Translate this page into:
Different aspects and variants of mycosis fungoides in a single patient
Corresponding author: Dr. Bruno Castro Souza, Hospital das Clínicas, Medical School of the University of São Paulo, São Paulo, Brazil. brunocastro1990@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Souza BC, Miyashiro D, Giannoti MA, Sanches JA. Different aspects and variants of mycosis fungoides in a single patient. Indian J Dermatol Venereol Leprol 2021;87:565-8.
Sir,
The WHO-EORTC classification includes only three clinico-pathological variants of mycosis fungoides: folliculotropic mycosis fungoides, granulomatous slack skin and pagetoid reticulosis.1 However, other forms of mycosis fungoides are commonly seen.2 Here we report a patient with a mixture of classical patches, folliculotropic, syringotropic and granulomatous lesions.
A 29-year-old male patient presented to our outpatient clinic with a history of pruritic cutaneous lesions for nine years. The lesions started over the trunk and later spread and the patient denied any previous treatment. Dermatological examination revealed erythematous scaly patches affecting the axillae, trunk, buttocks, legs, cubital and popliteal fossae. Palms and fingers showed diffuse erythema with dryness, edema and infiltration. There was an area of non-scarring alopecia in the left parietal region and of pubic and axillary hair were absent. Erythemato violaceous hardened infiltrated plaques were seen over the inguinal regions and right calf [Figure 1]. No lymph node enlargement or organomegaly was clinically detected. A diagnosis of mycosis fungoides was made with typical patches and features of syringotropic, folliculotropic and granulomatous mycosis fungoides. Histological and immunohistochemistry analysis of scalp, left palm, inguinal region and left calf were performed.

- a Area of non-scarring alopecia in the left parietal region
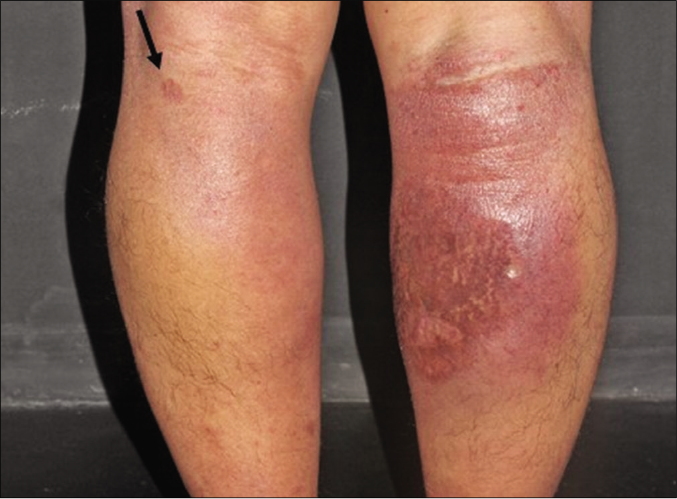
- The left leg with patches and the right calf with an infiltrated plaque with an erythematoviolaceous surface

- Hardened infiltrated plaque with an erythematoviolaceous surface in inguinal region. Observe the absence of pubic hair.
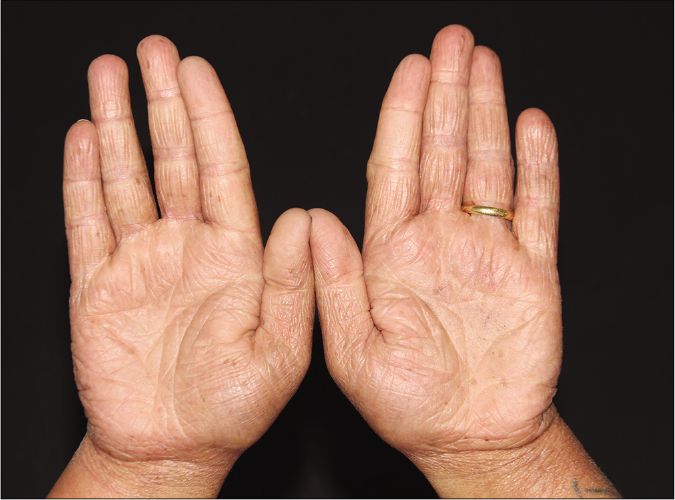
- Hands with diffuse erythema and infiltration
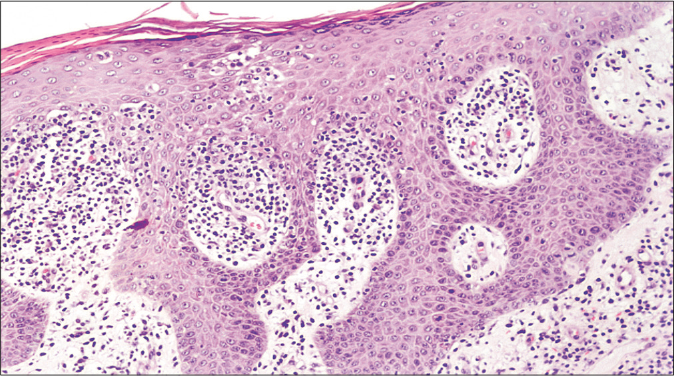
All specimens showed epidermal infiltration with small and medium-sized atypical lymphocytes. Folliculotropism of atypical lymphocytes with no mucin deposition was observed in the scalp (Alcian blue negative) and syringotropism was seen in the palmar region [Figures 2a and b]. In the left leg, there was epidermotropism with Pautrier microabscess [Figure 2c]. In the left inguinal lesion, besides the mycosis fungoides features, there were giant cells forming granulomas extending from the reticular to the deep dermis [Figure 2d].
