Translate this page into:
Dermoscopy of topical steroid-dependent or damaged face: A cross-sectional study
Corresponding author: Dr. R. Jindal, Department of Dermatology, Venereology and Leprosy, Himalayan Institute of Medical Sciences, Swami Rama Himalayan University, Dehradun, Uttarakhand, India. rashmijindal98@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sethi S, Chauhan P, Jindal R, Bisht YS. Dermoscopy of topical steroid-dependent or damaged face: A cross-sectional study. Indian J Dermatol Venereol Leprol 2022;88:40-6.
Abstract
Background:
Topical corticosteroid (TCS) abuse is rampant and results in steroid addiction labeled as topical steroid-dependent or damaged face (TSDF). Indian market is replete with triple combination creams containing TCS sold as over-the-counter products at low cost, luring people to use them without prescription. The resultant damage if detected late is irreversible and difficult to treat. Dermoscopy can help in the early identification of features of TSDF at a preclinical stage resulting in better prognosis. However, the literature on the same is limited.
Aims:
This study is undertaken to characterize dermoscopic features of TSDF and to correlate them with potency and duration of application of the TCS.
Methods:
One hundred and thirty-two patients aged 18 years or above, with clinical symptoms and signs suggestive of TSDF and with history of application of TCS on the face for a period of more than one month, were enrolled in the study. Their demographic details, clinical features, and dermoscopy findings were recorded using a predesigned structured format. Comparison of dermoscopic findings with clinical examination, gender, potency of TCS, and duration of TCS use was done using Chi-square test, Fisher’s exact test, and one-tailed Z-test.
Results:
Mean age of the patients was 31.7 ± 8.1 years. Male to female ratio was 2:9. Sixty-nine (52.3%) patients abused TCS for more than one year. Clinical findings noted in the patients were erythema (81.1%), hyperpigmentation (80.3%), and hypertrichosis (68.2%). The most common dermoscopy findings seen were brown globules (96.2%), red diffuse areas (92.4%), vessels (87.1%), white structureless areas (86.4%), and hypertrichosis (80.3%). Red diffuse areas, vessels, brown globules, white structureless areas, and white hair were observed in a statistically higher proportion of cases dermoscopically. Y-shaped vessels and brown globules were seen in significantly higher number of patients, using TCS for more than three months and in those continuing it beyond six months, polygonal vessels were predominant.
Limitations:
Lack of histopathological correlation is the limitation of our study. Furthermore, brown globules seen in 96.2% patients of TSDF on dermoscopy may have been over-estimated and not always signify TSDF; instead, it could represent melasma for which patient applied TCS.
Conclusion:
Dermoscopy in TSDF can help dermatologists in a multitude of ways from confirming the diagnosis to differentiating from other causes of red face and predicting the approximate duration of TCS abuse.
Keywords
Dermoscopy
red face
telangiectasias
topical corticosteroids
topical steroid-dependent or damaged face
Plain language summary
Topical steroid dependent or damaged face (TSDF) is an alarming upcoming entity rampant in India due to over-the-counter availability of topical corticosteroids containing products. Face being the conspicuous part of the body, it is subjected to use of various products upon recommendation by non-medical community. The aim of this study is to use dermoscopy in patients with TSDF in an attempt to identify pre-clinical characteristics. We found the presence of brown globules, red diffuse areas, vessels and white structureless globules in our patients. dermoscopy can thus be used in differentiating TSDF from other causes of red face, especially when history of abuse is not forthcoming. Further, female gender and prolonged application of topical steroids appear to affect the changes seen dermoscopically. The photographic evidence can be used to educate the patients about the harm done by topical steroids to prevent further abuse.
