Translate this page into:
Efficacy and safety of Erbium-doped Yttrium Aluminium Garnet fractional resurfacing laser for treatment of facial acne scars
Correspondence Address:
Sathish B Pai
Department of Dermatology, Kasturba Medical College, Manipal University, Manipal
India
| How to cite this article: Nirmal B, Pai SB, Sripathi H, Rao R, Prabhu S, Kudur MH, Nayak SU. Efficacy and safety of Erbium-doped Yttrium Aluminium Garnet fractional resurfacing laser for treatment of facial acne scars. Indian J Dermatol Venereol Leprol 2013;79:193-198 |
Abstract
Background: Treatment of acne scars with ablative fractional laser resurfacing has given good improvement. But, data on Indian skin are limited. A study comparing qualitative, quantitative, and subjective assessments is also lacking. Aim: Our aim was to assess the improvement of facial acne scars with Erbium-doped Yttrium Aluminium Garnet (Er:YAG) 2940 nm fractional laser resurfacing and its adverse effects in 25 patients at a tertiary care teaching hospital. Methods: All 25 patients received four treatment sessions with Er:YAG fractional laser at 1-month interval. The laser parameters were kept constant for each of the four sittings in all patients. Qualitative and quantitative assessments were done using Goodman and Barron grading. Subjective assessment in percentage of improvement was also documented 1 month after each session. Photographs were taken before each treatment session and 1 month after the final session. Two unbiased dermatologists performed independent clinical assessments by comparing the photographs. The kappa statistics was used to monitor the agreement between the dermatologists and patients. Results: Most patients (96%) showed atleast fair improvement. Rolling and superficial box scars showed higher significant improvement when compared with ice pick and deep box scars. Patient's satisfaction of improvement was higher when compared to physician's observations. No serious adverse effects were noted with exacerbation of acne lesions forming the majority. Conclusion: Ablative fractional photothermolysis is both effective and safe treatment for atrophic acne scars in Indian skin.Precise evaluation of acne scar treatment can be done by taking consistent digital photographs.Introduction
Atrophic scars are the dermal depressions commonly caused by the destruction of collagen after inflammatory acne. [1] Many therapeutic measures such as chemical peeling, [2] subcision, [3] dermabrasion, [4] fillers, [5] and punch techniques [6] have been performed to improve acne scarring but with suboptimal outcomes. Although significant clinical improvements can be seen with ablative lasers, adverse effects such as prolonged post-procedure erythema [7] and dyspigmentation [8] impede their widespread use especially in patients with darker skin. On the other hand, non-ablative lasers [9] such as diode, Neodymium-doped Yttrium Aluminum Garnet (Nd:YAG) and pulsed dye laser have better safety profiles but lower efficacies. Fractional laser resurfacing technique [10] was developed to address the drawbacks of both ablative and non-ablative lasers.
However, data on the efficacy and adverse effects of this novel resurfacing technique in Indian skin are limited. Also a good clinical study comparing qualitative and quantitative assessments of pre- and post-treatment photographs after standardizing them, along with subjective assessment is lacking.
Methods
Aim and objectives
Our aim and objectives were to assess the improvement of acne scars quantitatively, qualitatively and subjectively; then to estimate the improvement with respect to duration, grade and type of acne scars. We also wanted to look for the most common adverse reactions and their incidence.
Study design
The study was designed as a clinical trial using fractional laser resurfacing for the treatment of atrophic facial acne scars in 25 patients from June 2010 to October 2011. Patients diagnosed with atrophic acne scarring aged 18 years or above were included. Those with known photosensitivity, pregnancy, lactation, keloidal tendency, use of oral retinoids in last 6 months, infections like herpes labialis, active acute illness in last 4 weeks, and unrealistic expectations were excluded.
Ethical considerations
A written and signed informed explanatory consent was taken from all the patients before initiation of therapy. This clinical study was performed in accordance with the declaration of Helsinki after approval by the ethic committee of our hospital.
