Translate this page into:
Disseminated molluscum contagiosum in a patient on methotrexate therapy for psoriasis
2 Department of Pathology, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India
Correspondence Address:
Vineet Relhan
35-F, Sector-7, SFS Flats, Jasola Vihar, New Delhi -110 025
India
| How to cite this article: Bansal S, Relhan V, Roy E, Garg VK, Khurana N. Disseminated molluscum contagiosum in a patient on methotrexate therapy for psoriasis. Indian J Dermatol Venereol Leprol 2014;80:179-180 |
Sir,
Molluscum contagiosum is commonly a self-limiting condition occurring in children, but widespread infection can be encountered occasionally in patients with impaired cellular immunity. We report a case of a 70-year-old man with chronic plaque psoriasis on methotrexate therapy who developed disseminated molluscum contagiosum in resolving plaques of psoriasis. The lesions resolved on stopping methotrexate.
A 70-year-old male having plaque psoriasis for the past 30 years, presented with an asymptomatic papular eruption in healing plaques of psoriasis over the trunk, upper limbs and buttocks for the last 6 months. The patient had received many topical therapies in the past and was receiving methotrexate 22.5 mg weekly for the previous 8 months. Physical examination revealed smooth, discrete, asymptomatic, yellowish papules 2-5 mm in diameter over trunk, limbs, and buttocks [Figure - 1], some of which showed central umblication. Plaques of psoriasis were present over the scalp, trunk, and upper limbs. We considered the differential diagnoses of disseminated molluscum contagiosum, milia, granuloma annulare, and sarcoidosis. Cellular material expressed from the center of umblicated papules crushed between two slides and stained with Giemsa stain showed intracytoplasmic molluscum inclusion bodies. Punch biopsy of a papule on the trunk revealed a focal endophytic growth consisting of hyperplastic keratinocytes containing eosinophilic intracytoplasmic inclusions suggestive of molluscum contagiosum [Figure - 2]. Routine hematological investigations were normal. An antibody assay for human immunodeficiency virus (HIV) done by enzyme-linked immunosorbent assay (ELISA) was nonreactive and CD4 counts were 960 cells/mm 3 .
 |
| Figure 1: Disseminated discrete skin-coloured to yellow papules along with healing plaques of psoriasis on patient's thighs |
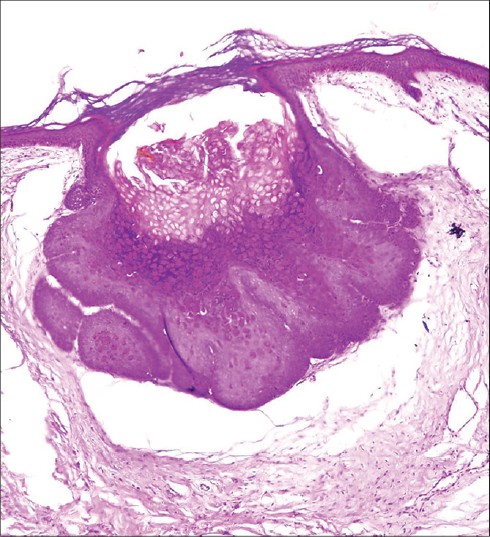 |
| Figure 2: Histopathology of a papule revealing a focal endophytic growth of keratinocytes containing eosinophilic intracytoplasmic inclusions (H and E, original magnifi cation 40) |
A diagnosis of disseminated molluscum contagiosum was made, methotrexate was stopped, and the patient was prescribed emollients. The mollusca gradually resolved over a period of 6 months without any other intervention.
