Translate this page into:
Efficacy of topical azelaic acid gel in the treatment of mild-moderate acne vulgaris
2 Department of Dermatology, Khoram Abad University of Medical Science, Khoram Abad, Iran
3 Skin Diseases and Leishmaniasis Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Correspondence Address:
Fariba Iraji
Department of Dermatology, Al-Zahra Hospital, P.O. Box: 892, Isfahan
Iran
| How to cite this article: Iraji F, Sadeghinia A, Shahmoradi Z, Siadat AH, Jooya A. Efficacy of topical azelaic acid gel in the treatment of mild-moderate acne vulgaris. Indian J Dermatol Venereol Leprol 2007;73:94-96 |
Abstract
Background: Twenty percent azelaic acid gel is recommended as a topical treatment for acne due to its favorable profile. Aim: Our objective in this study was to evaluate the efficacy of 20% azelaic acid gel in the treatment of mild to moderate acne vulgaris. Methods: This was a double blind, randomized clinical trial. Sixty patients with mild to moderate acne vulgaris were selected randomly to receive either azelaic acid gel or the vehicle gel alone. Patients were followed up every 15 days for a period of 45 days. The number of lesions and the acne severity index (ASI) were recorded and compared using Student's t-test. Results: Total lesion count was reduced by 60.6% and 19.9% by azelaic acid gel and the placebo respectively (P =0.002). ASI was reduced by 65.2% and 21.3% by azelaic acid gel and the placebo respectively (P =0.001), i.e., azelaic acid gel was 3.06 times more effective than the placebo in reducing ASI. Conclusion: Azelaic acid gel can be used as an effective treatment in mild to moderate acne vulgaris.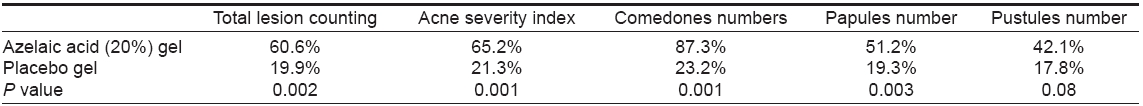
 |
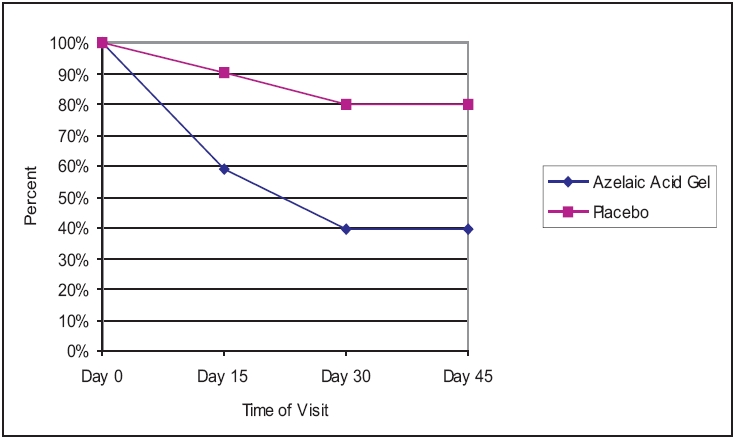
| Effi cacy of azelaic acid gel and placebo on acne severity index |
 |
| Effi cacy of azelaic acid gel and placebo on acne severity index |
 |
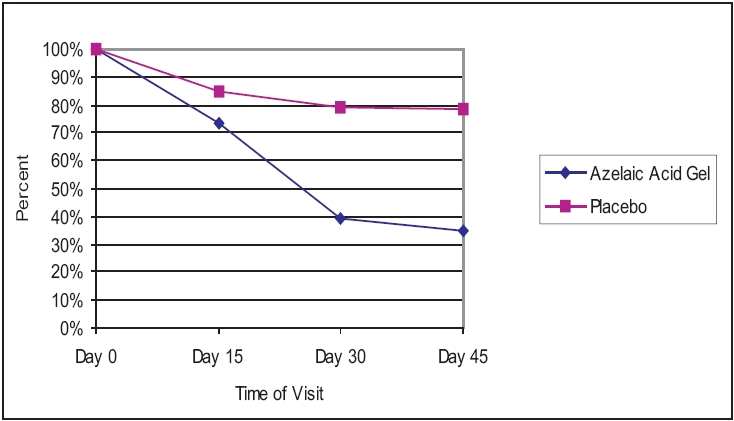
| Effi cacy of azelaic acid gel and placebo on total lesion counts |
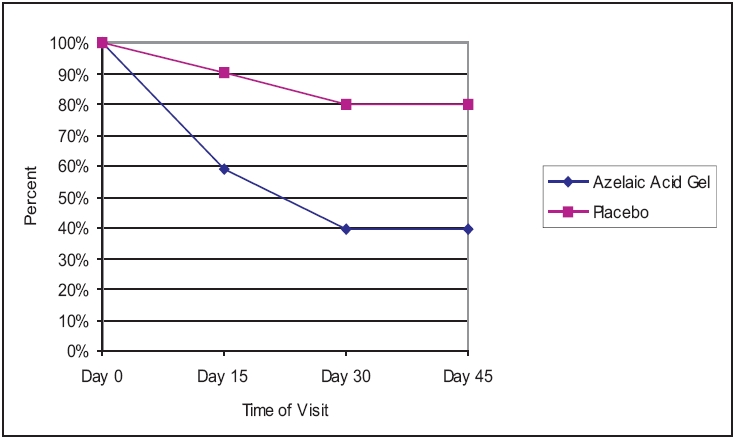 |
| Effi cacy of azelaic acid gel and placebo on total lesion counts |
INTRODUCTION
