Translate this page into:
Efficacy and relapse rates of different treatment modalities for progressive macular hypomelanosis
2 Yong Loo Lin School of Medicine, National University of Singapore, Singapore
3 National Skin Centre, Nanyang Technological University, Singapore
Correspondence Address:
Steven T. G. Thng
National Skin Centre, 1 Mandalay Road, 308205
Singapore
| How to cite this article: Thng ST, Long VS, Chuah SY, Tan VW. Efficacy and relapse rates of different treatment modalities for progressive macular hypomelanosis. Indian J Dermatol Venereol Leprol 2016;82:673-676 |
Abstract
Background: Progressive macular hypomelanosis is an acquired disorder characterized by hypopigmented macules mostly on the trunk and upper extremities. Although many treatment modalities have been proposed for this condition with variable success rates, there are few reports comparing their efficacy and relapse rates. Aim: To compare the efficacy and relapse rates of different treatment modalities for progressive macular hypomelanosis. Methods: Case records of patients diagnosed with progressive macular hypomelanosis and treated in National Skin Centre for a six year period between 2008 and 2014 were reviewed. Patient demographics, distribution of hypopigmented macules, treatment efficacy and relapse rates were noted. Results: A total of 108 patients were seen for progressive macular hypomelanosis over the study period; of these, 40 opted for no treatment but were followed up. Thirty-six were treated with topical antimicrobials and 32 with phototherapy. Of those untreated, 23% recovered spontaneously while 38% in the antimicrobial group and 90% in the phototherapy had remission of their hypopigmentation. After 2 years of follow-up, relapse occurred only in the phototherapy group. Limitations: The main limitation is the retrospective design whereby diagnosis is dependent on the attending dermatologist. Conclusions: Narrow-band ultraviolet B therapy appears to be the most effective treatment for progressive macular hypomelanosis but also has the highest potential for relapse. Response rates for antimicrobial therapy are lower and slower, but patients who responded did not relapse. A combination of topical/systemic antimicrobials with narrow-band ultraviolet B therapy might be the best option to hasten recovery and minimize relapse.Introduction
Progressive macular hypomelanosis is an acquired disorder characterized by hypopigmented macules, without previous history of inflammation or injury.[1],[2] Many treatment modalities have been proposed but none are universally effective.[3],[4],[5],[6],[7] Narrow-band ultraviolet B is the treatment of choice for progressive macular hypomelanosis in many centers.[4],[5],[7] Other treatment modalities include benzoyl peroxide, oral tetracyclines and isotretinoin.[3],[8],[9] We were unable to find previously published comparisons of efficacy and relapse rates between treatment modalities for this condition.
Methods
A retrospective analysis of all cases of progressive macular hypomelanosis diagnosed and treated in National Skin Centre, a tertiary dermatological unit in Singapore, from January 1, 2008, to January 1, 2014, was performed. The diagnosis of progressive macular hypomelanosis was mainly clinical, supported by laboratory investigations such as skin scraping and/or biopsy. The latter was done only in cases suspected to be hypopigmented mycosis fungoides. All patients whose scrapings were positive for pityriasis versicolor, or whose biopsies showed mycosis fungoides were excluded from the study. Patient demographics, distribution of hypopigmented macules, treatment efficacy as well as relapse rates were noted. For those treated with narrow-band ultraviolet B, phototherapy was given twice a week in a Daavlin cabinet (Daavlin, Bryan, OH, USA) equipped with Philips TL-01/100 W fluorescent lamps (Philips Company, Eindhoven, the Netherlands).
In this study, repigmentation greater than 80% was classified as treatment success, and less than 80% as treatment failure. Ethics approval was obtained from the local domain-specific review board.
Results
Clinical characteristics
A total of 108 patients, consisting of 30 (28%) women and 78 (72%) men were included in the study. The mean age was 24.4 ± 8.4 (median: 22.5) years, and the duration of disease at presentation was 31.3 ± 32.2 (median: 24.0) months. Most patients were asymptomatic. Only nine patients complained of mild itch. The demographics and clinical characteristics are shown in [Table - 1].