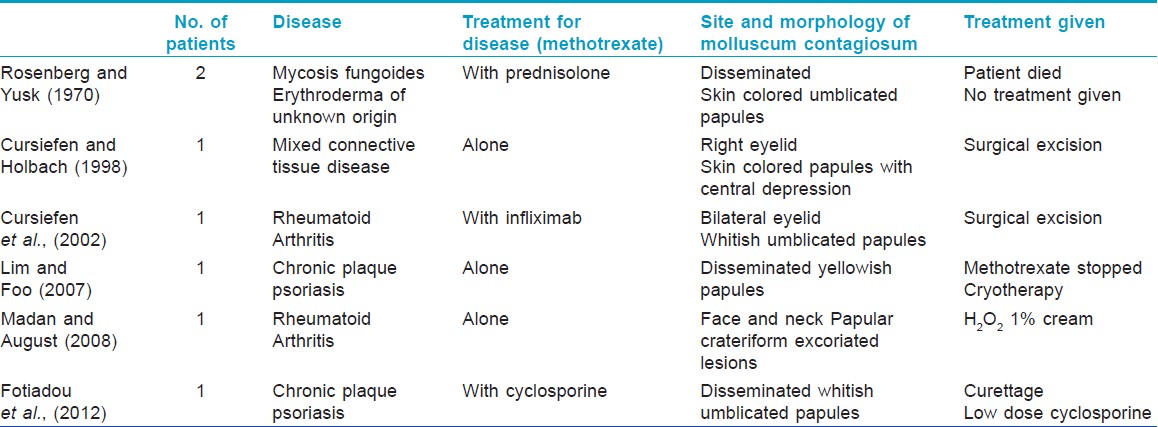
Molluscum contagiosum is a skin infection caused by the molluscum contagiosum virus of the Poxviridae family, which is transmitted by direct contact. There are some previous reports of widespread molluscum contagiosum infection in patients treated with methotrexate; either alone or in combination with other immunosuppressive agents, though we could find none from India [Table - 1]. [1],[2],[3],[4],[5],[6] The reported cases had either disseminated lesions or atypical morphology. Methotrexate inhibits deoxyribonucleic acid synthesis by binding to dihydrofolate reductase in immunologically competent cells, and suppresses serum levels of inflammatory cytokines like tumor necrosis factor (TNF) α production through the release of adenosine, and suppressing TNF α-induced nuclear factor κB activation. It also inhibits production of interferon-γ by T-cell receptor-primed T lymphocytes. [7] Suppressed activity or decreased production of TNF α and INF-ϒ by methotrexate may explain the susceptibility to molluscum contagiosum infection despite normal CD4 counts. In our patient, withdrawal of methotrexate led to clearance of mollusca in 6 months favoring a strong association of the drug with the development of disseminated infection.
Treatment options for disseminated molluscum contagiosum developing with immunosuppressive therapy include discontinuing the immunosuppressive therapy followed by manual extraction, chemical cauterization, or cryotherapy.
| 1. |
Rosenberg EW, Yusk JW. Molluscum contagiosum. Eruption following treatment with prednosolone and methotrexate. Arch Dermatol 1970;101:439-41.
[Google Scholar]
|
| 2. |
Cursiefen C, Holbach LM. Molluscum contagiosum in immunosuppression with methotrexate: multiple warts with central depressions of the eyelids. Klin Monbl Augenheilkd 1998;212:123-4.
[Google Scholar]
|
| 3. |
Cursiefen C, Grunke M, Dechant C, Antoni C, Jünemann A, Holbach LM. Multiple bilateral eyelid molluscum contagiosum lesions associated with TNF alpha-antibody and methotrexate therapy. Am J Ophthalmol 2002;134:270-1.
[Google Scholar]
|
| 4. |
Lim KS, Foo CC. Disseminated molluscum contagiosum in a patient with chronic plaque psoriasis taking methotrexate. Clin Exp Dermatol 2007;32:591-3.
[Google Scholar]
|
| 5. |
Madan V, August PJ. Facial molluscum contagiosum in a patient with rheumatoid arthritis taking methotrexate. Clin Exp Dermatol 2008;33:347.
[Google Scholar]
|
| 6. |
Fotiadou C, Lazaridou E, Lekkas D, Kourouklidou A, Demetrios I. Disseminated, eruptive molluscum contagiosum lesions in a psoriasis patient under treatment with methotrexate and cyclosporine. Eur J Dermatol 2012;22:147-8.
[Google Scholar]
|
| 7. |
Chan ES, Cronstein BN. Molecular action of methotrexate in inflammatory diseases. Arthritis Res 2002;4:266-73
[Google Scholar]
|
Fulltext Views
3,810
PDF downloads
2,159





