Translate this page into:
Docetaxel induced pellagroid dematitis
Correspondence Address:
Preema Sinha
Department of Dermatology, Armed Forces Medical College, Pune - 411 040, Maharashtra
India
| How to cite this article: Sinha P, Sood A, Baveja S, Pathania V. Docetaxel induced pellagroid dematitis. Indian J Dermatol Venereol Leprol 2018;84:723-725 |
Sir,
Varied presentations of docetaxel-induced cutaneous side-effects include maculopapular drug rash, hand-foot syndrome, plaque-like erythrodysesthesia, erythema multiforme, nail changes, scleroderma, supravenous discoloration, radiation recall dermatitis, desquamation, flagellate erythema, photolichenoid reactions and even life-threatening toxic epidermal necrolysis.[1],[2] Pellagra-like lesions caused by docetaxel have been reported only once in the literature. Here, we describe this rare side-effect.
A 47-year-old lady a known case of invasive lobular carcinoma of the left breast on regular chemotherapy presented with complaints of red, raised, itchy, dark-colored lesions over her face, neck, forearms, hands and feet ten days after receiving the first injection of docetaxel. Earlier she was receiving paclitaxel which was stopped after seven cycles on suspicion of grade 3 paraesthesias due to paclitaxel. She gave a history of burning sensation at the site of the lesions on sun exposure. Itching was moderate but did not interfere with her sleep and daily activities. There was no history of fever, loose motions, pain abdomen or affection of mental faculties. She denied any exposure to chemical agents and contact allergens and home remedies.
General and systemic examination was normal. Dermatological examination revealed presence of erythematous to hyperpigmented, scaly plaques with areas of erosions and fissuring with minimal oozing of clear watery fluid over the face, nape of neck, sides and 'V' of neck, dorsa of hands and feet, both forearms and legs with sharp demarcation at midhalf [Figure - 1] and [Figure - 2]. Nails showed black discoloration with lack of lustre. Examination of oral mucosa and palms and soles was normal. Scalp had chemotherapy-induced alopecia totalis.