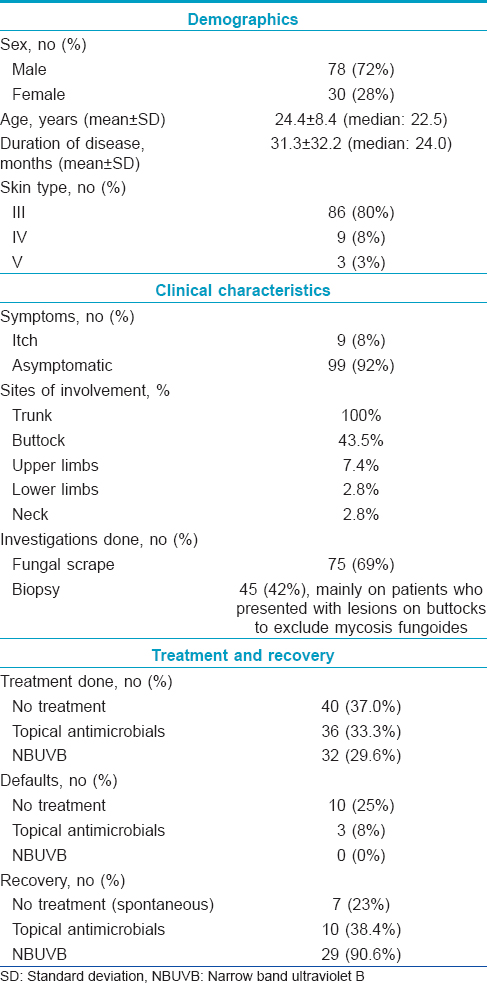
All patients had truncal lesions, with 43.5% of the patients having lesions that extended to the buttocks. Other affected areas included the upper limbs (7.4%), neck (2.8%) and lower limbs (2.8%). Classically, the lesions were ill-defined nummular, hypopigmented, non-scaly macules on the trunk with a confluence of the macules in and around the midline [Figure - 1].
 |
| Figure 1: (a) Patient with progressive macular hypomelanosis before treatment. (b) Patient with progressive macular hypomelanosis after 2 months of narrow-band ultraviolet B |
Investigations done
Scraping was done on 75 (69%) patients to exclude Malassezia furfur infection. In addition, a biopsy was done on 45 (42%) patients with buttock involvement to exclude mycosis fungoides.
Treatment efficacy and relapse rates
Forty (37%) of the patients opted not to go for any treatment when assured that the condition is benign. Of these, 30 patients continued to be on follow-up during which seven (23%) had spontaneous resolution. The average time to resolution was 10.2 ± 4.0 months (median: 12.0, range: 3–22).
Thirty-six (33.3%) patients were treated with topical clindamycin and/or topical benzoyl peroxide. Thirty three patients from this group were compliant with the treatment and follow-up. Of these, 10 (38%) achieved good repigmentation in an average of 8.5 ± 6.7 months (median: 6, range: 3–26). None of these patients relapsed during a follow-up period of 2 years.
Thirty two patients (30%) were treated with narrow-band ultraviolet B phototherapy twice a week. All patients were compliant with this treatment for at least 3 months. In this group, more than 90% of the patients achieved greater than 80% repigmentation in a shorter time period with an average time to resolution of about 2.5 ± 1.3 months. The mean number of treatments and cumulative ultraviolet B dose of phototherapy were 22.3 and 2540 mJ, respectively. The mean number of treatments required for the initial response was 6.4.
Of all those who responded to treatment with narrow-band ultraviolet B, 6% experienced a relapse and this occurred in an average of 10.2 ± 13.2 months (median: 4.0, range: 2–36).