The etiopathogenesis of acne includes four primary processes: hyperkeratinization (plugging) of the pilosebaceous follicles, increased sebum levels, increased bacterial colonization with Propionibacterium acnes and inflammation. [1],[2] No single topical agent has yet been developed that addresses all of these factors. Hence, combination regimes that usually include an antibiotic and an agent to reduce follicular plugging have become the mainstay of treatment. [3]
Azelaic acid is a naturally occurring dicarboxylic acid analogue. [3] It is an extremely weak acid, much weaker than vinegar. It is found in some whole grains and in trace amounts in the human body, [4] its plasma levels normally ranging from 20-80 ng/ml. [4] Azelaic acid has in vitro antimycotic properties. [5] Azelaic acid (20%) cream is an anti-acne agent with antimicrobial and keratinization-normalizing properties. [6] Its antibiotic effects may be due to the inhibition of bacterial protein synthesis, [7] which is dose- and pH-dependent (it is more effective at low pH values). [8]
While 20% azelaic acid cream is effective as monotherapy in mild to moderate acne, [9] there were no controlled trials. Hence, we proceeded to evaluate the efficacy of 20% azelaic acid gel in comparison with the vehicle gel alone for the treatment of the mild to moderate acne vulgaris.
METHODS
Sixty patients in the age range of 15-35 years with mild to moderate acne were recruited in this 45-day trial. The Isfahan University of Medical Sciences Ethical Committee permission was obtained before performing the study. Informed consent was obtained from patients. Patients who had a background of drug sensitivity, hepatic or kidney disease, malnutrition, pregnancy or lactation were excluded from the study. All acne medications were stopped 6 weeks before the initiation of the study. During the initial visit, the patients were randomly assigned to one of the two treatment groups. Thirty patients were treated twice daily with topical azelaic acid gel (20%) and thirty controls with the vehicle gel, composed of carbapol 934 (1%), glycerin (5%) and triethanolamine (0.2-0.5%). Both physicians and patients were blinded to the type of treatment. All 60 patients completed the study.