Laser treatment
All 25 patients received four sittings of laser treatment at 1-month interval. They were treated with fractional ablative resurfacing module using 2940 nm Er:YAG handpiece. A cooling device delivering cold air was used to reduce pain sensation during and after treatment. Parameters for each sitting were kept constant in all patients. First and second sessions were performed using 9 × 9 tips with fluence of 1,200 and 1,400 mJ, respectively. Third and fourth sessions were performed using 7 × 7 tips with fluence of 1,200 and 1,400 mJ respectively. Long pulse mode (2 Hz) was used for all four sessions. Three passes in vertical, horizontal, and oblique directions with upto 50% overlapping between the adjacent pulses and stacking was done over scar areas where five pulses were given in exactly same place without moving the tip. Strict photoprotection was advised as a routine and topical antibiotic-steroid combination was applied for 3 days post-procedure.
Assessment of efficacy
Qualitative assessment
Qualitative assessment was done using Goodman and Barron (GB) qualitative global scarring grading system [11] which has four grades viz., macular, mild, moderate and severe.
Quantitative assessment
Quantitative assessment was done using GB quantitative global scarring grading system. [12] Different types of scars were given increasing scores and multiplied depending on the number of scars in each type giving a maximum score of 84.
Subjective assessment
The patients were asked to quantify their percentage of improvement 1 month after each treatment session and their subjective assessment of improvement of scars was also documented.
Photography assessment
We designed an instrument [Figure - 1] in our workshop to ensure that photographs were taken with identical patient positioning, lighting, and camera settings. Small inconsistencies with patient positioning were corrected using image analysis software.
 |
| Figure 1: The instrument used for taking consistent photographs |
Serial photographs were assessed by two unbiased, certified dermatologists. Physician evaluations and patient satisfaction were graded on a four-point scale viz., none, fair, good, and excellent improvement.
Assessment of safety
Subjects were instructed to report any cutaneous side-effects including erythema, oozing, crusting, dyschromia, scarring or secondary infection after laser treatment. Patients were specifically asked about immediate post-treatment sequelae and about interference with daily activities in the post-treatment period and report if any.
Statistical analysis
The results were statistically analyzed using SPSS version 11.0 (SPSS, Inc., Chicago, IL, USA). Differences were considered statistically significant when p < 0.05. The kappa statistic was used as a measure of agreement between physicians and patients.
Results
Patient demographics
A total of 25 patients with acne scars of skin phototypes IV-V participated in the study comprising of 15 males (60%) and 10 females (40%). They belonged to the age group of 18-38 years. The duration of scars ranged from as less as 6 months to 15 years. Most patients had grade 4 acne scars constituting 48% (12 cases) of the study population followed by grade 2 (seven cases), grade 3 (six cases), and nil in grade 1. Superficial box, deep box, rolling, ice pick scars were present predominately in eight, seven, seven, and three cases, respectively.
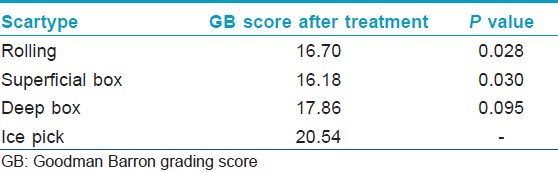
Estimation of improvement with respect to the type of scar
Analysis of covariance was performed and results were evaluated using GB quantitative score-before treatment value of 27.60 as covariate. The difference in mean values between rolling (16.7) and ice pick scars (20.54) after adjusting for the GB-before scores at 27.6 was statistically significant (p =0.028). The superficial box (16.18) also showed a statistically significant (p =0.030) difference in the mean as compared to the ice pick scars [Table - 1]. There was no statistically significant difference in the mean values between deep box (17.86) and ice pick scars (p =0.095).
There was no statistically significant variation of improvement with respect to duration as well as grade of acne scars.