Discussion
Since progressive macular hypomelanosis was first described in 1985 by Guillet et al., many reports have appeared over the past two decades detailing the clinical, histopathological characteristics and possible etiologies as well as treatment options for the condition.[2] However, the exact cause for the condition is still unknown. Currently, the most widely accepted view is that progressive macular hypomelanosis is probably due to infection of the pilosebaceous unit by Propionibacterium acnes. This is based on a serendipitous observation by Westerhof et al., wherein they discovered coral red fluorescence when lesions were examined under Woods lamp.[10] Subsequently, they were able to isolate Propionibacterium acnes in pilo-sebaceous units of lesional skin. The natural history of progressive macular hypomelanosis is elusive. While some authors have suggested that it might disappear spontaneously within 3–5 years, there are no studies documenting this spontaneous recovery.[11] We found that close to 23% of our patients improved spontaneously without any treatment when they were followed up for more than 2 years. In the remaining 77% without treatment, the condition seemed to persist beyond the 2-year follow-up, with some persisting even after 5 years (results not shown here).
For those who spontaneously recovered, the time taken for resolution was about 1 year. It is not possible to predict spontaneous recovery based on clinical or demographic characteristics. Mahe et al. suggested that progressive macular hypomelanosis is a “normal” variation of the skin which “fades away” after the fifth decade resulting in spontaneous recovery of the condition.[12] However, this is clearly not the case in this study as spontaneous recovery occurred within 1–2 years.
There is no widely accepted first-line treatment for progressive macular hypomelanosis. The hypothetical overgrowth of Propionibacterium acnes in patients with this condition has prompted many investigators to use antimicrobial therapies aimed at its eradication. The response rates to topical antimicrobial therapies were low in this study with only 38.4% of our patients responding to the treatment. This is much lower than the 85% response rate reported by Santos et al.[3] We believe that the low response rates in our group of patients could be explained by poor compliance as the disease is usually extensive involving the trunk and most of our patients reported that they found it difficult to apply the medication on the back. Patients in Santos's study were also told to expose the affected areas to the sun, The ultraviolet exposure could possibly have helped in the eradication of Propionibacterium acnes, especially in areas where topical medications are hard to apply. We were unable to find any previous studies documenting the relapse rates in cases treated with topical antimicrobial therapy. None of our patients who responded to antimicrobial therapy experienced any relapse at all and this is interesting, as progressive macular hypomelanosis has been known to relapse after stopping treatment.[7]
The other well-documented treatment for progressive macular hypomelanosis is narrow-band ultraviolet B phototherapy. There are several theories supporting its use. Narrow-band ultraviolet B has been shown to exhibit excellent antibacterial properties [13] and also promotes the synthesis of melanin by stimulating residual melanocytes while also increasing the melanization in melanosomes. Kim et al., in their case series showed that 56.2% of patients, responded with more than 90% repigmentation.[7] In our study, we recorded more than 90% of patients achieving greater than 80% repigmentation. The time for the first response was usually within 4–8 sessions of narrow-band ultraviolet B and time for maximal repigmentation was about 22 sessions. From our data, it can be suggested that if patients do not respond within 12 sessions, it may not be advisable to continue with phototherapy. These observations are somewhat similar to those of Kim et al.[7] In addition, phototherapy should be continued till about 22 sessions to achieve maximal repigmentation. The relapse rate in our cases was about 6%, much lower than 31% reported by Kim et al.[7] In our cases, relapse usually occurred within 7 months (range: 2–36) of discontinuing the therapy but was observed as late as 3 years after the cessation of therapy. There were no clinical or demographic characteristics that could predict relapse rates. With regard to relapse of progressive macular hypomelanosis upon cessation of narrow-band ultraviolet B treatment, we hypothesize that it acts mainly to encourage repigmentation but is not very effective in eradicating Propionibacterium acnes completely resulting in re-infection of pilosebaceous unit when the bacteriostatic effect of narrow-band ultraviolet B is removed.