Introduction
A new era in therapeutic dermatology emerged in 1952 with the unveiling of the first topical corticosteroid (TCS). A number of steroid molecules of varying potencies, from super-potent to those with the least potency, have been developed since then, rendering the treatment of many inflammatory dermatoses feasible.1 Corticosteroids have anti-inflammatory, immunosuppressive, anti-pruritic, and melanopenic action.2,3 Although immensely beneficial, TCS have proved to be double-edged swords. They have been misused in varying extent by pharmacies and pharmaceutical, companies, by those who prescribe (who may not always be doctors or dermatologists), and by the general population.1 Face is the most common site of such misuse, with the resultant steroid addiction leading to a phenomenon labeled as “topical steroid-dependent or damaged face” (TSDF).4 TCS are used on the face as wonder compounds with the belief that they can correct any flaw or imperfection. On the contrary, they produce a red face after a variable duration, treating which becomes a battle for both the patients and the dermatologist.5 The onus of countering this menace behoves on the dermatologists. There is a need for early, identification of the signs of TSDF before they become irreversible. Dermoscopy can act as the modern-day instrument for early detection of subclinical signs of TSDF by delineating characteristic features such as polygonal vessels and telengiectasias, structureless white areas (atrophy), hypertrichosis, scales, and erythema.6 This study is undertaken to characterize dermoscopic features of TSDF and to correlate them with potency and duration of application of the TCS.
Methods
Patients (18 years or above) with clinical symptoms and signs suggestive of TSDF (redness, itching, acne, burning, swelling, photosensitivity, pigmentation and atrophy) and with history of application of TCS on the face for a period of more than one month presenting to Himalayan Institute of Medical Sciences (Dehradun) were included in the study after obtaining written informed consent. Institutional Ethics Committee approval was obtained before the commencement of the study (SRHU/Reg/ Int/2019-76). History of rosacea, pre-existing comorbidities (e.g., Cushing’s syndrome, polycystic ovaries, and thyroid disorders), pregnancy, and ongoing treatment with oral corticosteroids were the exclusion criteria. Sample size of 132 cases was calculated by z2pq/d2 where z = 1.96 with 95% confidence interval, p (estimated prevalence) = 90.5%, q = 1-p, d = 5.7 Data regarding demographics, source of TCS prescription, potency, and duration of TCS used was recorded. A patient was labeled literate if he was able to read and write with understanding in any language. In patients with a history of using multiple topical steroids of various potencies, the preparation with the highest potency used was considered for statistical analysis. However, when a more potent steroid was applied for less than one month, the preparation used beyond one month was considered for analysis. Patients were subjected to dermoscopic evaluation with both polarized and non-polarized modes. Dermoscopic images were captured with iPhone X (12-megapixel camera; Apple Inc., Cupertino, California) attached to Dermlite DL200 hybrid, ×10 magnification (3Gen, San Juan Capistrano, California). Patients were later counseled about the harmful effects of TCS abuse. Statistical analysis was carried out using statistical package for social sciences version 20. Comparison of dermoscopic findings with clinical examination, gender, and potency of TCS was done using Chi-square test and Fisher’s exact test with a “P” < 0.05 considered significant. Comparison of dermoscopic findings on the basis of duration of TCS applied was done using one-tailed Z-test for sample proportion.
Results
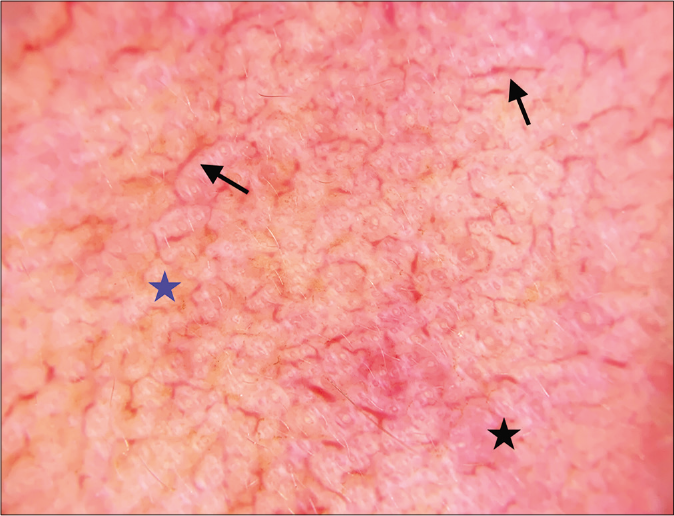
