Translate this page into:
Eosinophilic fasciitis associated with Raynaud's phenomenon, esophageal dysmotility, positive antinuclear antibody and anti-neutrophil cytoplasmic antibody
2 Department of Pathology, JIPMER, Puducherry, India
Correspondence Address:
Laxmisha Chandrashekar
Department of Dermatology, Venereology and Leprology, JIPMER, Puducherry - 605 006
India
| How to cite this article: Behera B, Singh N, Chandrashekar L, Sathya AB, Thappa DM, Toi PC. Eosinophilic fasciitis associated with Raynaud's phenomenon, esophageal dysmotility, positive antinuclear antibody and anti-neutrophil cytoplasmic antibody. Indian J Dermatol Venereol Leprol 2018;84:224-227 |
Sir,
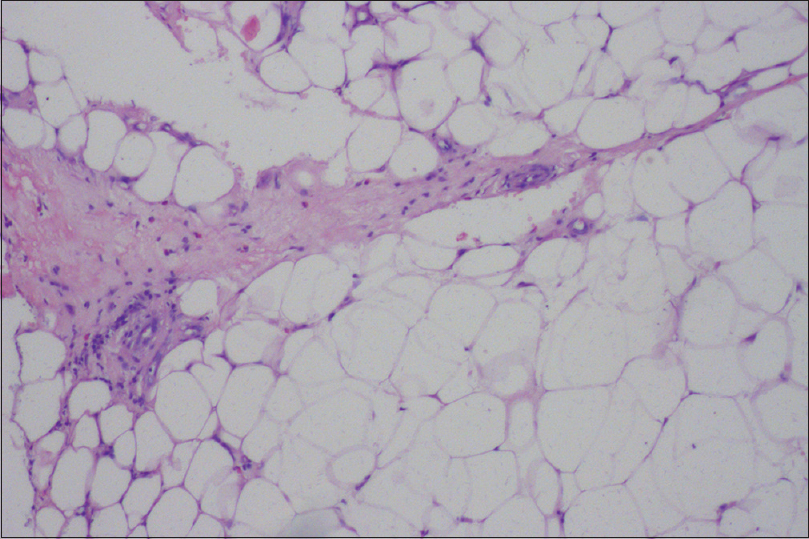
A 33-year-old female agricultural laborer of Tamil origin presented with diffuse painful swelling of both forearms and legs of 5 months duration. She had difficulty in full extension of the fingers, getting up from sitting position, and raising hands above the shoulder. There was a history of Raynaud's phenomenon and burning retrosternal pain. She gave a history of strenuous manual work before the onset of the disease. Clinical examination revealed diffuse pitting edema bilaterally over forearms, hands, and legs, along with tightening of the skin and finger contractures. There was thickening and induration of the skin without any peau d' orange appearance. The overlying skin was shiny, and “groove sign” was visible on bilateral forearms and legs which got accentuated on raising the limbs [Figure - 1]a and [Figure - 1]b. A positive Raynaud's phenomenon was demonstrated by cold stimulation test. There were no fingertip ulcers, telangiectasia, or any evidence of pigmentary change. General and systemic examinations were within normal limit without any muscle tenderness or evidence of synovitis, and with normal chest expansion and breath sounds. A differential diagnosis of eosinophilic fasciitis and systemic sclerosis was considered. Nail fold capillaroscopy was within normal limit. Patient's total leukocyte count was 13500 per mm [3] (34% eosinophil), and erythrocyte sedimentation was 50 mm at the 1st hour. Tested by immunofluorescence method, antinuclear antibody (ANA) was positive (4+ with centromere pattern). Cytoplasmic–anti-neutrophil cytoplasmic antibody (c-ANCA) was also positive. Esophageal scintigraphy demonstrated dysmotility in the lower third of the esophagus. Other investigations were within normal limits. A full thickness wedge skin biopsy revealed edema and thickening of subcutis and adjacent fascia along with moderate infiltration by lymphocytes, histiocytes, plasma cells, and eosinophil, which was consistent with the diagnosis of eosinophilic fasciitis [Figure - 2] and [Figure - 3]. The patient was put on 0.5 mg/kg prednisolone orally once daily. Due to poor response, oral methotrexate 15 mg weekly was added after 4 weeks. She reported symptomatic improvement in 3 months, following which prednisolone was gradually tapered and stopped by 6 months. At that time, she had mild skin induration over the extremities for which weekly 15 mg methotrexate was continued for next 3 months and stopped. The patient had completely recovered with disappearance of the skin thickening and absence of groove sign after 1-year post treatment follow-up.
