Translate this page into:
Endonyx onychomycosis caused by Trichophyton tonsurans
2 Department of Medical Services, Institute of Dermatology, Ministry of Public Health, Bangkok, Thailand
Correspondence Address:
Penvadee Pattanaprichakul
Department of Dermatology, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Prannok Road, Bangkoknoi, Bangkok
Thailand
| How to cite this article: Bunyaratavej S, Bunyaratavej S, Muanprasart C, Matthapan L, Varothai S, Tangjaturonrusamee C, Pattanaprichakul P. Endonyx onychomycosis caused by Trichophyton tonsurans. Indian J Dermatol Venereol Leprol 2015;81:390-392 |
Sir,
Endonyx onychomycosis (EO) is an unusual variant of onychomycosis which involves the inner surface of nail plate without inflammation of the nail bed, onycholysis or subungual hyperkeratosis. Previously, it was considered a subtype of distal and lateral subungual onychomycosis (DLSO), as both originate from the distal part of the nail. However, their clinical manifestations, pathogenesis and etiologies were found to be different. Distal and lateral subungual onychomycosis usually manifests as an inflammation of the nail bed with onycholysis and subungual hyperkeratosis which are not found in endonyx onychomycosis. Moreover, the common pathogen of the former is Trichophyton rubrum, whereas in the latter Trichophyton soudanense and Trichophyton violaceum play an important role. We were unable to find any previous reports of, endonyx onychomycosis caused by Trichophyton tonsurans. [1],[2]
A 25-year-old woman presented with a 5-month history of whitish discoloration of the left third fingernail with pruritic skin rashes present around umbilicus, groin, right axilla and left dorsum of hand for 3 months. She had been applying an unknown, over-the-counter, topical antifungal medication on the rash and nail lesion with no significant improvement. She was previously healthy with no known underlying disease. None of her family members had a history of dermatophytosis. On physical examination, multiple, well-defined, scaly, annular, erythematous plaques were present on the right axilla, periumbilical area, groin and left hand were present. The left third fingernail plate revealed milky white transverse patches without changes of the nail surface [Figure - 1]. Onycholysis and subungual hyperkeratosis were not detected. The scalp including the remainder of her skin, fingernails and toenails were normal. Potassium hydroxide (10% KOH) examination of skin scrapings from the left third fingernail, right axilla, abdomen and dorsum of the left hand revealed branching septate fungal hyphae with arthrospores in all the specimens. Cultures on Sabouraud dextrose agar (SDA) (HiMedia Laboratories, Mumbai, India) from all the affected sites showed yellow-brown colonies with a suede-like surface, raised and folded center, and a flat periphery [Figure - 2]a. The reverse side of the culture plate showed reddish-brown to deep mahogany colored colonies. These colonies revealed decent growth on thiamine-enriched media and positive hydrolysis of urea at 5 days. In vitro hair perforation test was positive within 14 days. Microscopic findings showed relatively irregular, broad, septate hyphae with numerous club-shaped microconidia of varying sizes from long clavate to broad pyriform, generated at right angles to the hyphae. Numerous giant forms of microconidia and chlamydospore-like structures were also detected in this case [Figure - 2]b. Smooth-walled macroconidia containing two to four cells in each were sparsely detected and no spiral coils were identified.[Figure - 2]c. These overall findings were characteristic of T. tonsurans.[3],[4]
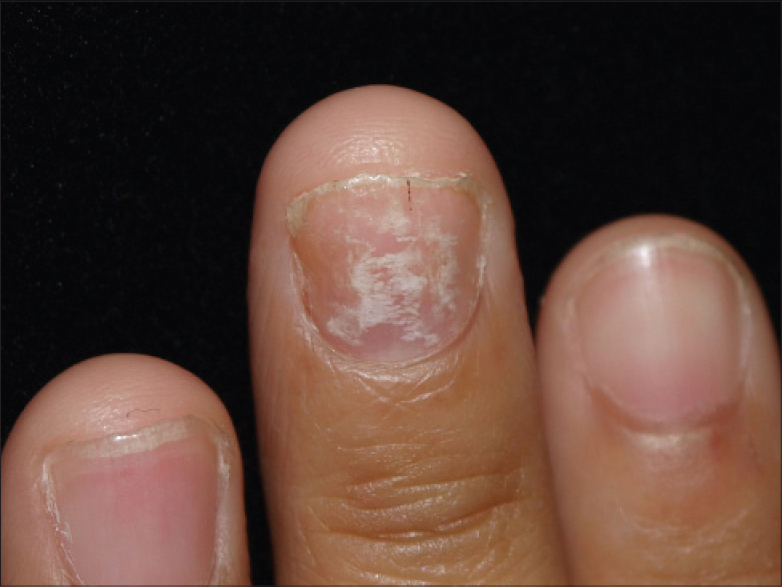 |
| Figure 1: Milky white discoloration of the nail plate without surface change in endonyx onychomycosis |
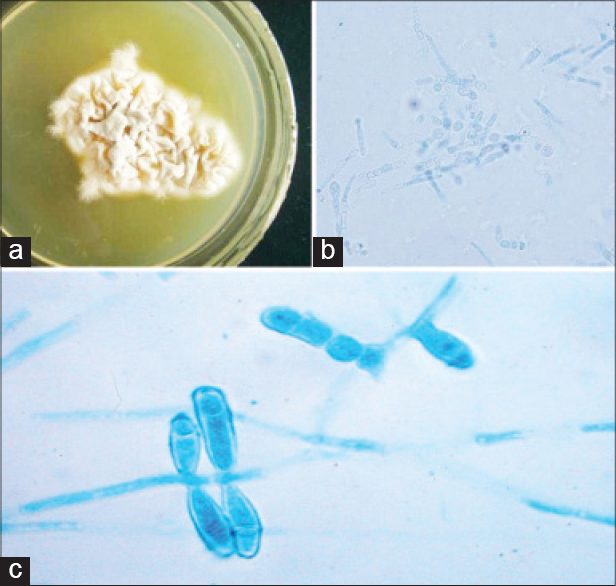 |
| Figure 2: (a) Fungal culture on SDA showed centrally folded, yellow-brown colored colonies with a suede-like surface and flattening periphery; (b) Numerous multiform microconidia and chlamydospore-like structures (The lactophenol cotton blue (LPCB) wet mount preparation, ×400); (c) Smooth-walled macroconidia of T. tonsurans are sparsely detected with short cigar-shaped appearance and variable sizes, attached perpendicular to the original septate hyphae (LPCB, ×1000) |
The patient was treated successfully with weekly oral fluconazole 200 mg for 8 months in combination with topical ketoconazole cream applied on the skin lesions for 4 weeks. The skin and nail lesions were completely cured. Follow-up microscopic examination and fungal culture from multiple sites were negative after the course of antifungal therapy.