A total of 132 patients were recruited in the study. Females (108,81.8%) constituted the majority with a male to female ratio of 2:9. Most of the patients belonged to the age group of 18–30 years (66,50%) with a mean age of 31.6 ± 8.1 years. One hundred and seven (81.1%) patients had received some form of formal education, while 25 (18.9%) patients were illiterate. Presenting complaints of the patients were redness in 107 (81.1%), itching in 102 (77.3%), pigmentation in 87 (65.9%), burning in 84 (63.6%) and acne in 47 (35.6%) patients. Duration of TCS application ranged from one month to 25 years with 69 (52.3%) patients having applied TCS for over one year. Most patients, (74,56.1%) started using TCS on the recommendation of relatives and friends [Table 1]. Several patients (95, 71.9%) gave a history of using multiple topical steroids of various potencies. Based on the potency of TCS used, patients were categorized into two groups: One using class I/II (54, 40.9%) potency TCS and the other using class III and above (78, 59.1%). Acne (56, 42.4%) and melasma (47, 35.6%) were the most common underlying diseases for which TCS were used. Further, 13 (9.8%) patients used TCS for tinea faciei and 34 (25.8%) as fairness creams or routine face creams. Clinical findings noted in the patients were erythema in 107 (81.1%), hyperpigmentation in 106 (80.3%), and hypertrichosis in 90 (68.2%) followed by telangiectasia in 63 (47.7%) and wrinkles in 47 (35.6%) [Table 2 and Figure 1]. The most common dermoscopy findings seen were brown globules in 127 (96.2%), red diffuse areas in 122 (92.4%), vessels in 115 (87.1%), white structureless areas in 114 (86.4%), hypertrichosis in 106 (80.3%), breaking of pseudo-reticular network in 99 (75%), and white hair in 82 (62.1%) patients [Figures 2 and 3]. Type of vessels seen was linear without bends and branches in 62 (46.9%), serpentine in 97 (73.5%), polygonal in 43 (32.6%), and Y-shaped in 33 (25%) cases. Polygonal and Y-shaped vessels, though, are categorized under linear vessels with branches, the term Y-shaped vessel was used when only one lateral branch was visible and polygonal vessel was used if multiple branches forming a network were seen. Comparison of dermoscopy findings with their corresponding clinical finding revealed that red diffuse areas, vessels, brown globules, white structureless areas, desquamation, hypertrichosis and white hair were observed in a statistically higher proportion of cases dermoscopically [Table 2]. Dermoscopic findings found significantly more in males as compared to females were fine vessels and pustules, whereas, in females, branched vessels were predominant. Almost all the dermoscopy findings were seen in a higher proportion of patients using class III or above potency TCS; however, this failed to achieve statistical significance [Table 3]. With increasing duration of TCS application, more patients showed characteristic dermoscopy findings. Statistical significance was, however, attained for Y-shaped vessels and brown globules with ≥3 months duration of TCS use and polygonal vessels with ≥6 months duration [Table 4].
| Characteristic | Number(%) |
|---|---|
| Age group(years) | |
| 18–30 | 66(50) |
| 31–40 | 47(35.6) |
| >40 | 19(14.4) |
| Gender | |
| Male | 24(18.2) |
| Female | 108(81.8) |
| Education | |
| Illiterate | 25(18.9) |
| Literate | 107(81.1) |
| Duration of TCS application(years) | |
| ≤1 | 63(47.7) |
| 1–10 | 63(47.7) |
| >10 | 6(4.6) |
| Source of recommendation | |
| Relatives/friends | 74(56.1) |
| Non-dermatologist doctors | 34(25.7) |
| Over the counter | 32(24.2) |
| Dermatologist | 10(7.6) |
| Practitioners of alternative systems of medicines | 6(4.6) |
| Others(Parlor, Internet) | 2(1.5) |
| Clinical findings | Number of patients(%) | Dermoscopy findings | Number of patients(%) | P-value |
|---|---|---|---|---|
| Erythema | 107(81.1) | Red diffuse areas | 122(92.4) | 0.35 |
| Telangiectasia | 63(47.7) | Vessels(Linear, serpentine, polygonal, fine, branched, Y-shaped) | 115(87.1) | 0.001 |
| Hypertrichosis | 90(68.2) | Hypertrichosis | 106(80.3) | 0.001 |
| Hyperpigmentation | 106(80.3) | Brown globules | 127(96.2) | 0.025 |
| Atrophy | 1(0.8) | White structureless areas | 114(86.4) | 0.006 |
| White hair | 15(11.4) | White hair | 82(62.1) | 0.001 |
| Scaling | 22(16.7) | Desquamation | 48(36.4) | 0.001 |
| Pustules | 4(3.0) | Pustules | 39(29.6) | 0.001 |
| Other findings | ||||
| Wrinkles | 47(35.6) | Demodex tails | 38(28.8) | |
| Hypopigmentation | 14(10.6) | Breaking of pseudoreticular network | 99(75) | |
| Follicular plugging | 17(12.9) | |||
| Comedones | 14(10.6) |
Statistically significant values are in bold.