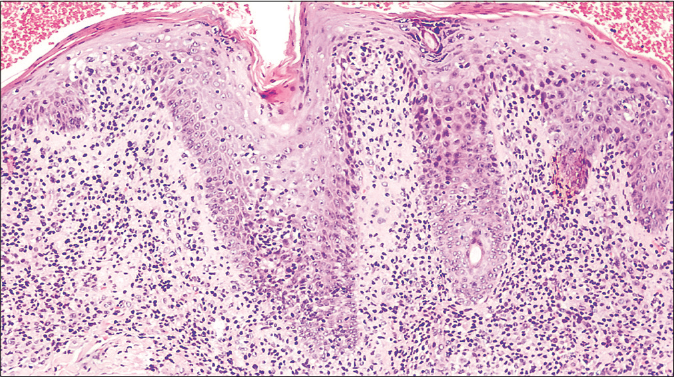
- Histological findings of the parietal biopsy revealed infiltration of the follicular epithelium by small, medium-sized lymphocytes. Mucinous degeneration was not seen (hematoxylin and eosin 100×)
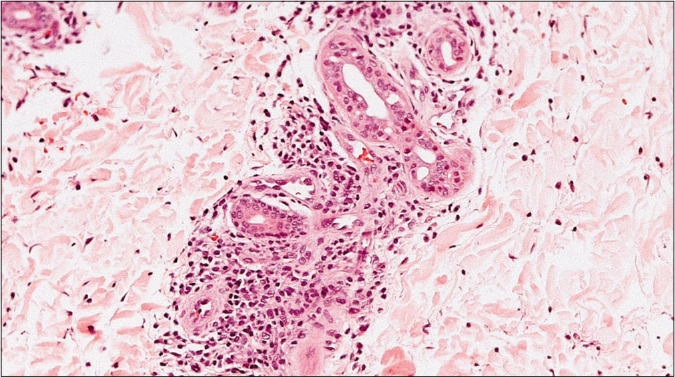
- Biopsy of the palm revealed small collections of medium and large size atypical lymphocytes within the acrosyringium (hematoxylin and eosin 200×)
- Biopsy of the leg revealed epidermotropism of small and medium size lymphocytes (hematoxylin and eosin 100×)
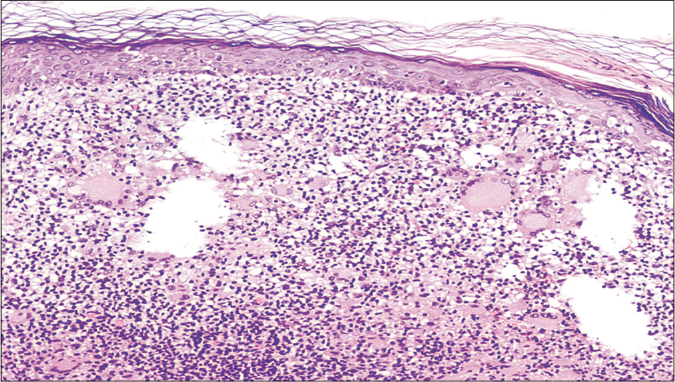
- Skin biopsy from inguinal region with superficial atypical lymphocyte infiltrate, granulomas and multinucleated giant cells (hematoxylin and eosin 100×)
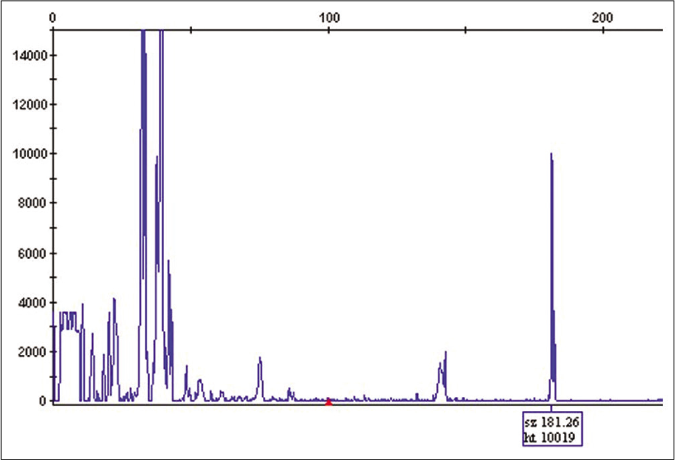
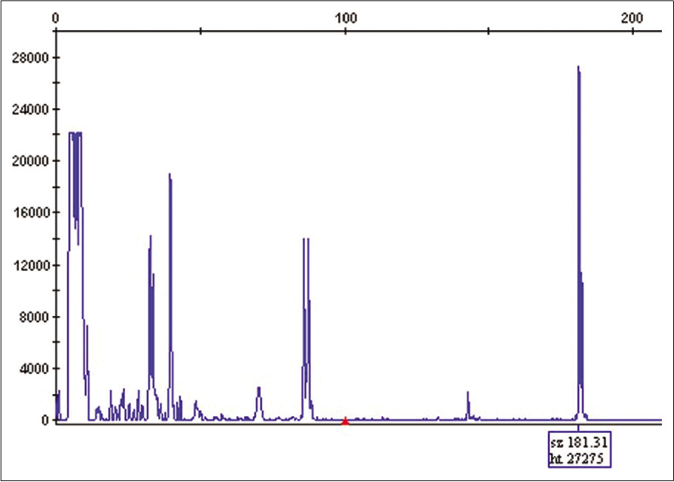
Immunohistochemistry of all specimens was similar. There was a predominance of CD4+ lymphocytes with a CD4/CD8 ratio of 9:1. Loss of CD7 was present in more than 90% of CD4+ lymphocytes. T-cell receptor gene rearrangement by polymerase chain reaction identified the same clonal T-cell population in the parietal scalp, inguinal and leg samples [Figure 3]. We made a diagnosis of mixed classic, folliculotropic, syringotropic and granulomatous mycosis fungoides.
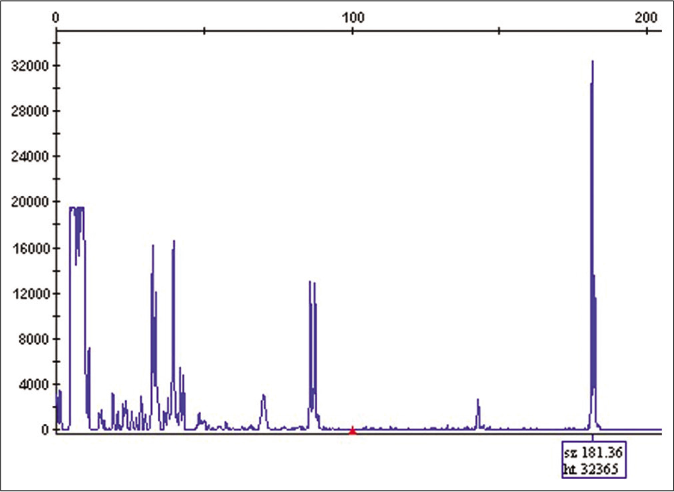
- T-cell receptor gene rearrangement by PCR identified the same clonal T-cell population in parietal region samples
- T-cell receptor gene rearrangement by PCR identified the same clonal T-cell population in inguinal samples
- T-cell receptor gene rearrangement by PCR identified the same clonal T-cell population in leg samples
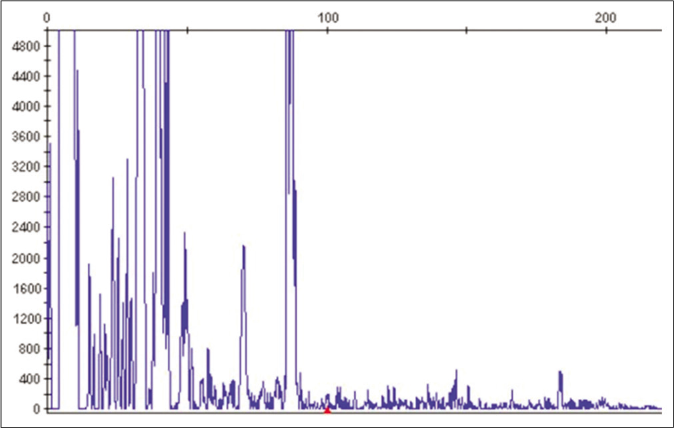
- No clonal population of T cells were identified in blood sample
