Translate this page into:
Dermoscopy of aggressive basal cell carcinomas
Correspondence Address:
Mirjana Popadic
Dermatovenereologist, Pasterova 2, Belgrade
Serbia
| How to cite this article: Popadic M. Dermoscopy of aggressive basal cell carcinomas. Indian J Dermatol Venereol Leprol 2015;81:608-610 |
Sir,
The histological subtype of basal cell carcinoma (BCC) is the most important factor used to determine the best treatment modality. Although up to 26 histological subtypes of basal cell carcinoma have been identified, only three of these (nodular, superficial and aggressive) are relevant to determining the appropriate treatment choice.[1] Superficial and nodular basal cell carcinoma, both usually demonstrate an indolent growth pattern and have a low-risk for incomplete treatment and recurrence. The third, a high-risk subtype, includes all basal cell carcinomas that exhibit aggressive-growth such as infiltrative, morpheaform, micronodular and basal cell carcinoma with squamous differentiation.[2] The “aggressive-growth” subtypes are characterized by an infiltrative growth pattern that has poor circumscription and tendency for perineural and perivascular invasion leading to difficulty in surgical eradication and consequent high recurrence rates.[2]
Early diagnosis and accurate treatment are essential to reduce morbidity and prevent recurrence/metastasis. Dermoscopic examination, by providing additional morphological information, can aid the clinical diagnosis of basal cell carcinoma. However, the significance of dermoscopy in determining the aggressiveness of basal cell carcinoma remains to be elucidated.
The aim of the present study was to evaluate the dermoscopic patterns of aggressive basal cell carcinoma and to investigate the possible role of dermoscopy in identifying the aggressive nature of the tumor.
Seven histopathologically proven aggressive basal cell carcinomas (4 morpheaform and 3 infiltrative) were identified and closely analyzed, using DermLite FOTO Equipment at 10-fold magnification.[3] Each aggressive tumor was evaluated for the presence of various dermoscopic features relevant for the diagnosis of basal cell carcinoma. In mixed-type lesions, the superiority rule was applied according to the most unfavorable subtype: aggressive > nonaggressive. Almost all were primary tumors except one that was a recurrent basal cell carcinoma (infiltrative type).
Males were predominantly affected in both variants of aggressive tumors [Table - 1]. Patients with infiltrative basal cell carcinoma were older (mean age 72 years; range 65–76 years) than patients with morpheaform basal cell carcinoma (mean age 66.5 years; range 51–78 years).
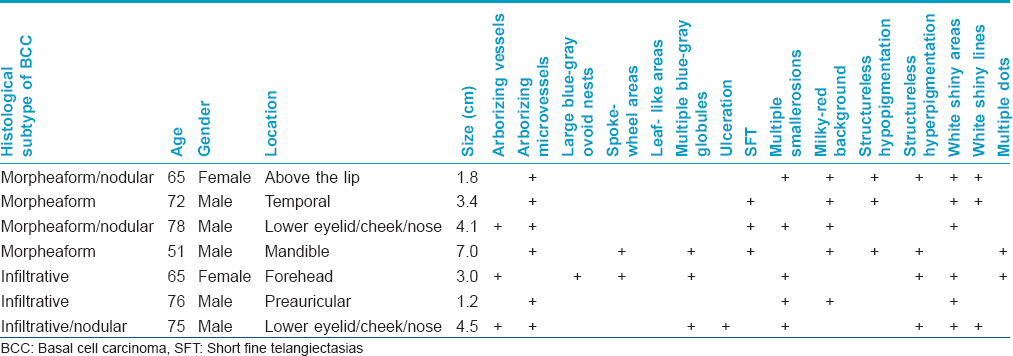
All tumors were located in the head/neck region. Morpheaform basal cell carcinomas were larger (mean diameter 4.07 cm; range, 1.8–7 cm) than infiltrative basal cell carcinoma (mean diameter 2.9 cm; range, 1.2–4.5 cm), with a longer history of duration (78 months, range = 36–120 months), compared to infiltrative basal cell carcinomas (8.7 months, range = 2–12 months) [Table - 1].