| Dermoscopy Examination | Comparison on the basis of gender | Comparison on the basis of potency used | ||||
|---|---|---|---|---|---|---|
| Males(%) n=24 |
Females(%) n=108 |
P value | Class I and II(%) n=54 |
Class III and above (%) n=78 |
P-value | |
| Linear vessels without branches | 12(50) | 50(46.3) | 0.74 | 21(38.9) | 41(52.6) | 0.12 |
| Serpentine vessels | 15(62.5) | 82(75.9) | 0.18 | 39(72.2) | 58(74.4) | 0.79 |
| Polygonal vessels | 5(20.8) | 38(35.2) | 0.18 | 20(37.0) | 23(29.5) | 0.36 |
| Fine vessels | 3(12.5) | 2(1.8) | 0.01 | 1(1.8) | 4(5.1) | 0.33 |
| Branched vessels | 11(45.8) | 73(67.6) | 0.04 | 36(66.7) | 48(61.5) | 0.55 |
| Y-shaped vessels | 4(16.7) | 29(26.8) | 0.29 | 13(24.0) | 20(25.6) | 0.84 |
| Breaking of pseudoreticular network | 19(79.2) | 80(74.1) | 0.6 | 4176.0) | 58(74.4) | 0.84 |
| White structureless areas | 19(79.2) | 95(87.9) | 0.26 | 4787.0) | 67(85.6) | 0.85 |
| Brown globules | 23(95.8) | 104(96.3) | 0.92 | 51(94.4) | 76(97.4) | 0.38 |
| Linear brown/red wavy streaks | 6(25) | 32(29.6) | 0.65 | 15(27.8) | 23(29.5) | 0.83 |
| Red diffuse areas | 23(95.8) | 99(91.7) | 0.49 | 52(96.3) | 70(89.7) | 0.16 |
| Follicular plugging | 5(20.8) | 12(11.1) | 0.19 | 5(9.2) | 12(15.4) | 0.3 |
| Demodex tails | 8(33.3) | 30(27.8) | 0.59 | 18(33.3) | 20(25.6) | 0.34 |
| Pustules | 11(45.8) | 28(25.9) | 0.05 | 1731.4) | 22(28.2) | 0.69 |
| Comedones | 4(16.7) | 10(9.3) | 0.29 | 8(14.8) | 6(7.7) | 0.19 |
| White hair | 14(58.3) | 68(62.9) | 0.67 | 36(66.6) | 46(59.0) | 0.37 |
| Hypertrichosis | 16(66.7) | 90(83.3) | 0.06 | 42(77.8) | 64(83.3) | 0.54 |
| Desquamation | 8(33.3) | 40(37.0) | 0.73 | 20(37.0) | 28(35.9) | 0.89 |
| Others(Tinea) | 3(12.5) | 7(6.5) | 0.31 | 3(5.6) | 7(9.0) | 0.47 |
Statistically significant values are in bold.
