Translate this page into:
Does contact allergy to benzocaine cause orodynia?
Correspondence Address:
Dipankar De
Department of Dermatology, Venereology, and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh - 160 012
India
| How to cite this article: A, De D, Handa S. Does contact allergy to benzocaine cause orodynia?. Indian J Dermatol Venereol Leprol 2015;81:84-86 |
Sir,
Contact dermatitis to topical anesthetics is a well-known entity and manifests as a wide spectrum of irritant and allergic reactions. Herein, we report two cases with unusual presentations of contact allergy to benzocaine, a commonly prescribed anesthetic gel for relief from pain in various mucosal conditions.
A 52-year-old lady presented with a highly pruritic erythematous rash on her lips and perioral area, with predominant involvement of the angles of mouth since 2 weeks. She also had similar lesions on her right index finger and the lateral aspect of her right middle finger since 1 week. She had extreme burning and stinging in her oral cavity, in spite of regular application of benzocaine 20% gel and triamcinolone acetonide 0.1% paste for oral lichen planus. Her past records revealed drug allergies to sulphasalazine
and dapsone with which she had developed acute generalized exanthematous pustulosis and generalized maculopapular rash, respectively around 1 year back. She denied any other drug intake known to cause orodynia such as angiotensin-converting enzyme inhibitors, anticoagulants, antipsychotics, antidepressants or anti-retroviral drugs. The patient was otherwise well and in good mental health. On examination, multiple erythematous papules coalescing to form ill-defined plaques were present on the lips, perioral area and right index and middle fingers. Desquamation occurred particularly over lips, angles of mouth and web space of the second finger [[Figure - 1]a]. On the contrary, oral mucosa was relatively normal with no clinical signs of inflammation except subsiding lesions of oral lichen planus [[Figure - 1]b]. An eczematous eruption temporally correlating with the application of medicaments suggested a diagnosis of contact dermatitis to the local application(s). To confirm our suspicion, we performed patch tests with Indian Standard Series (ISS) and corticosteroid series (both from Chemotechnique Diagnostics R ), using aluminium chambers premounted on hypo-allergenic adhesive tape. Readings were taken at 48 and 96 hours by the same clinician according to the International Contact Dermatitis Research Group grading. Benzocaine showed 1+ reaction at 48 hours and 2+ at 96 hours, and was of current relevance. She did not develop a positive reaction to triamcinolone acetonide, even when read at day 7. She developed 2+ reaction to paraphenylene diamine (PPD) and nickel, at 96 hours [[Figure - 2]a]. The former was found to be of past relevance as she revealed history of hand eczema few years back, when she used to apply hair dye to her friends and neighbors. This probably also signifies cross-reaction between benzocaine and PPD. She had gradual improvement in both her cutaneous lesions and orodynia after discontinuation of benzocaine gel [[Figure - 2]b and c]. Topical corticosteroids and antihistamines were required for a short period for control of symptoms that were due to application of benzocaine.
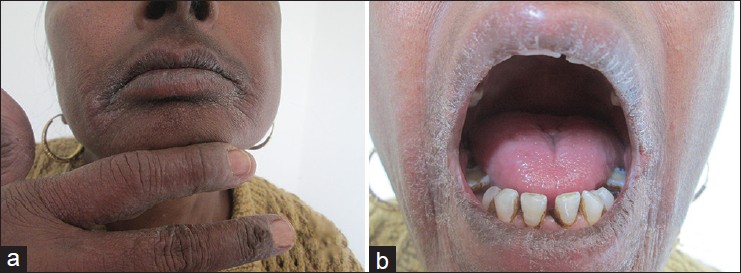 |
| Figure 1: (a) Erythematous rash on lips, angles of mouth and perioral area with similar involvement of right index finger and lateral aspect of right middle finger; (b) oral mucosa showing no evidence of erythema or erosions |
 |
| Figure 2: (a) Patch test reading in first patient at 96 hours: 2+ reaction to benzocaine, PPD and nickel in ISS; (b and c) post treatment photographs of same patient. Note the clearing of erythematous rash and desquamation from lips and perioral area |
The other patient, a 58-year-old lady in good health, had extreme burning and stinging in her oral mucosa since 1 month, in spite of regular application of anesthetic gel (benzocaine 20%) and steroid paste (triamcinolone acetonide 0.1%) for oral lichen planus. Oral mucosal examination was normal in this case also with no evidence of erythema, erosions or reticulate lesions of lichen planus, which had been observed a month back, just prior to initiation of treatment. A past history of allergy to sulpha drugs was recorded. Patch test showed 1+ reaction to benzocaine and balsam of Peru at 96 hours [Figure - 3], the former being most probably of current relevance. Positive reaction to balsam of Peru could also indicate sensitivity to toothpaste or other oral toiletries which may contain it. However, she was not using any oral toiletry except toothpaste and she was using a particular toothpaste for a long period of time. Triamcinolone acetonide did not elicit any positive reaction, even when read at day 7. The patient improved after discontinuation of benzocaine gel while she continued to use the same toothpaste which suggests benzocaine contact allergy causing orodynia. For control of symptoms, she was prescribed oral pregabalin 75 mg/day, with which she had gradual relief over a short period of time.