Comparison of patient satisfaction between sittings
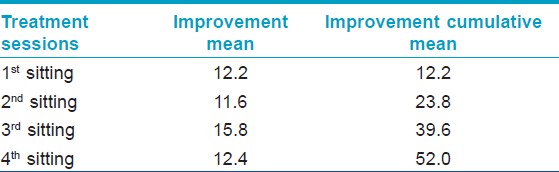
The patient′s satisfaction between first, second, third, and fourth sittings [Figure - 2] was computed using general linear model. Higher significant improvement was seen after the third sitting with the mean improvement in the GB quantitative score increasing to 15.8 after third sitting [Table - 2]. The graph [Figure - 3] shows the steep increase in improvement after the third sitting.
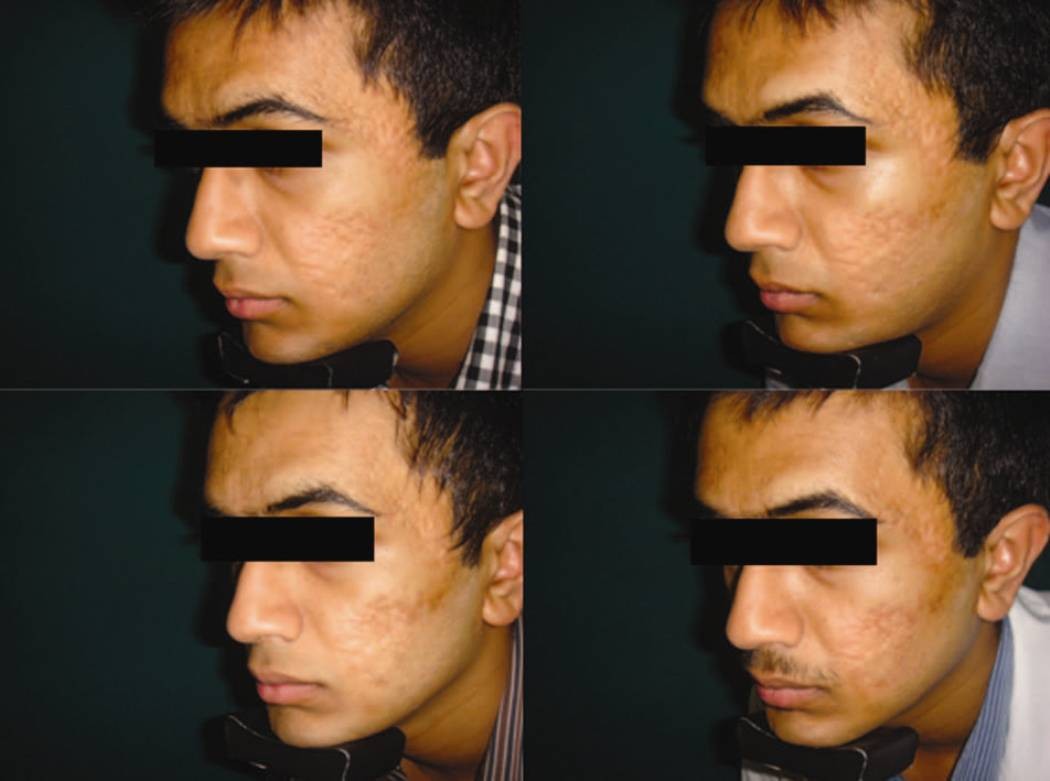 |
| Figure 2: Digital photographs after first, second, third, and fourth sittings |
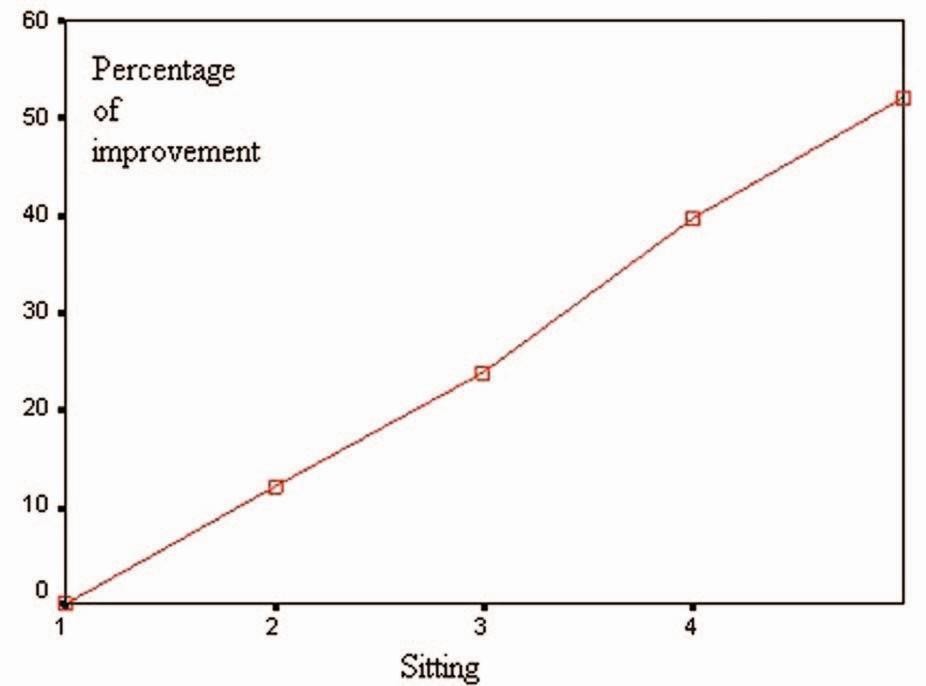 |
| Figure 3: Graph showing the percentage of improvement after each sitting |
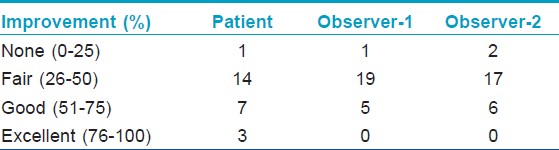
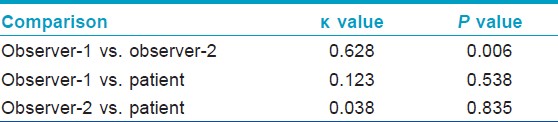
Comparison of patient′s satisfaction and inter-observer variation
Patient′s satisfaction scores were higher in comparison to both observers′ rating with a relatively higher proportion of improvement grading in the good and excellent categories [Table - 3]. The kappa statistic was used to monitor the agreement between observers, patient and observer-1, and patient and observer-2. The observers [Figure - 4] showed statistically significant [Table - 4] substantial agreement between each other (κ=0.61-0.8), whereas the patient′s agreement with observer-1 and observer-2 was only slight (κ=0-0.2).