The most frequently detected features in morpheaform basal cell carcinoma were milky-red background and arborizing microvessels (4/4, 100%), followed by short fine telangiectasias (SFT), white areas and structureless hypopigmentation (3/4, 75%). Structureless hyperpigmentation, white lines and multiple erosions were rarer findings (2/4, 50%) [Figure - 1] and [Figure - 2].[3]
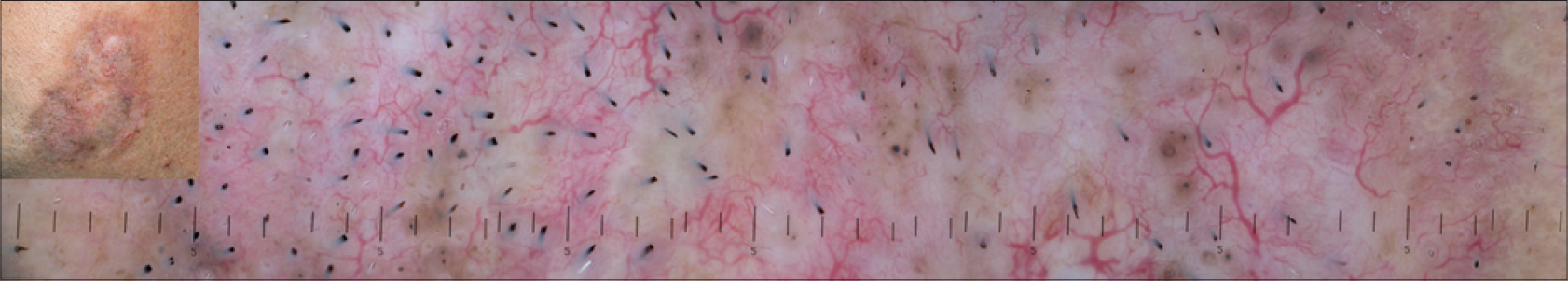 |
| Figure 1: Morpheaform basal cell carcinoma. On dermoscopy, numerous arborizing telangiectatic vessels and areas of structureless hypo/hyperpigmentation are seen |
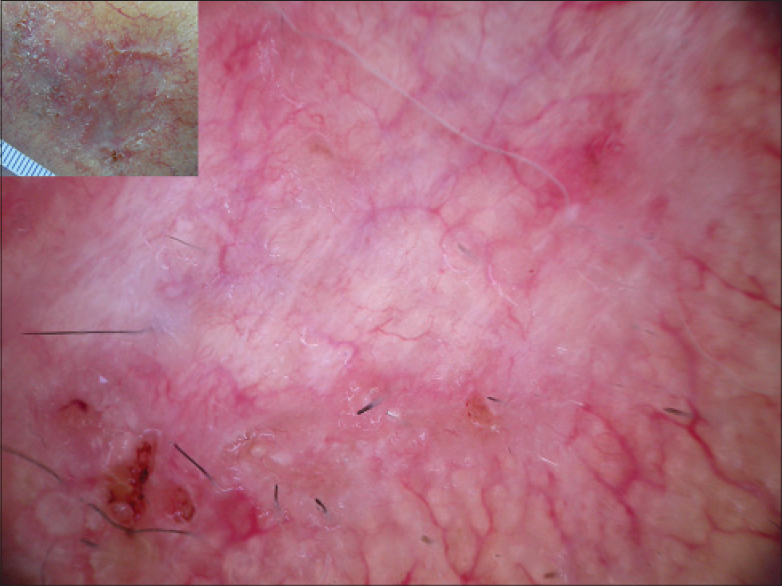 |
| Figure 2: Morpheaform basal cell carcinoma. On dermoscopy, a milky-red background, with arborizing telangiectatic vessels, short fine telangiectatic vessels, white lines, structureless hypopigmentation and multiple small erosions are seen |
All three infiltrative basal cell carcinomas demonstrated multiple erosions and white areas (3/3, 100%). Arborizing vessels/microvessels, multiple blue-gray globules and structureless hyperpigmentation were found in 2 of 3 (66.7%) infiltrative basal cell carcinomas [Figure - 3]a and [Figure - 3]b.[3]
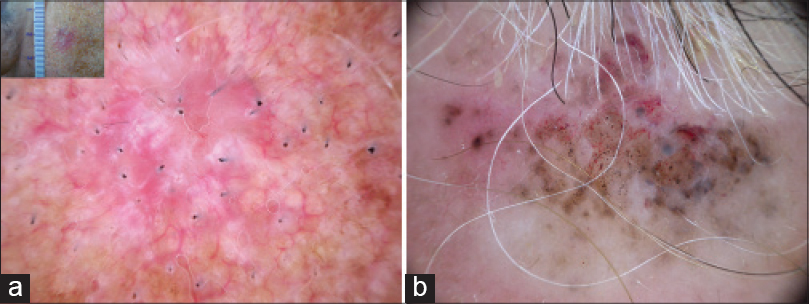 |
| Figure 3: Infiltrative basal cell carcinomas. (a) Flat clinical presentation with typical dermoscopic features in thin tumors (milky-red background, short fine telangiectatic vessels) in combination with white structures. (b) Nodular clinical presentation: Numerous pigmented features with structureless hypo/hyperpigmentation are identified |
Pyne et al., established that aggressive basal cell carcinoma tends to have no or less pink within the tumor area and absent or few vessels in the central tumor area compared to other subtypes.[4] A recent study that investigated correlation of dermoscopic findings with different histopathologic variants of basal cell carcinoma showed that dermoscopy had a low sensitivity to detect risk of recurrence.[5] Arborizing vessels was found to be the main dermoscopic finding in infiltrative basal cell carcinoma and truncated vessels and globules in micronodular basal cell carcinoma.[5]