Complete blood count, peripheral blood immunophenotyping by flow cytometry, manual Sézary cell count and blood chemistry panel were normal, including serum calcium and lactate dehydrogenase. Computed tomography showed no lymphadenopathy or organomegaly. Alpha-interferon three million IU and PUVA three times a week were initiated. After seven months of treatment, partial response with reduction in cutaneous infiltration over axillae, trunk, cubital and popliteal fossae, and inguinal regions was observed. Furthermore, the punctate erythema on the palms improved. Scalp, pubic and axillary hair loss persisted. The patient was followed up with clinical evaluation and there was no sign of systemic dissemination.
In addition to the three variants included in the WHOEORTC classification of cutaneous lymphomas, other clinicopathologic subtypes are described.2 Typically, these subtypes are divided clinical (distinctive clinical, but same histopathology as of classic mycosis fungoides), clinicopathologic (distinctive clinical and histopathology) and histopathologic ones (distinctive histopathology, but same clinical presentation as classic mycosis fungoides).2 We have observed in our clinical practice that some patients present with more than one form concomitantly. However, the association of multiple peculiar forms of mycosis fungoides is rarely described in the literature.3
Our patient presented typical clinical lesions of classic, folliculotropic, syringotropic and granulomatous mycosis fungoides. Histopathology confirmed these suspicions. It is the first report of these associations in a single patient to the best of our knowledge.
Syringotropism is not commonly reported in histopathological specimens of mycosis fungoides. There is a controversy if syringotropic mycosis fungoides is a variant of folliculotropic mycosis fungoides or a distinct entity.4 De Masson et al. showed that, while in folliculotropic mycosis fungoides, the head and neck are commonly affected, in syringotropic form, nearly half of the patients present with punctate palmoplantar lesions. Furthermore, clinical course of syringotropic mycosis fungoides seems to be more indolent with better overall and disease-free survival.5