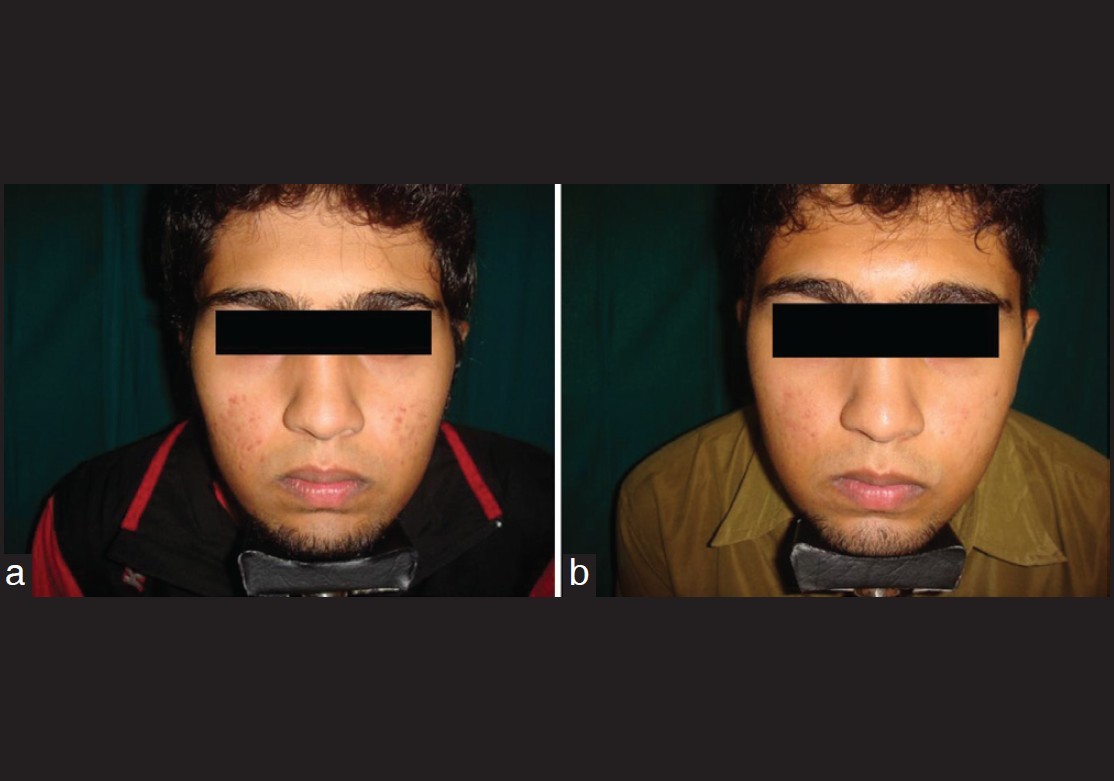 |
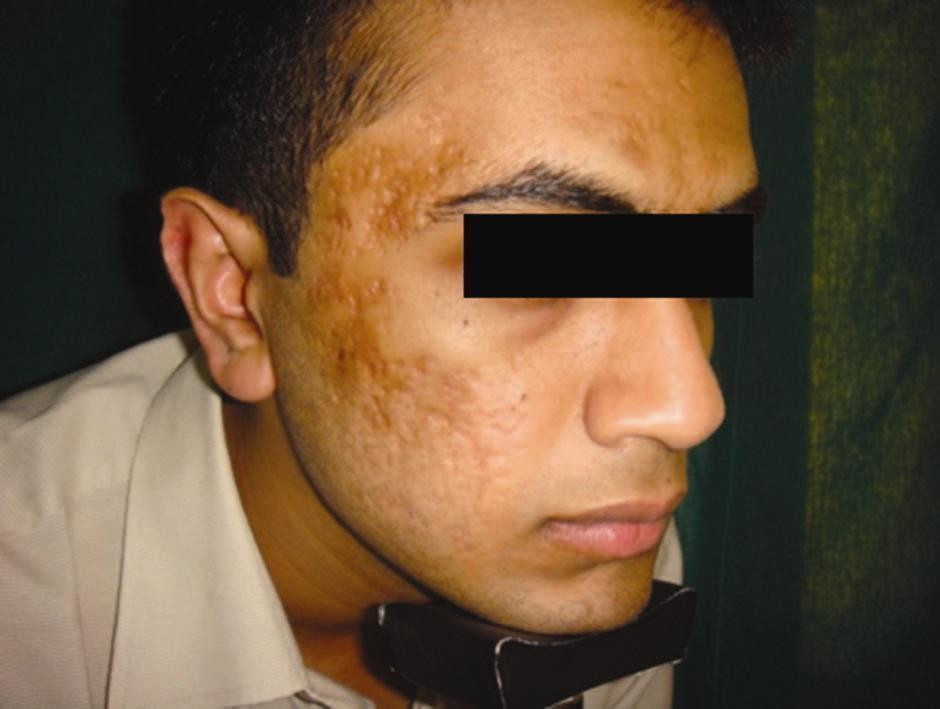
| Figure 4: Patient, observer-1, and observer-2 agreed good (50-75%) improvement (a) before treatment (b) after treatment |
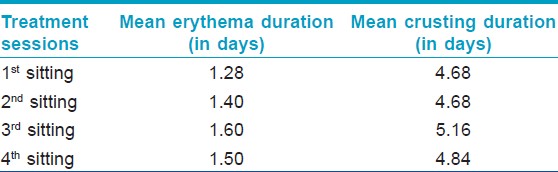
Adverse reactions
Most common side-effect seen after 100 sittings (25 patients × 4 sittings each) of Er:YAG 2940nm fractional laser resurfacing was exacerbation of acne lesions (13%) which was treated with oral antibiotics. Post-treatment pigmentation was seen only in 2% and was effectively treated with demelanizing creams. Prolonged crusting (more than 7 days) was seen after 3% of the sittings. None of the patients had prolonged erythema (more than 4 days) after undergoing treatment sessions. The mean erythema duration was less than 2 days and mean crusting was around 5 days in all sittings [Table - 5]. [Figure - 5] shows the appearance immediately after the laser treatment showing the stamping effect of pixel laser, 1 day post-treatment showing erythema, 3 days post-treatment showing crusting, and 7 days post-treatment with complete clearance of erythema and crusting.
 |
| Figure 5: Sequence of events post- laser treatment: (a) Immediate post laser, (b) 1 day post laser, (c) 3 days post laser, (d) 7 days post laser |