| Dermoscopy Examination | Number of patients | P value* | Number of patients | P value* | Number of patients | P value* | |||
|---|---|---|---|---|---|---|---|---|---|
| <3 months | ≥3 months | <6 months | ≥6 months | <9 months | ≥9 months | ||||
| Linear vessels without branches | 13 | 49 | 0.84 | 23 | 39 | 0.92 | 24 | 38 | 0.89 |
| Serpentine vessels | 16 | 81 | 0.32 | 32 | 65 | 0.79 | 33 | 64 | 0.61 |
| Polygonal vessels | 5 | 38 | 0.11 | 9 | 34 | 0.04 | 11 | 32 | 0.10 |
| Fine vessels | 0 | 5 | 0.15 | 1 | 4 | 0.29 | 1 | 4 | 0.26 |
| Branched vessels | 13 | 71 | 0.22 | 27 | 57 | 0.64 | 28 | 56 | 0.50 |
| Y-shaped vessels | 1 | 32 | 0.01 | 7 | 26 | 0.08 | 9 | 24 | 0.19 |
| Breaking of pseudoreticular network | 18 | 81 | 0.65 | 32 | 67 | 0.71 | 34 | 65 | 0.67 |
| White structureless areas | 21 | 93 | 0.78 | 37 | 77 | 0.81 | 40 | 74 | 0.86 |
| Brown globules | 20 | 107 | 0.01 | 38 | 89 | 0.08 | 40 | 87 | 0.01 |
| Linear brown/red wavy streaks | 9 | 29 | 0.89 | 12 | 26 | 0.53 | 14 | 24 | 0.71 |
| Red diffuse areas | 21 | 101 | 0.41 | 39 | 83 | 0.78 | 42 | 80 | 0.82 |
| Follicular plugging | 3 | 14 | 0.51 | 6 | 11 | 0.66 | 6 | 11 | 0.57 |
| Demodex tails | 7 | 31 | 0.58 | 14 | 24 | 0.82 | 16 | 22 | 0.91 |
| Pustules | 7 | 32 | 0.54 | 14 | 25 | 0.78 | 15 | 24 | 0.791 |
| Comedones | 5 | 9 | 0.97 | 6 | 8 | 0.84 | 6 | 8 | 0.79 |
| White hair | 15 | 67 | 0.63 | 26 | 56 | 0.58 | 29 | 53 | 0.74 |
| Hypertrichosis | 20 | 86 | 0.81 | 34 | 72 | 0.69 | 36 | 70 | 0.62 |
| Desquamation | 8 | 40 | 0.43 | 14 | 34 | 0.36 | 17 | 31 | 0.65 |
| Others(Tinea) | 1 | 9 | 0.26 | 5 | 5 | 0.91 | 5 | 5 | 0.88 |
Statistically significant values are in bold.

- Erythema, telangiectasias, and hyperpigmentation along with atrophy and hypopigmentation in a 40-year-old lady after using mometasone furoate 0.1% cream for 3 months

- Clinical image showing telangiectasias, depigmentation, hypertrichosis, and comedones

- Telangiectasias, atrophy, hypertrichosis, and comedones in a 52-year-old lady with topical steroid-dependent or damaged face

- Marked skin wrinkling and white hair in a man with topical steroid-dependent or damaged face
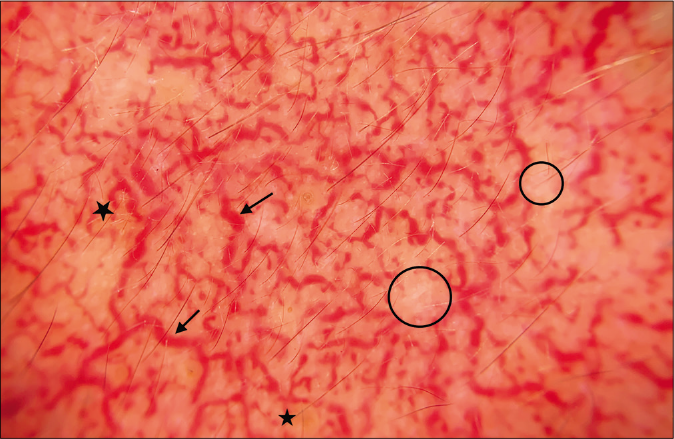
- Serpentine vessels (black arrow), brown globules (black star), white structureless areas (black circle), and breaking of pseudo-reticular network (Dermlite DL 200 hybrid, polarized mode, ×10)
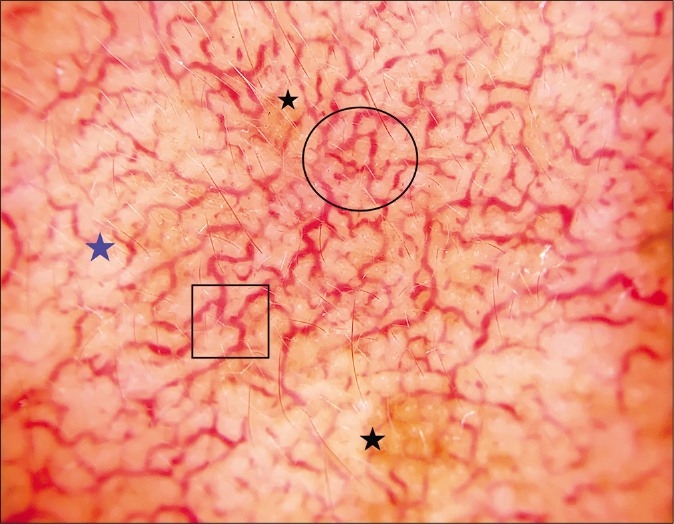
- Branched and polygonal vessels (black circle), Y-shaped vessels (black square), brown globules (black star), and white structureless areas (blue star) (Dermlite DL 200 hybrid, polarized mode, ×10)

- Demodex tails (black circle), white structureless areas (black star), serpentine vessels (black arrow), and white hair (blue arrow) (Dermlite DL 200 hybrid, polarized mode, ×10)
- Linear vessels without branches (black arrow), red diffuse areas (black star), and brown globules (blue star) (Dermlite DL 200 hybrid, polarized mode, ×10)
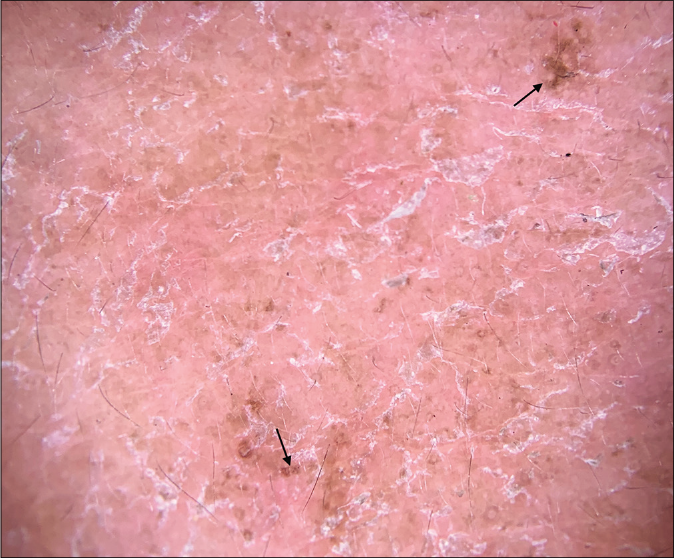
- Diffuse desquamation and brown globules (black arrow) (Dermlite DL 200 hybrid, non-polarized mode without contact fluid, ×10)

- Follicular plugging (black circle), Y-shaped vessels (black square), hypertrichosis (blue arrow), and desquamation (black arrow) (Dermlite DL 200 hybrid, polarized mode, ×10)
Discussion
