Translate this page into:
Dermoscopy combined with ink staining as one more method to diagnose nodular scabies
Correspondence Address:
Ping Wang
No. 38 West Lake Road, Shangcheng Zone, Hangzhou City, Zhejiang Province, 310009
China
| How to cite this article: Ma Y, Hu W, Wang P, Bian K, Liu Z. Dermoscopy combined with ink staining as one more method to diagnose nodular scabies. Indian J Dermatol Venereol Leprol 2019;85:324-325 |
Sir,
Scabies is caused by an infestation of Sarcoptes scabiei (S. scabiei var. hominis). It is important to make a prompt and accurate diagnosis of scabies and to provide appropriate treatment to prevent its spread and avoid unnecessary investigations.[1] Nevertheless, it is easy to misdiagnose during the clinical assessment. In this study, a simple and painless method which involves dermoscopy plus ink staining is applied to observe nodular scabies.
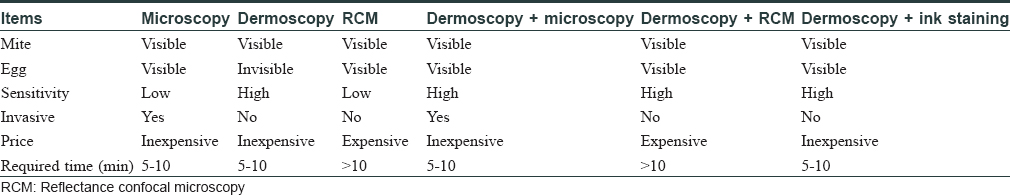
We present the case of a 3-year-old girl with reddish and itchy nodules of 5–6 mm on her trunk and proximal extremities of about 2 months duration. She had been diagnosed elsewhere to have eczema and was treated with hydrocortisone butyrate cream for 15 days. family history revealed that, her mother and grandparents also had itchy papular eruption on the interdigital web spaces of their hands for 1 month. In addition, dermoscopy (FotoFinder Systems GmbH, Bad Birnbach, Germany) showed a typical “jet with condensation trails” and “hang glider sign” (a brown triangle which corresponds to the gnathosoma and the two anterior pairs of forelimbs of the mite) [Figure - 1]a. We colored the burrow, used a syringe to add some drops of china ink into the lesions and then removed them with alcohol. As revealed by the results, the burrow had a mite egg and a hyaline mite [Figure - 1]b. The girl cried and struggled because her lesions were scraped with small tweezers and further dug. Using microscopic examination, we could only discover a mite egg. The patient was treated with sulfur cream (it was put on all involved parts except the part above the neck) for 3 consecutive days and hydrocortisone butyrate cream for 2 weeks. The lesions darkened and itching was eased. Finally, the diagnosis of nodular scabies was confirmed.
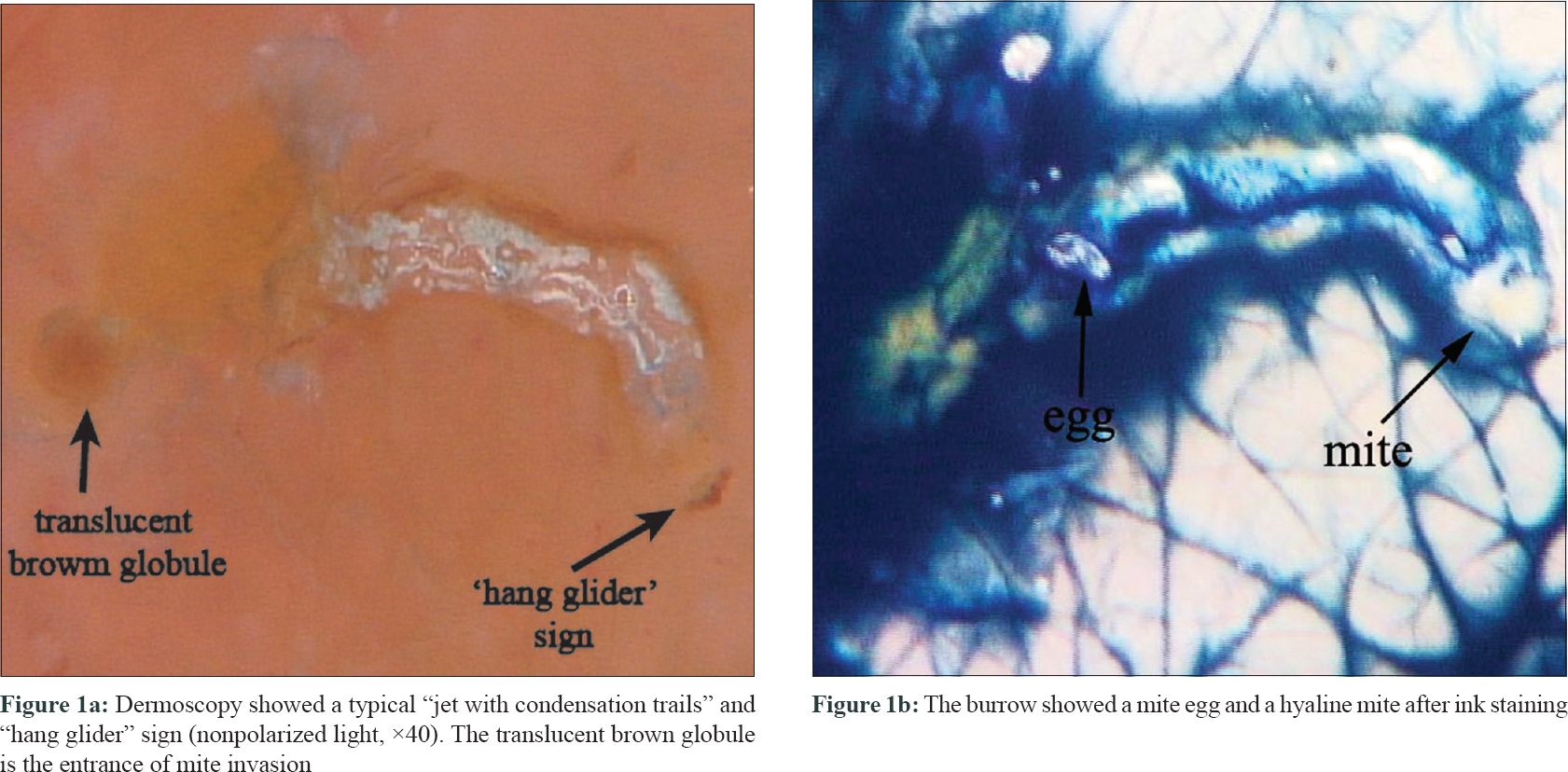 |
| Figure 1 |