This article confirms that dermoscopy is useful in the detection of basal cell carcinoma with limited impact in discriminating aggressive basal cell carcinomas from the non-aggressive ones. Detailed dermoscopic analysis did not reveal any distinct feature that would point to the aggressive nature of tumors. In the infiltrative basal cell carcinomas that were evaluated, the presence of dermoscopic features correlated with tumor thickness. In the clinically thicker parts of infiltrative basal cell carcinomas, multiple erosions and pigmented features were identified, whereas in the thin parts of tumors white areas were frequently found.
Similar dermoscopic features were also seen in morpheaform basal cell carcinomas with one important difference, the flat parts of tumors had well developed, branched arborizing vessels, in contrast to the domination of short fine telangiectasias in flat, superficial basal cell carcinoma. This could be explained by deeper infiltration of tumor cells and consequently increasing vascular needs of the tumor tissue. Furthermore, white areas/lines were a striking feature, also localized to the flat parts of lesions. This probably correlates with prominent collagen in the tumor stroma of morpheaform basal cell carcinoma.
In conclusion, dermoscopy appears to be of limited diagnostic value to determine the aggressive histological nature of basal cell carcinoma, though larger comparative studies are required to ascertain its value.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Wade TR, Ackerman AB. The many faces of basal-cell carcinoma. J Dermatol Surg Oncol 1978;4:23-8.
[Google Scholar]
|
| 2. |
Crowson AN. Basal cell carcinoma: Biology, morphology and clinical implications. Mod Pathol 2006;19 Suppl 2:S127-47.
[Google Scholar]
|
| 3. |
Popadic M. Dermoscopic features in different morphologic types of basal cell carcinoma. Dermatol Surg 2014;40:725-32.
[Google Scholar]
|
| 4. |
Pyne J, Sapkota D, Wong JC. Aggressive basal cell carcinoma: dermatoscopy vascular features as clues to the diagnosis. Dermatol Pract Concept 2012;2:203a02.
[Google Scholar]
|
| 5. |
Verduzco-Martínez AP, Quiñones-Venegas R, Guevara-Gutiérrez E, Tlacuilo-Parra A. Correlation of dermoscopic findings with histopathologic variants of basal cell carcinoma. Int J Dermatol 2013;52:718-21.
[Google Scholar]
|
Fulltext Views
4,013
PDF downloads
1,528