TCSs are used widely for multitude of indications in dermatology. However, if abused or overused, these can result in a plethora of symptoms.3 A multicentric study in India highlighted and documented that long-term application and repeated use of TCS is rampant and also coined the term “TSDF” to signify typical traits of potent TCS application over the long haul on face such as dryness, burning, itching, and rebound erythema.7 TSDF presents as a stumbling block for the patient as well as the treating dermatologist.8 At first, patients may initiate using TCS for some minor dermatosis such as acne or melasma upon suggestion by friends and relatives.9 Ab initio, the anti-inflammatory and vasoconstrictive effects of steroids result in what appears to be clearing of primary dermatitis, but their incessant use culminates in atrophy of epidermis, degeneration of dermal structure, and collagen deterioration over several months.8 Various studies have stressed upon the diverse clinical manifestations of TSDF. Female predominance has been reported by most investigators, which was the finding in this study as well.3,5,10 The underlying reasons for this might be a higher cosmetic concern as well as societal pressure prevalent amongst females. Past studies have found the most common age group to be 18–30 years, which corroborates with the present study wherein half of the patients were in this age group.5,7,11 The vulnerability of this age group is due to attainment of marriageable age, starting of new jobs, and active participation in society and social media. Illiteracy is perceived by most as the prime reason for unsupervised application of TCS. However, 81.1% patients in the reported study were literate. A similar Indian study mirrors our findings, strengthening the belief that even educated persons can be ignorant and could get trapped in the morass of TCS use. Presenting complaints in this study ranged from redness, itching, photosensitivity to pigmentation, and acne. Mechanisms such as rebound dilatation of blood vessels, cytokine release, and nitric oxide accumulation are considered responsible for the development of pruritus, erythema, and burning sensation.5 Duration of TCS application ranged from one month to over 25 years. More than half (52.3%) of the patients used TCS for over one year. This reflects the rampant and unchecked sale of TCS as over-the-counter (OTC) products. About 56.1% patients used TCS on recommendation by relatives, friends, and neighbors whereas 25% got them prescribed by non-dermatologists. Similar trends were reported by Lu et al. from China.12 OTC availability is one of the major contributory factors in increasing steroid abuse, demanding implementation of stringent legislative measures to stop OTC sale of steroid containing creams. About 78% patients used TCS with potency three and above, consistent with other Indian studies from diverse regions.3,5,10 Many of our patients used double or triple combination creams containing an antibiotic, antifungal, and TCS. These so-called cocktail creams pose the greatest challenge due to their low cost and easy availability. Most reported indications for TCS abuse include melasma and acne. Another prevalent reason appears to be the false belief of TCS being a fairness product. Many consider TCS to be a panacea and use them for any rash on skin without consultation. This may be due to the cost-effective accessibility of creams containing such formulations. Erythema, dyspigmentation, and papulopustular lesions are the common clinical signs seen in patients with TSDF.3,5,10 We, in addition, also observed hypertrichosis (68.2%) in a high percentage of patients.
Dermoscopy has emerged as an excellent tool to evaluate the subtle changes in skin and can be especially useful in patients of TSDF. It can help in identifying various findings suggestive of TCS abuse that cannot be appreciated with naked eye examination. Studies on dermoscopy in TSDF are scarce, with most being anecdotal case reports. Dermoscopy may aid in early identification of features suggestive of TSDF before their clinical appearance. In the present study, significantly higher number of patients dermoscopically revealed white structureless areas (P = 0.006), vessels (P = 0.001), desquamation (P = 0.001), white hair (P = 0.001), and hypertrichosis (P = 0.001). These features become clinically evident after months of TCS use and if identified early can be reversible. In a previous study on 40 patients by Tatu, dermoscopy findings seen were polygonal vessels (100%), red diffuse areas (100%), demodex tails (80%), and pustules (80%). Atrophy was clinically visible in four patients, but dermoscopy revealed another four patients with white structureless areas.6