The severity of acne on the face was graded according to the method of Burke and Cunliffe, [10] with the individual scores added up. Four sites on the face (chin, forehead and left and right cheeks) were graded. The mean value from this grading was used for further calculations. The same dermatologist counted the number of comedones, papules and pustules on the face at each visit. The total lesion count (TLC) was defined as the total number of comedones and inflammatory lesions. Acne on other parts of the body was not considered.
Response to therapy was measured by calculating the difference between the TLC and the acne severity index (ASI) at baseline and every 15 days in the 45-day trial. Acne severity index was calculated as:
ASI = Papules + (2 x pustules) + (0.25 x comedones)
The total number of lesions for each patient was considered to be 100% at the first visit. Any subsequent decrease in the number was calculated accordingly and regarded as the percentage of improvement. The mean of these improvement percentages was calculated for each group of patients and used for statistical analysis. At the end of the study, labels were decoded and the collected data was analyzed by using the SPSS program. For comparing the efficacy of these treatments, statistical Student′s t -test was used and P value < 0.05 was considered to be statistically significant.
RESULTS
The mean age of patients was 18.33 for the group treated with azelaic acid gel and 16.93 for the placebo group. Males accounted for 34 and 44% of patients in the azelaic acid and placebo groups, respectively. The results of treatment with azelaic acid gel and placebo gel are shown in [Table - 1]. As it can be seen in this Table, azelaic acid gel was 3.04 times more effective than placebo in the reduction of TLC. The reduction of TLC during the 6 weeks (45 days) course of treatment is shown in [Figure - 1]. In terms of ASI, azelaic acid gel was 3.06 times more effective than the placebo [Figure - 2]. Azelaic acid gel′s effect was greater than that of the placebo on all types of lesions. Compared to the placebo, it was more effective against non-inflammatory lesions (comedones) and less effective against inflammatory ones (papules and pustules).
Side effects occurred in approximately 3% of patients in the azelaic acid-treated group and mainly consisted of pruritus, burning, stinging and tingling. They were generally transient and mild in nature. Five patients who used azelaic acid gel noted that the growth of their coarse facial hair was also reduced.
DISCUSSION
Azelaic acid cream (20%) is useful in the treatment of mild to moderate acne, with an efficacy comparable to that of tretinoin (0.05%), benzoyl peroxide (5%) and topical erythromycin (2%). [11] It is as effective as oral tetracycline in the treatment of acne with the onset of action being 4 weeks after starting treatment. [4],[12] It may be favorably combined with minocycline and may help reduce recurrences following discontinuation of systemic therapy. Azelaic acid interferes with acne pathogenesis by virtue of its anti-keratinizing, antibacterial and antiinflammatory properties. [13],[14] It has a favorable safety profile; [15] it is not teratogenic, is not associated with systemic adverse events or photodynamic reactions. It also exhibits excellent local tolerability and does not induce resistance in P. acnes . [15]
Although the efficacy of azelaic acid cream in the treatment of mild-moderate acne vulgaris has been established, we did not find any controlled trial of the use of 20% azelaic acid gel for this indication in literature. Gollnick et al compared the efficacy of 15% azelaic acid gel with that of 5% benzoyl peroxide gel and 1% clindamycin gel applied twice daily for 4 months in two randomized, blinded comparative trials. Azelaic acid (15%) gel was as effective as 5% benzoyl peroxide gel and clindamycin, with a median reduction of 70 and 71% respectively of papules and pustules (both inflamed lesions). It was well tolerated; its side effects (local burning and irritation) being distinctly less but more pronounced than those of 5% benzoyl peroxide gel and clindamycin respectively. The efficacy of the 15% azelaic acid gel described by Gollnick et al was more than that observed in our study, probably because of the longer duration of treatment, 4 months as compared to our 6 weeks.