Discussion
Resurfacing lasers date back to 1980s using ablative carbondioxide lasers, [13] which are based on the theory of selective photothermolysis. [14] Non-ablative lasers were developed to combat the side-effect profiles of ablative lasers but had unpredictable efficacy. Fractional photothermolysis (FP) was devised by Manstein and colleagues in 2004. [15] The results of first fractional non-ablative laser (1,550 nm Er:glass laser) [16] were still unsatisfactory. The need for better results led to the combination of the theory of FP and ablative laser technologies producing ablative fractional resurfacing [17] to address the drawbacks of both ablative and non-ablative lasers, thus considered "the best of both worlds." The principle of FP is targeting water as a chromophore. Water-rich targets in skin include epidermal keratinocytes, collagen and blood vessels. [18] FP involves the application of multiple beams of pixilated light producing microscopic treatment zones. [19] Thermal damage initiates a biological signaling cascade [20] leading to increased expression of heat shock protein which causes upregulation of transforming growth factor beta, a facilitator of collagen synthesis. [21] Healing is faster since most of the surrounding tissue is spared from thermal damage with replacement of epidermis and expulsion of microscopic exudative necrotic debris, composed of elastin and melanin. [22]
This study demonstrates that Er:YAG 2940 nm fractional resurfacing laser effectively improves acne scars with minimal downtime and a low risk of adverse reactions. After four treatments with Er:YAG 2940 nm fractional laser, 24 out of 25 subjects rated themselves as having at least 25-50% overall satisfaction which was similar to the physicians′ grading. This observation was consistent with the finding of fractional laser in darker skin types by Manuskiatti et al.,[23] Hu et al.,[24] Alster et al.,[25] and Mahmoud et al.[26] The difference in agreement was noticed when observing the number of patients reporting more than 50% improvement (good to excellent) as compared with the observers′ rating. Forty percent of the subjects noticed good to excellent improvement as opposed to 20-24% in the observers. Patients felt better probably because of the additional benefits of fractional laser in decreasing pigmentation, decreasing fine lines, skin tightening, and pore reduction. This is the reason why though the patients had only a fair improvement after pixel laser, they felt the laser′s efficacy to be good or excellent. Twelve percent of the patients reported excellent improvement with the highest being 85% improvement.
