [Figure - 4]. The tumor cells were periodic acid–Schiff stain positive [Figure - 5]. The mitotic rate was high and necrotic areas were observed in the middle of a few tumor islands. On cervical sentinel lymph node biopsy, nonspecific reactive lymphoid hyperplasia was reported. The diagnosis was performed as trichilemmal carcinoma according to the histopathological findings. Cervical magnetic resonance imaging examination revealed no pathological findings. The patient has been followed up clinically and by cervical ultrasonography at 2 months' intervals for 7 months. We did not detect any recurrence or metastasis.
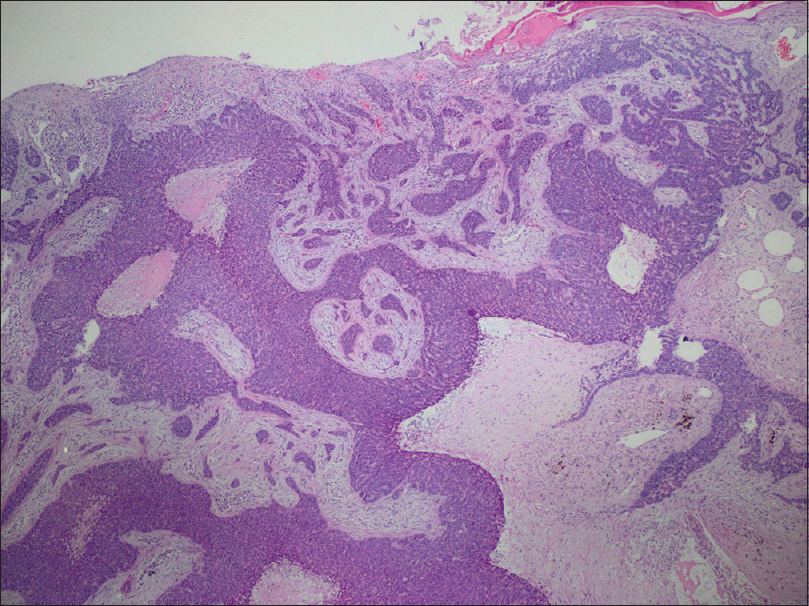 |
| Figure 3: Diffuse, trabecular or island-like growing infiltrative tumoral lesion composed of mostly basaloid cells and cells with clear cytoplasm (hematoxylin and eosin, ×40) |
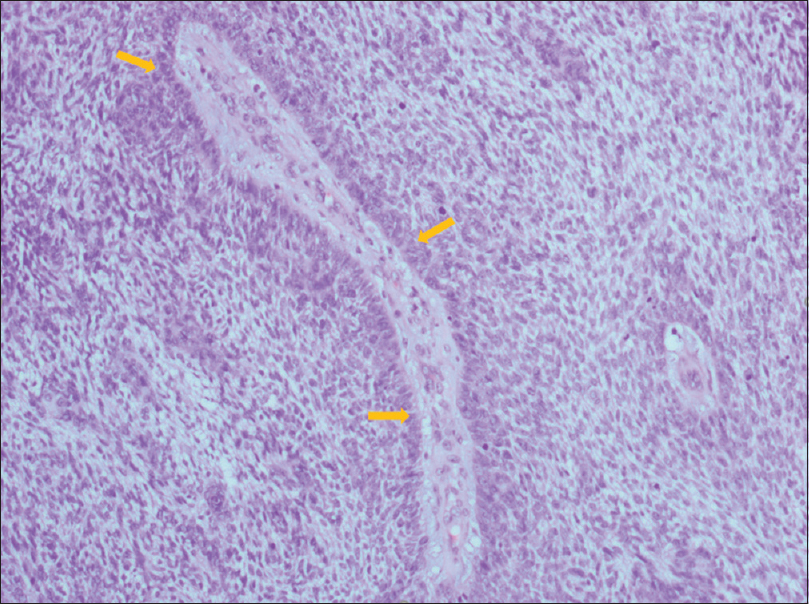 |
| Figure 4: Peripherally palisaded basaloid cells and cells with clear cytoplasm (hematoxylin and eosin H and E, ×100). Yellow arrows: palisading |
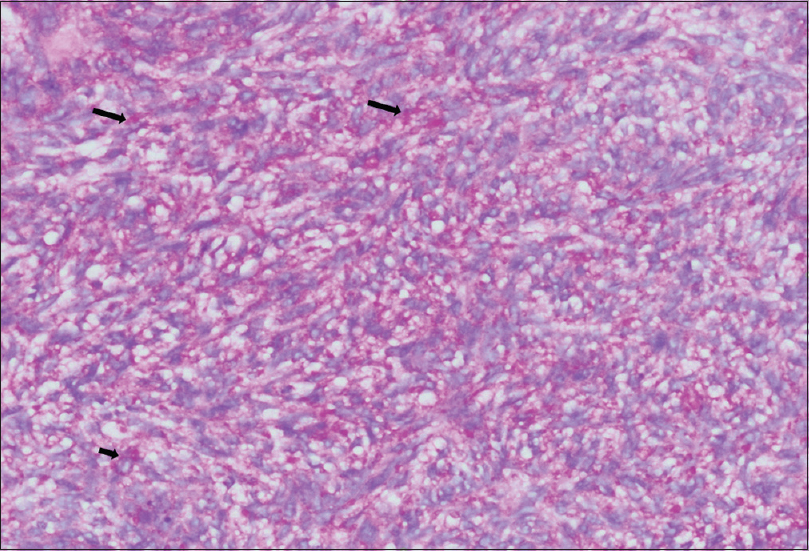 |
| Figure 5: Periodic acid–Schiff stain positive tumor cells (×200). Black arrows: PAS + areas |
Trichilemmal carcinoma is an uncommon cutaneous neoplasm that has been the subject of controversy in the dermatology literature as a malignant counterpart of trichilemmoma with approximately 100 reported cases. However, the number of cases of trichilemmal carcinoma may be overestimated, owing to the significant histopathologic overlap with clear cell squamous cell carcinoma. Histopathology of the tumor is characterized by the presence of clear cells with atypical nuclei and trichilemmal keratinization of tumor cell nests, and tumor cells are commonly periodic acid–Schiff stain positive. Differential diagnosis is very important to distinguish it from the other malignant tumors, such as squamous cell carcinoma, basal cell carcinoma, nodular melanoma or keratoacanthoma.[2],[3] These malignant tumors are more aggressive than trichilemmal carcinoma; they have a slower growth rate but a very distinctive histology. Wide local surgical excision should be considered as the primary modality of treatment.[4],[5] Multiple recurrences and metastasis to regional lymph nodes even after excision with clear resection margins have been reported. Since trichilemmal carcinoma has metastatic potential and usually recurs, careful follow- up for early detection of recurrence is needed.[6]
Although dermoscopic examination is very important to perform while considering the differential diagnosis of skin cancers, it is sometimes difficult to distinguish adnexal tumors from nonmelanoma skin cancers as in our case. Miyachi et al. reported a 96-year-old Japanese man with the diagnosis of proliferated trichilemmal tumor on the left parietal region of the scalp. Dermoscopic examination of the ulcerated nodule showed arborizing vessels, shiny white areas and purple hue with multiple shades of yellow coloration in the background.