Many authors consider granulomatous mycosis fungoides as a histopathological variant. In our opinion, however, the sarcoidal aspect of the cutaneous lesions could suggest this diagnosis even clinically. Therefore, it would be classified as a clinicopathological subtype. In granulomatous mycosis fungoides, biopsy shows scarce epidermotropism, atypical lymphocytic dermal infiltrate and multinucleated giant histiocytes producing ill-defined granulomas that may extend to the reticular dermis.3 The absence of elastolysis and elastophagocytosis helps to differentiate granulomatous mycosis fungoides from granulomatous slack skin.3 Clinically, granulomatous mycosis fungoides differs from granulomatous slack skin by the absence of pendulous lax skin folds in the former.
We draw attention to the fact that some patients present different clinical-pathological forms of mycosis fungoides. Are they distinct entities or a spectrum of the same disease? In this patient, identical T-cell clones in all specimens reinforce the hypothesis that they are part of the same spectrum.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The 2018 update of the WHO-EORTCclassification for primary cutaneous lymphomas. Blood. 2019;133:1703-14.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathologic variants of mycosis fungoides. Actas Dermosifiliogr. 2017;108:192-208.
- [CrossRef] [PubMed] [Google Scholar]
- Coexistence of various clinical and histopathological features of mycosis fungoides in a young female. Indian J Dermatol. 2015;60:214.
- [Google Scholar]
- The histological prevalence and clinical implications of folliculotropism and syringotropism in mycosis fungoides. Chin Clin Oncol. 2019;8:6.
- [CrossRef] [PubMed] [Google Scholar]
- Syringotropic mycosis fungoides: clinical and histologic features, response to treatment, and outcome in 19 patients. J Am Acad Dermatol. 2014;71:926-34.
- [CrossRef] [PubMed] [Google Scholar]