The most common dermoscopy findings seen in our patients were brown globules (96.2%), red diffuse areas (92.4%), vessels (87.1%), white structureless areas (86.4%), hypertrichosis (80.3%), and white hairs (62.1%). Sonthalia et al. in a 29-year-old man with TSDF reported reddish-brown background, brown dots, globules and clods, ivory-white-to-strawberry ice cream-colored patches, multiple serpentine, and branching linear vessels without branches with hypertrichosis.13 Jakhar and Kaur also appreciated irregularly dilated, branched serpentine vessels, almost interconnecting, giving a polygonal pattern along with white structureless areas and hypertrichosis in a young female.14 Appearance of fine vessels (P = 0.01) and pustules (P = 0.05) were significantly associated with male gender, and branched vessels (P = 0.04) with female gender. Androgens in males stimulate sebaceous gland proliferation, especially over face, chest, and upper back. Production of sebum is significantly higher among males, mainly influenced by androgens which can dilute the TCS effect, whereas estrogens exert opposing effect through down-regulation of sebaceous gland function.15 According to Bailey et al., men have an overall 10–20% thicker skin than women which could be the reason for increased tortuosity and arborization of vessels in females.16 The potency of TCS used did not appear to alter the dermoscopic findings. This further needs to be correlated with the duration of TCS used for better interpretation. Y-shaped vessels and brown globules were seen in a significantly higher number of patients using TCS for more than three months and in those continuing it beyond six months, polygonal vessels were predominant. With increasing duration of TCS application, most dermoscopy findings, including white structureless area, brown globules, white hair, and hypertrichosis show progression. Thus, by visualizing these findings, we can assess even the approximate duration of application of TCS by the patient if the history is not forthcoming, thus helping in predicting treatment response and prognosis. All patients presenting with facial redness, itching, dermatitis must be examined using a dermoscope to identify these easily recognizable features and to differentiate TSDF from other causes of red face, including tinea faciei, contact dermatitis, and lupus erythematosus. Follicular micropustules, diffuse intense erythema (not as regular dots), and brown spots with white-yellowish halo have been described in superficial fungal infections.17 Dotted vessels, yellow scales, and sero-crusts are evident in contact dermatitis and inverse strawberry pattern with salmon-colored follicular dots surrounded by white halos in malar rash of lupus.18,19 Older term of “steroid dermatitis resembling rosacea” suggests that TSDF can mimic rosacea with or without demodecidosis, especially in the absence of a supportive history of TCS application. However, the absence of hypertrichosis, white hair, and atrophy favors TSDF over rosacea. Dermoscopy not only non-invasively confirms the suspicion but also aids in patient’s understanding of the seriousness of topical steroid abuse through the demonstration of pictures explained in patient-friendly language. This also can prevent further steroid abuse and improves treatment compliance.