Conclusion
Our data supports the current understanding that progressive macular hypomelanosis occurs mainly in adolescence or young adults and runs a chronic and indolent course, although spontaneous resolution might occur in a small proportion of patients. We postulate that a combination of topical/systemic antimicrobial therapy with narrow-band ultraviolet B might be the best option to hasten recovery and minimize relapse.
The strengths of this study lie in it being the first study to compare the clinical efficacy of using narrow-band ultraviolet B alone against the use of antimicrobial monotherapy. In addition, we have a fairly large sample size of more than 100 patients. The main limitation is the retrospective design whereby diagnosis is very much dependent on the dermatologist attending to the patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Borelli D. Cutis “trunci variata.” A new genetic dermatosis. Med Cutan Ibero Lat Am 1987;15:317-9.
[Google Scholar]
|
| 2. |
Guillet G, Helenon R, Gauthier Y, Surleve-Bazeille JE, Plantin P, Sassolas B. Progressive macular hypomelanosis of the trunk: Primary acquired hypopigmentation. J Cutan Pathol 1988;15:286-9.
[Google Scholar]
|
| 3. |
Santos JB, Almeida OL, Silva LM, Barreto ER. Efficacy of topical combination of benzoyl peroxide 5% and clindamycin 1% for the treatment of progressive macular hypomelanosis: A randomized, doubleblind, placebo-controlled trial. An Bras Dermatol 2011;86:50-4.
[Google Scholar]
|
| 4. |
Kanwar AJ, Dogra S, Parsad D, Kumar B. Narrow-band UVB for the treatment of vitiligo: An emerging effective and well-tolerated therapy. Int J Dermatol 2005;44:57-60.
[Google Scholar]
|
| 5. |
Barbagallo J, Spann CT, Tutrone WD, Weinberg JM. Narrowband UVB phototherapy for the treatment of psoriasis: A review and update. Cutis 2001;68:345-7.
[Google Scholar]
|
| 6. |
Relyveld GN, Kingswijk MM, Reitsma JB, Menke HE, Bos JD, Westerhof W. Benzoyl peroxide/clindamycin/UVA is more effective than fluticasone/UVA in progressive macular hypomelanosis: A randomized study. J Am Acad Dermatol 2006;55:836-43.
[Google Scholar]
|
| 7. |
Kim MB, Kim GW, Cho HH, Park HJ, Kim HS, Kim SH, et al. Narrowband UVB treatment of progressive macular hypomelanosis. J Am Acad Dermatol 2012;66:598-605.
[Google Scholar]
|
| 8. |
Kim YJ, Lee DY, Lee JY, Yoon TY. Progressive macular hypomelanosis showing excellent response to oral isotretinoin. J Dermatol 2012;39:937-8.
[Google Scholar]
|
| 9. |
Elmariah SB, Kundu RV. Progressive macular hypomelanosis. J Drugs Dermatol 2011;10:502-6.
[Google Scholar]
|
| 10. |
Westerhof W, Relyveld GN, Kingswijk MM, de Man P, Menke HE. Propionibacterium acnes and the pathogenesis of progressive macular hypomelanosis. Arch Dermatol 2004;140:210-4.
[Google Scholar]
|
| 11. |
Lesueur A, Garcia-Granel V, Helenon R, Cales-Quist D. Progressive macular confluent hypomelanosis in mixed ethnic melanodermic subjects: An epidemiologic study of 511 patients. Ann Dermatol Venereol 1994;121:880-3.
[Google Scholar]
|
| 12. |
Tyring S, Lupi O, Hengge U. Tropical Dermatology. Edinburgh: Elsevier Churchill Livingstone; 2006.
[Google Scholar]
|
| 13. |
Fluhr JW, Gloor M. The antimicrobial effect of narrow-band UVB (313 nm) and UVA1 (345-440 nm) radiation in vitro. Photodermatol Photoimmunol Photomed 1997;13:197-201.
[Google Scholar]
|
Fulltext Views
12,037
PDF downloads
2,035