 |
| Figure 1: Involvement of face, nape of neck, sides and ‘V’ of neck, in the form of erythematous to hyperpigmented, scaly plaques |
 |
| Figure 2: Hyperpigmented scaly oozy plaques over dorsa of hands and feet, both forearms and legs with sharp demarcation at midhalf |
Histopathological examination of the affected skin showed thinned-out epidermis with necrotic keratinocytes and spongiosis. Superficial dermis showed marked edema with sparse lymphomononuclear inflammatory infiltrate. Scattered histiocytes and melanin pigment were seen [Figure - 3].
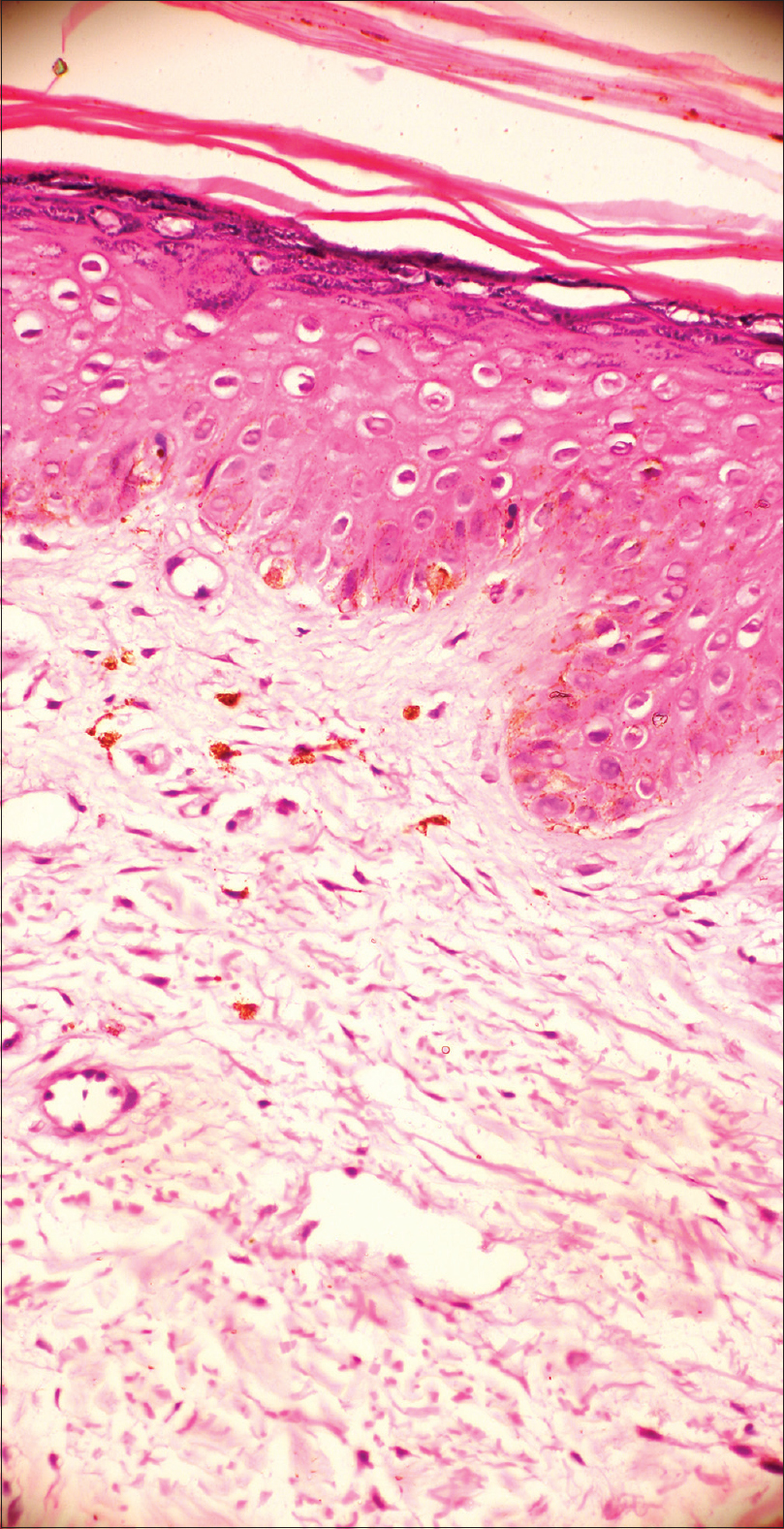 |
| Figure 3: Histopathological examination shows thinned out epidermis with necrotic keratinocytes and spongiosis. Superficial dermis shows marked oedema with pigment incontinence (H and E, ×400) |
Based on history, physical examination and histopathological examination, a diagnosis of drug-induced, pellagra-like dermatitis was made. Patient was started on tablet nicotinamide 300 mg per day in three divided doses with multivitamin B complex, and her oncologist was asked to discontinue docetaxel. Her lesions healed completely within two weeks of nicotinamide therapy [Figure - 4]. Proper nutrition with high protein diet and a physical sunscreen cream were also added to her treatment protocol.
 |
| Figure 4: Complete regression of lesions over face and neck after two weeks of treatment |
Pellagra was first described by Don Gaspar Casal in 1735 and named by Frapolli in 1771.[3] It was earlier associated with poverty, under nutrition and was mainly seen in populations subsisting on maize diet. With the introduction of niacin-fortified foods, food-related endemic pellagra has become rare.
Niacin and nicotinamide are precursors of nicotinamide adenine dinucleotide (NAD) and NAD phosphate (NADP), which are important coenzymes in the metabolism of carbohydrate, protein and fatty acid. Deficiency of NAD and NADP can lead to pellagra, resulting in a classical triad of dermatitis, diarrhea and dementia.[3]
Pellagra is now mostly associated with chronic alcohol consumption or can be drug induced.