Lack of histopathological correlation is the limitation of our study. Brown globules seen in 96.2% patients of TSDF on dermoscopy may not always signify TSDF; instead, it could represent underlying melasma for which the patient applied TCS. Thus, dermoscopy in TSDF can help in a multitude of ways, from confirming the diagnosis to differentiating from other causes of red face and predicting the approximate duration of TCS abuse. Further, it can also help in predicting disease severity and prognosis. An additional advantage could be in counseling the patients and monitoring response to treatment. With effective treatment, a decrease in vessels, scaling, hypertrichosis, white hair, and red diffuse areas is expected; however, future research supporting the same is warranted.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Topical steroid damaged/dependent face (TSDF): An entity of cutaneous pharmacodependence. Indian J Dermatol. 2016;61:265-72.
- [CrossRef] [PubMed] [Google Scholar]
- Topical corticosteroids: Mechanisms of action. Acta Derm Venereol Suppl (Stockh). 1989;151:7-10. discussion 47-52
- [Google Scholar]
- Study of clinical profile of patients presenting with topical steroid-induced facial dermatosis to a tertiary care hospital. Indian Dermatol Online J. 2020;11:208-11.
- [Google Scholar]
- Topical corticosteroid misuse: The Indian scenario. Indian J Dermatol. 2014;59:451-5.
- [CrossRef] [PubMed] [Google Scholar]
- Steroid dermatitis resembling rosacea: A clinical evaluation of 75 patients. ISRN Dermatol. 2013;2013:491376.
- [CrossRef] [PubMed] [Google Scholar]
- Topical steroid induced facial rosaceiform dermatitis. Acta Endocrinol (Buchar). 2016;12:232-3.
- [CrossRef] [PubMed] [Google Scholar]
- Topical corticosteroid abuse on the face: A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160-6.
- [CrossRef] [PubMed] [Google Scholar]
- Topical steroid-dependent face: Response to xylometazoline topical. Indian J Drugs Dermatol. 2017;3:87-9.
- [CrossRef] [Google Scholar]
- Misuse of topical corticosteroids: A clinical study of adverse effects. Indian Dermatol Online J. 2014;5:436-40.
- [CrossRef] [PubMed] [Google Scholar]
- Topical corticosteroids: Abuse and Misuse. Our Dermatol Online. 2015;6:130-4.
- [CrossRef] [Google Scholar]
- Facial corticosteroid addictive dermatitis in Guiyang City, China. Clin Exp Dermatol. 2010;35:618-21.
- [CrossRef] [PubMed] [Google Scholar]
- The role of dermoscopy in a topical steroid-damaged face. Dermatol Pract Concept. 2018;8:166-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of topical steroid damaged/dependent face. Indian Dermatol Online J. 2018;9:286-7.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of male and female sebum production. Egypt J Hosp Med. 2017;69:1847-79.
- [CrossRef] [Google Scholar]
- The use of non-invasive instruments in characterizing human facial and abdominal skin. Lasers Surg Med. 2012;44:131-42.
- [CrossRef] [PubMed] [Google Scholar]
- Can dermoscopy serve as a diagnostic tool in dermatophytosis? A pilot study. Indian Dermatol Online J. 2019;10:530-5.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of inflammatory dermatoses (inflammoscopy): An up-to-date overview. Dermatol Pract Concept. 2019;9:169-80.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of discoid lupus erythematosus. Br J Dermatol. 2013;168:284-8.
- [CrossRef] [PubMed] [Google Scholar]