Post-inflammatory hyperpigmentation (PIH) was the most common side-effect as observed by Manuskiatti et al.[23] in 92.3% patients. In our experience, PIH [Figure - 6] was low (2%) in Er:YAG ablative fractional resurfacing, suggesting that it can be safely performed in Indian skin. Our findings were consistent with that observed by Hu et al.,[27] where also the incidence of PIH was less, seen only in 3% of the cases in 34 patients with Fitzpatrick skin types III and IV using ablative fractional Er:YAG laser. Downtime was also acceptable in our study with mean value less than 7 days in all four sittings. Prolonged erythema was seen in none of the sittings and only 3% showed prolonged crusting. Exacerbation of acne lesions [Figure - 7] was the most common adverse effect of fractional laser in our study which developed after 13% of the sittings which could be due to the steroid-antibiotic cream used for 3 days after treatment. This was comparable to the observations by Hu et al.[27] in his study of 34 patients using Er:YAG laser for atrophic facial acne scars in Asian skin where acne eruption was seen in 24.2% of patients.
 |
| Figure 6: Post-inflammatory hyper pigmentation |
 |
| Figure 7: Exacerbation of acne lesions |
Conclusion
Ninety-six percent of the subjects rated themselves as having at least fair improvement. Rolling and superficial box scars showed higher significant improvement when compared to ice pick and deep box scars. Patient′s satisfaction of improvement was higher when compared to physician′s observations and it increased markedly after third sitting. Incidence of adverse effects post-laser was very less and period of recovery was also not prolonged. Thus, the results of this study support the use of FP for the safe and effective treatment of atrophic facial acne scars.
Future Recommendations
As improvement in patient rating increases markedly after third sitting and incidence of side-effects was minimal even in type V skin, we recommend future studies to start with the fluence of third sitting over scar area and regular protocol on rest of the face similar to spot peels for melasma where higher concentration is used over pigmented area and lower concentration over the rest of the face. As the improvement was increasing with every sitting, we also recommend further studies to be undertaken with more treatment sessions.
Acknowledgments
We would like to acknowledge our professors Dr. Shrutakirthi D. Shenoi and Dr. C. Balachandran for their observation and assessment of photographs in this study. We also thank Dr. Asha Kamath, Assistant professor, Department of Community Medicine, Kasturba Medical College, Manipal for statistical analysis of the data. We would like to thank the patients for providing consent to use their photographs in this article.
| 1. |
Holland DB, Jeremy AH, Roberts SG, Seukeran DC, Layton AM, Cunliffe WJ. Inflammation in acne scarring: A comparison of the responses in lesions from patients prone and not prone to scar. Br J Dermatol 2004;150:72-81.
[Google Scholar]
|
| 2. |
Slavin JW. Trichloroacetic acid peels. Aesthet Surg J 2004;24:469-70.
[Google Scholar]
|
| 3. |
Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg 1995;21:543-9.
[Google Scholar]
|
| 4. |
Alkhawam L, Alam M. Dermabrasion and microdermabrasion. Facial Plast Surg 2009;25:301-10.
[Google Scholar]
|
| 5. |
Hirsch RJ, Cohen JL. Soft tissue augmentation. Cutis 2006;78:165-72.
[Google Scholar]
|
| 6. |
Grevelink JM, White VR. Concurrent use of laser skin resurfacing and punch excision in the treatment of facial acne scarring. Dermatol Surg 1998;24:527-30.
[Google Scholar]
|
| 7. |
Dierickx CC, Khatri KA, Tannous ZS, Childs JJ, Cohen RH, Erofeev A, et al.0 Micro-fractional ablative skin resurfacing with two novel erbium laser systems. Lasers Surg Med 2008;40:113-23.
[Google Scholar]
|
| 8. |
Kono T, Chan HH, Groff WF, Manstein D, Sakurai H, Takeuchi M, et al. Prospective direct comparison study of fractional resurfacing using different fluences and densities for skin rejuvenation in Asians. Lasers Surg Med 2007;39:311-4.
[Google Scholar]
|
| 9. |
Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of laser skin resurfacing: Nonablative, fractional, and ablative laser resurfacing. J Am Acad Dermatol 2008;58:719-37.