We found that a significant therapeutic improvement was seen after 6 weeks of treatment with 20% azelaic acid gel in patients with mild-moderate acne vulgaris and the side effects were minimal. It was most effective on the non-inflammatory lesions probably due its keratolytic effect. Some reduction of acne lesions due to the placebo gel was probably due to the alcohol content. The reduction of facial hair in some female patients was possibly due to the inhibition of the enzyme 5a-reductase. [16]
In summary, the results of this study suggest that topical 20% azelaic acid gel is effective for the treatment of mild to moderate acne vulgaris with few side effects.
| 1. |
Cunliffe W, Gollnick H. Acne. In: Ardnt KA, Leboit PE, Robinson JK, Wintroub BU, editors. Cutaneous medicine and surgery. 1 st ed. WB Saunders: Philadelphia; 1996. p. 461-80.
[Google Scholar]
|
| 2. |
Cunliffe WJ, Simpson NB. Disorders of the sebaceous glands. In: Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Textbook of dermatology. 6 th ed. Black Well Science: Oxford; 1998. p. 1955-60.
[Google Scholar]
|
| 3. |
Weiss JS. Current options for the topical treatment of acne vulgaris. Pediatr Dermatol 1997;14:480-8.
[Google Scholar]
|
| 4. |
Bonner MW, Benson P, James W. Topical antibiotics in dermatology. In: Freedberg IM, Elsen AZ, Wolf FK, Austin KF, Goldsmith LA, Katz ST, editors. Dermatology in general medicine. 5 th ed. McGraw-Hill: New York; 1999. p. 2733-4.
[Google Scholar]
|
| 5. |
Brash J, Christopher E. Azelaic acid has antimycotic properties in vitro . Dermatology 1993;186:55-8.
[Google Scholar]
|
| 6. |
Gibson JR. Azelaic acid 20% cream (AZELEX) and the medical management of acne vulgaris. Dermatol Nurs 1997;9:339-44.
[Google Scholar]
|
| 7. |
King K. The effect of Azelaic acid on cutaneous micro flora in vivo. J Invest Dermatol 1995;84:480.
[Google Scholar]
|
| 8. |
Holland KT, Bojar RA. Antimicrobial effects of Azelaic acid. J Dermatol Treatment 1993;4S8-11.
[Google Scholar]
|
| 9. |
Fitton A, Goa KL. Azelaic acid. A review of its pharmacological properties and therapeutic efficacy in acne and hyperpigmentary skin disorders. Drugs 1991;41:780-98.
[Google Scholar]
|
| 10. |
Burke BM, Cunliffe WJ. The assessment of acne vulgaris-the Leeds technique. Br J Dermatol 1984;111:83-92
[Google Scholar]
|
| 11. |
Gollnick H. Azelaic acid for keratinization disorders? Med Monatsschr Pharm 1991;14:370-1.
[Google Scholar]
|
| 12. |
Shemer A, Weiss G, Amichai B, Kaplan B, Trau H. Azelaic acid (20%) cream in the treatment of acne vulgaris. J Eur Acad Dermatol Venereol 2002;16:178-9.
[Google Scholar]
|
| 13. |
Gollnick HP, Graupe K, Zaumseil RP. Azelaic acid 15% gel in the treatment of acne vulgaris. Combined results of two double-blind clinical comparative studies. J Dtsch Dermatol Ges 2004;2:841-7.
[Google Scholar]
|
| 14. |
Spellman MC, Pincus SH. Efficacy and safety of azelaic acid and glycolic acid combination therapy compared with tretinoin therapy for acne. Clin Ther 1998;20:711-21.
[Google Scholar]
|
| 15. |
Graupe K, Cunliffe WJ, Gollnick HP, Zaumseil RP. Efficacy and safety of topical azelaic acid (20 percent cream): An overview of results from European clinical trials and experimental reports. Cutis 1996;57:20-35.
[Google Scholar]
|
| 16. |
Stamatiadis D, Bulteau-Portois MC, Mowszowicz I. Inhibition of 5 alpha-reductase activity in human skin by zinc and azelaic acid. Br J Dermatol 1988;119:627-32.
[Google Scholar]
|
Fulltext Views
15,146
PDF downloads
3,028