 |
| Figure 3: Patch test reading in second patient at 96 hours: 1+ reaction to benzocaine and balsam of Peru in ISS |
Both of our patients presented with an extreme degree of oral mucosal discomfort despite the tendency towards clinical resolution of the primary disease. Burning mouth syndrome or orodynia is a chronic pain condition that can be caused by several factors, namely drugs, stress, anxiety and depression, none of which was borne out by detailed questioning in our patients. Such a clinical scenario of orodynia, in the absence of any clinical signs is very difficult to diagnose and treat. The temporal correlation between application of benzocaine and onset of symptoms and the simultaneous presence of dermatitic rash over the perioral area and fingers in the first patient helped us in suspecting allergic contact dermatitis. Recently, a retrospective study of patch test results from a large case series of patients with burning mouth syndrome demonstrated contact allergy to be an etiologic factor in a significant number of patients. [1] Notably, examination of oral mucosa was non-contributory in both the patients, which is odd for a true contact allergy. The most plausible explanation for this could be that gel preparations are easily washed off from the mucosal surface and contact allergy manifests only by symptomatic distress. Also, they were being treated concomitantly with topical steroids which could have masked the clinical signs of inflammation in the mucosa.
Benzocaine, a common and potent contact sensitizer, is currently the sole screening hapten among local anesthetics in the Indian as well as the European standard series. The issue of replacing it with caine mix (benzocaine, tetracaine and cinchocaine) with the aim of increasing the sensitivity of detecting contact allergies to local anesthetics is a matter of debate. [2] The incidence of benzocaine allergy seems to vary in different parts of the world depending upon the prescription pattern. Published data shows variable patch test positivity rates, being 2.6% in the United States, [3] 1% in Denmark and 10% in Germany. [4] In India, numerous formulations containing benzocaine are easily available as over-the-counter preparations: oral preparations such as antitussives, astringents and antibacterial mouthwashes, anesthetic gels for toothache, cold sores and denture irritation, as well as skin creams and gels for abrasions, burns, insect bites and leg ulcers etc. Benzocaine, used in the anogenital area as antihemorrhoidal creams, soothing creams for anal and vulvar pruritus, anesthetic gels in condoms and condom catheters etc. is being increasingly recognized as an important, yet underestimated cause for contact and even connubial contact allergies. [5]
Cross reactivity is not unique within the ester group of local anesthetics such as tetracaine and procaine, but also extends beyond this class. Benzocaine tends to cross-react with related compounds which have an amino group in the para-position of the benzene ring viz., paraphenylenediamine, sulfonamides, sulphonyl ureas, dapsone, azo dyes and PABA-derivative sunscreens. Patch test results from our first patient also demonstrated cross reactivity with paraphenylenediamine. However, sensitization to sulfonamide drugs in both patients could not be confirmed as they did not consent to oral provocation tests. Reports from the literature suggest that this possible risk of multiple cross-sensitivity should caution benzocaine-sensitive individuals to avoid related compounds in future. [2] Moreover, past exposure to cross-sensitizing allergens significantly shortens the induction period of allergic contact dermatitis to benzocaine from 7-20 days to as short as 48-72 hours, as evident in our first patient. [6] This is true for topical sensitization with para-amino compounds resulting in systemic contact dermatitis with oral drugs later, but vice versa i.e. systemic sensitization leading to contact dermatitis is considered to be rare. [7] Although systemic absorption of benzocaine is negligible, it gets metabolized to PABA, which is highly allergenic and capable of inducing systemic contact dermatitis later.
| 1. |
Lynde CB, Grushka M, Walsh SR. Burning mouth syndrome: Patch test results from a large case series. J Cutan Med Surg 2014;18:174-9.
[Google Scholar]
|
| 2. |
Sidhu SK, Shaw S, Wilkinson JD. A 10-year retrospective study on benzocaine allergy in the United Kingdom. Am J Contact Dermat 1999;10:57-61.
[Google Scholar]
|
| 3. |
Marks JG, Belsito DV, DeLeo VA, Fowler JF Jr, Fransway AF, Maibach HI, et al. North American Contact Dermatitis Group patch test results for the detection of delayed-type hypersensitivity to topical allergens. J Am Acad Dermatol 1998;38:911-8.
[Google Scholar]
|
| 4. |
Fregert S, Hjorth N, Magnusson B, Bandmann HJ, Calnan CD, Cronin E, et al. Epidemiology of contact dermatitis. Trans St Johns Hosp Dermatol Soc 1969;55:17-35.
[Google Scholar]
|
| 5. |
Muratore L, Calogiuri G, Foti C, Nettis E, Di Leo E, Vacca A, et al. Contact allergy to benzocaine in a condom. Contact Dermatitis 2008;59:173-4.
[Google Scholar]
|
| 6. |
Arroyo MP. Black henna tattoo reaction in a person with sulfonamide and benzocaine drug allergies. J Am Acad Dermatol 2003;48:301-2.
[Google Scholar]
|
| 7. |
Fisher AA. Systemic contact dermatitis from orinase and diabenese in diabetics with para-amino hypersensitivity. Cutis 1982;29:551,556,565.
[Google Scholar]
|
Fulltext Views
4,435
PDF downloads
3,364