[Google Scholar]
|
| 10. |
Tierney EP, Kouba DJ, Hanke CW. Review of fractional photothermolysis: Treatment indications and efficacy. Dermatol Surg 2009;35:1445-61.
[Google Scholar]
|
| 11. |
Goodman GJ, Baron JA. Postacne scarring: A qualitative global scarring grading system. Dermatol Surg 2006;32:1458-66.
[Google Scholar]
|
| 12. |
Goodman GJ, Baron JA. Postacne scarring: A quantitative global scarring grading system. J Cosmet Dermatol 2006;5:48-52.
[Google Scholar]
|
| 13. |
Brightman LA, Brauer JA, Anolik R, Weiss E, Karen J, Chapas A, et al. Ablative and fractional ablative lasers. Dermatol Clin 2009;27:479-89.
[Google Scholar]
|
| 14. |
Anderson RR, Parrish JA. Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation. Science 1983;220:524-7.
[Google Scholar]
|
| 15. |
Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med 2004;34:426-38.
[Google Scholar]
|
| 16. |
Bodendorf MO, Grunewald S, Wetzig T, Simon JC, Paasch U. Fractional laser skin therapy. J Dtsch Dermatol Ges 2009;7:301-8.
[Google Scholar]
|
| 17. |
Goel A, Krupashankar DS, Aurangabadkar S, Nischal KC, Omprakash HM, Mysore V. Fractional lasers in dermatology-Current status and recommendations. Indian J Dermatol Venereol Leprol 2011;77:369-79.
[Google Scholar]
|
| 18. |
Hantash BM, Bedi VP, Kapadia B, Rahman Z, Jiang K, Tanner H, et al. In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med 2007;39:96-107.
[Google Scholar]
|
| 19. |
Khan MH, Sink RK, Manstein D, Eimerl D, Anderson RR. Intradermally focused infrared laser pulses: Thermal effects at defined tissue depths. Lasers Surg Med 2005;36:270-80.
[Google Scholar]
|
| 20. |
Tierney EP, Kouba DJ, Hanke CW. Review of fractional photothermolysis: Treatment indications and efficacy. Dermatol Surg 2009;35:1445-61.
[Google Scholar]
|
| 21. |
Hantash BM, Mahmood MB. Fractional photothermolysis: A novel aesthetic laser surgery modality. Dermatol Surg 2007;33:525-34.
[Google Scholar]
|
| 22. |
Laubach HJ, Tannous Z, Anderson RR, Manstein D. Skin responses to fractional photothermolysis. Lasers Surg Med 2006;38:142-9.
[Google Scholar]
|
| 23. |
Manuskiatti W, Triwongwaranat D, Varothai S, Eimpunth S, Wanitphakdeedecha R. Efficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in Asians. J Am Acad Dermatol 2010;63:274-83.
[Google Scholar]
|
| 24. |
Hu S, Chen MC, Lee MC, Yang LC, Keoprasom N. Fractional resurfacing for the treatment of atrophic facial acne scars in Asian skin. Dermatol Surg 2009;35:826-32.
[Google Scholar]
|
| 25. |
Alster TS, Tanzi EL, Lazarus M. The use of fractional laser photothermolysis for the treatment of atrophic scars. Dermatol Surg 2007;33:295-9.
[Google Scholar]
|
| 26. |
Mahmoud BH, Srivastava D, Janiga JJ, Yang JJ, Lim HW, Ozog DM. Safety and efficacy of erbium-doped yttrium aluminum garnet fractionated laser for treatment of acne scars in type IV to VI skin. Dermatol Surg 2010;36:602-9.
[Google Scholar]
|
| 27. |
Hu S, Hsiao WC, Chen MC, Huang YL, Chang SL, Shih PY, et al. Ablative fractional erbium-doped yttrium aluminum garnet laser with coagulation mode for the treatment of atrophic acne scars in Asian skin. Dermatol Surg 2011;37:939-44.
[Google Scholar]
|
Fulltext Views
5,689
PDF downloads
1,252