Onychomycosis has been recently classified into five clinical presentations according to the modes of invasion: distal and lateral subungual onychomycosis, proximal subungual onychomycosis (PSO), superficial white onychomycosis (SWO), endonyx onychomycosis and mixed onychomycosis (total nail dystrophy, secondary onychomycosis and paronychia-associated onychomycosis). [5]
Recent literature classified endonyx as a distinct group of onychomycosis with a characteristic mechanism by which fungal elements reach the nail plate via the finger pulp and invade its superficial and deeper parts leading to lamellar splitting of the nail plate without causing onycholysis or subungual alteration. This unique mechanism of fungal invasion commonly occurs with dermatophytes that cause endothrix-type of tinea capitis especially, T. soudanense and T. violaceum. Although T. tonsurans has not been reported to cause endonyx onychomycosis, it has been documented to cause distal and lateral subungual onychomycosis and endothrix type of tinea capitis. Therefore, one may suspect invasion of the nail plate causing endonyx onychomycosis. Clinically, this condition is characterized by diffuse milky white discoloration of affected nail. In contrast to distal and lateral subungual onychomycosis, the affected nail in endonyx onychomycosis does not show clinical signs of inflammation in the nail bed, such as onycholysis and subungual hyperkeratosis. [2] In spite of the milky color, endonyx type can be differentiated from superficial white onychomycosis by the presence of normal surface of the nail plate.
Tosti et al. reported three cases of endonyx onychomycosis caused by T. soudanense. [2] Nail biopsy specimens showed extensive fungal invasion through the nail plate without inflammation of the nail bed. T. violaceum has also been reported to cause the same clinicopathological features. [6] Our case demonstrated the classic nail lesion of endonyx onychomycosis, showing milky white discoloration in the nail plate without nail surface change; therefore, superficial white onychomycosis was excluded. Unfortunately, the nail biopsy was not performed to demonstrate the histopathological change in this case; however, the positive fungal culture from the affected nail confirmed T. tonsurans. Previously, there were several studies of tinea capitis and tinea corporis caused by T. tonsurans and some reported cases of T. tonsurans-induced onychomycosis. [7] It is mostly observed in the patients with coexistent tinea capitis or contact history of asymptomatic carriers such as family members. In our patient, there were no scalp lesions and none of her family members had features of dermatomycosis.
| 1. |
Fletcher CL, Moore MK, Hay RJ. Endonyx onychomycosis due to Trichophyton soudanense in two Somalian siblings. Br J Dermatol 2001;145:687-8.
[Google Scholar]
|
| 2. |
Tosti A, Baran R, Piraccini BM, Panti PA. "Endonyx" onychomycosis: A new modality of nail invasion by dermatophytes. Acta Derm Venereol 1999;79:52-3.
[Google Scholar]
|
| 3. |
Ellis D. Identification of common dermatophytes. Mycology online. Available from: http://www.mycology.adelaide.edu.au. [Last accessed on 2014 Aug 24].
[Google Scholar]
|
| 4. |
Mochizuki T, Anzawa K, Sakata Y, Fujihiro M. Simple identification of Trichophyton tonsurans by chlamydospore-like structures produced in culture media. J Dermatol 2013;40:1027-32.
[Google Scholar]
|
| 5. |
Baran R, Hay RJ, Tosti A, Haneke E. A new classification of onychomycosis. Br J Dermatol 1998;139:567-71.
[Google Scholar]
|
| 6. |
Sagher F. Histologic examinations of fungous infections of the nails. J Invest Dermatol 1948;11:337-57.
[Google Scholar]
|
| 7. |
Bronson DM, Desai DR, Barsky S, Foley SM. An epidemic of infection with Trichophyton tonsurans revealed in a 20-year survey of fungal infections in Chicago. J Am Acad Dermatol 1983;8:322-30.
[Google Scholar]
|
Fulltext Views
11,267
PDF downloads
1,710