[7] The arborizing vessels are known as one of the significant dermoscopic findings of basal cell carcinoma; however, they may also be found in adnexal tumors.[8] Lallas et al. reported that the presence of the white structure is suggestive of adnexal tumors of follicular origin. They also reported that dermoscopic yellow structures are typically observed in sebaceous tumors with a homogenous yellow background with or without yellow lobules.[9] Some basal cell carcinomas also have yellow structures with lobule-like structures.[10]
The combination of thick and thin vessels, yellowish-white structureless area behind the vessels is an important dermoscopic feature for the diagnosis of adnexal tumors, particularly trichilemmal tumors.
We could not find any literature about dermoscopic findings of trichilemmal carcinoma. We suggest that further studies are needed on dermoscopic view of adnexal tumors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hamman MS, Brian Jiang SI. Management of trichilemmal carcinoma: An update and comprehensive review of the literature. Dermatol Surg 2014;40:711-7.
[Google Scholar]
|
| 2. |
Zhuang SM, Zhang GH, Chen WK, Chen SW, Wang LP, Li H, et al. Survival study and clinicopathological evaluation of trichilemmal carcinoma. Mol Clin Oncol 2013;1:499-502.
[Google Scholar]
|
| 3. |
Evrenos MK, Kerem H, Temiz P, Ermertcan AT, Yoleri L. Malignant tumor of outer root sheath epithelium, trichilemmal carcinoma. Clinical presentations, treatments and outcomes. Saudi Med J 2018;39:213-6.
[Google Scholar]
|
| 4. |
Romeu M, Foletti JM, Chossegros C, Dales JP, Berbis P, Cribier B, et al. Malignant cutaneous adnexal neoplasms of the face and scalp: Diagnostic and therapeutic update. J Stomatol Oral Maxillofac Surg 2017;118:95-102.
[Google Scholar]
|
| 5. |
Deshmukh BD, Kulkarni MP, Momin YA, Sulhyan KR. Malignant proliferating trichilemmal tumor: A case report and review of literature. J Cancer Res Ther 2014;10:767-9.
[Google Scholar]
|
| 6. |
Lee NR, Oh SJ, Roh MR. Trichilemmal carcinoma in a young adult. Indian J Dermatol Venereol Leprol 2015;81:531-3.
[Google Scholar]
|
| 7. |
Miyachi H, Togawa Y, Yamamoto Y, Oguma R, Suehiro K, Matsue H, et al. Proliferating trichilemmal tumour: A comparison of dermoscopic, ultrasonographic and histopathological features. Eur J Dermatol 2016;26:400-2.
[Google Scholar]
|
| 8. |
Martín JM, Bella-Navarro R, Jordá E. Vascular patterns in dermoscopy. Actas Dermosifiliogr 2012;103:357-75.
[Google Scholar]
|
| 9. |
Lallas A, Moscarella E, Argenziano G, Longo C, Apalla Z, Ferrara G, et al. Dermoscopy of uncommon skin tumours. Australas J Dermatol 2014;55:53-62.
[Google Scholar]
|
| 10. |
Bellucci C, Arginelli F, Bassoli S, Magnoni C, Seidenari S. Dermoscopic yellow structures in basal cell carcinoma. J Eur Acad Dermatol Venereol 2014;28:651-4.
[Google Scholar]
|
Fulltext Views
4,438
PDF downloads
2,326