At present, scabies is generally confirmed through the dermatoscopic detection of mites or the microscopic identification of mites, mite eggs or fecal matter (scybala) from skin scrapings.[2] identifying lesions through dermoscopic examination can enhance monitoring clinical response to treatment by observing mites and trails.[3] Because the abdomen and eggs of mites are transparent, they are hardly visible under dermoscopy.[1],[2] The combination method of dermoscopy plus ink staining can enhance the yield of the mites and their eggs to evaluate and monitor the progression of scabies, so that the accurate location for microscopic detection or reflectance confocal microscopy can be determined. If the pruritic nodules still persist after antiscabietic therapy and the effect of the above method is negative (failure to see any mites or eggs), we can initiate an anti-inflammatory therapy such as treating with hydrocortisone butyrate cream.
[Table - 1] compares the existing diagnostic methods of scabies.[1],[2],[3],[4],[5] In conclusion, the combination method of dermoscopy plus ink staining is a painless and simple method for enhancing the diagnosis of scabies as well as detecting response to treatment.
Declaration of patient consent
The authors certify that she has obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that their name and initial will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Executive Committee of Guideline for the Diagnosis and Treatment of Scabies. Guideline for the diagnosis and treatment of scabies in Japan (third edition): Executive committee of guideline for the diagnosis and treatment of scabies. J Dermatol 2017;44:991-1014.
[Google Scholar]
|
| 2. |
Sunderkötter C, Feldmeier H, Fölster-Holst R, Geisel B, Klinke-Rehbein S, Nast A, et al. S1 guidelines on the diagnosis and treatment of scabies – Short version. J Dtsch Dermatol Ges 2016;14:1155-67.
[Google Scholar]
|
| 3. |
Micali G, Lacarrubba F, Tedeschi A. Videodermatoscopy enhances the ability to monitor efficacy of scabies treatment and allows optimal timing of drug application. J Eur Acad Dermatol Venereol 2004;18:153-4.
[Google Scholar]
|
| 4. |
Cinotti E, Labeille B, Cambazard F, Biron AC, Chol C, Leclerq A, et al. Videodermoscopy compared to reflectance confocal microscopy for the diagnosis of scabies. J Eur Acad Dermatol Venereol 2016;30:1573-7.
[Google Scholar]
|
| 5. |
Micali G, Lacarrubba F, Verzì AE, Chosidow O, Schwartz RA. Scabies: Advances in noninvasive diagnosis. PLoS Negl Trop Dis 2016;10:e0004691.
[Google Scholar]
|
Fulltext Views
4,976
PDF downloads
2,143