Drug-induced pellagra can be caused by drugs such as antitubercular drugs, 5-fluorouracil, 6-mercaptopurine, phenytoin, chloramphenicol, azathioprine and phenobarbital. Isoniazid, pyrazinamide and ethionamide are structurally similar with NAD and competitively replace NAD from the metabolic pathways. Hence, tissues with high energy requirements, such as the brain, or with high turnover rate, such as the skin and gut, are affected in pellagra.[4] Moreover, these drugs are also hepatotoxic which further add to the decreased utilization of absorbed niacin and tryptophan.[5]
Inhibition of conversion of tryptophan to niacin by 5-fluorouracil leads to pellagra, and 6-mercaptopurine causes pellagra-like dermatitis by inhibiting Korenberg's enzyme (NAD phosphorylase).[5],[6] Other drugs such as phenytoin, chloramphenicol, azathioprine and phenobarbital interfere in the tryptophan-niacin pathway and lead to pellagroid dermatitis. The exquisite photosensitivity seen in pellagra may result from a cutaneous deficiency of urocanic acid, accumulation of kynurenic acid, deficiency of NAD and NADP and altered porphyrin metabolism that may induce a phototoxic reaction.[7]
However, the exact mechanism leading to pellagra-like skin lesions due to docetaxel is still not known. Akay et al. felt that the cause of photosensitive dermatitis due to docetaxel was due to a mild form of chemical porphyria affecting the porphyrin biosynthesis, but the exact mechanism still remains elusive.[8]
The cutaneous rash of pellagra is typically bilateral, well-defined, symmetrical and limited to exposed sites of sun exposure, most prominent on the dorsum of hands, “V” of the neck, face, radial aspects of the forearms and exposed skin on legs and feet. Persistent erythema and scaling are sequelae of the acute eruption. Chronic lesions show marked hyperpigmentation, skin thickening, dryness and roughness. Various signs described in association with pellagra are the “glove” or “gauntlet,” the “boots” and the “Casal's necklace.”[5],[6] All these features associated with pellagra were found in our patient.
Diagnosis of pellagra is based on the typical clinical presentation and rapid response to niacin supplementation. The primary management is replacement of nicotinamide, with the initial dose of 100 mg orally every 6 hours, tapering to 50 mg every 8–12 hours until resolution of all symptoms. Parenteral nicotinamide administration of 1 g, 3–4 times daily, is recommended for severe cases. Supplementation of other B vitamins, zinc, magnesium, as well as a diet rich in niacin, calories and protein is also recommended.
Nicotinamide is preferred over niacin in the treatment of pellagra because it does not cause vasomotor disturbances such as flushing, itching or burning.
Only one similar case of pellagra related to docetaxel has been reported by Yokomizo et al., hence, due to paucity of such reports we report this rare entity.[9]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hui YF, Giles FJ, Cortes JE. Chemotherapy-induced palmar-plantar erythrodysesthesia syndrome – Recall following different chemotherapy agents. Invest New Drugs 2002;20:49-53.
[Google Scholar]
|
| 2. |
Chew L, Chuen VS. Cutaneous reaction associated with weekly docetaxel administration. J Oncol Pharm Pract 2009;15:29-34.
[Google Scholar]
|
| 3. |
Hegyi J, Schwartz RA, Hegyi V. Pellagra: Dermatitis, dementia, and diarrhea. Int J Dermatol 2004;43:1-5.
[Google Scholar]
|
| 4. |
Sweetman SC, editor. Nutritional agents and vitamins. In: Martindale the Complete Drug Reference. 36th ed. London: RPS Publishing; 2009. p. 1957-9.
[Google Scholar]
|
| 5. |
Karthikeyan K, Thappa DM. Pellagra and skin. Int J Dermatol 2002;41:476-81.
[Google Scholar]
|
| 6. |
Hendricks WM. Pellagra and pellagralike dermatoses: Etiology, differential diagnosis, dermatopathology, and treatment. Semin Dermatol 1991;10:282-92.
[Google Scholar]
|
| 7. |
Gillman J, Gillman T, Brenner S. Porphyrin fluorescence in the livers of pellagrins in relation to ultra-violet light. Nature 1945;156:689.
[Google Scholar]
|
| 8. |
Akay BN, Unlu E, Buyukcelik A, Akyol A. Photosensitive rash in association with porphyrin biosynthesis possibly induced by docetaxel and trastuzumab therapy in a patient with metastatic breast carcinoma. Jpn J Clin Oncol 2010;40:989-91.
[Google Scholar]
|
| 9. |
Yokomizo Y, Fujikawa A, Tajiri T, Ota J, Yumura Y, Moriyama M, et al. Two cases of pellagra associated with chemotherapy of docetaxel, estramustine, dexamethasone. Hinyokika Kiyo 2010;56:585-8.
[Google Scholar]
|
Fulltext Views
4,681
PDF downloads
1,362