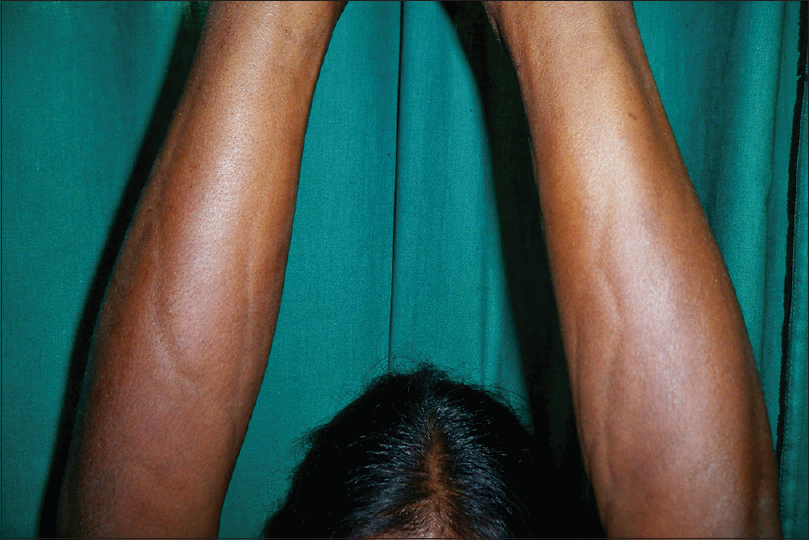 |
| Figure 1a: “Groove sign” seen over the forearms with shiny skin |
 |
| Figure 1b: “Groove sign” seen over the leg with shiny skin |
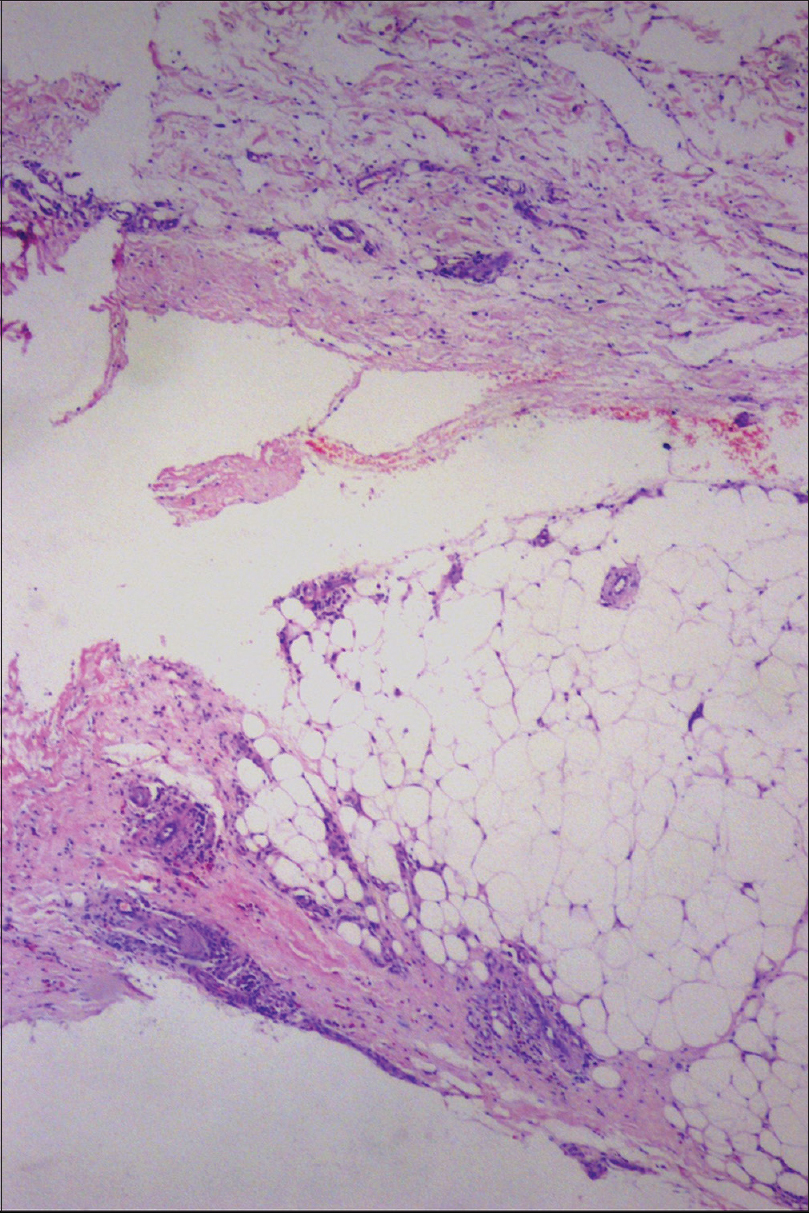 |
| Figure 2: Thickened and edematous fascia with infiltration of lymphocytes, plasma cells, and eosinophils (H and E, ×50) |
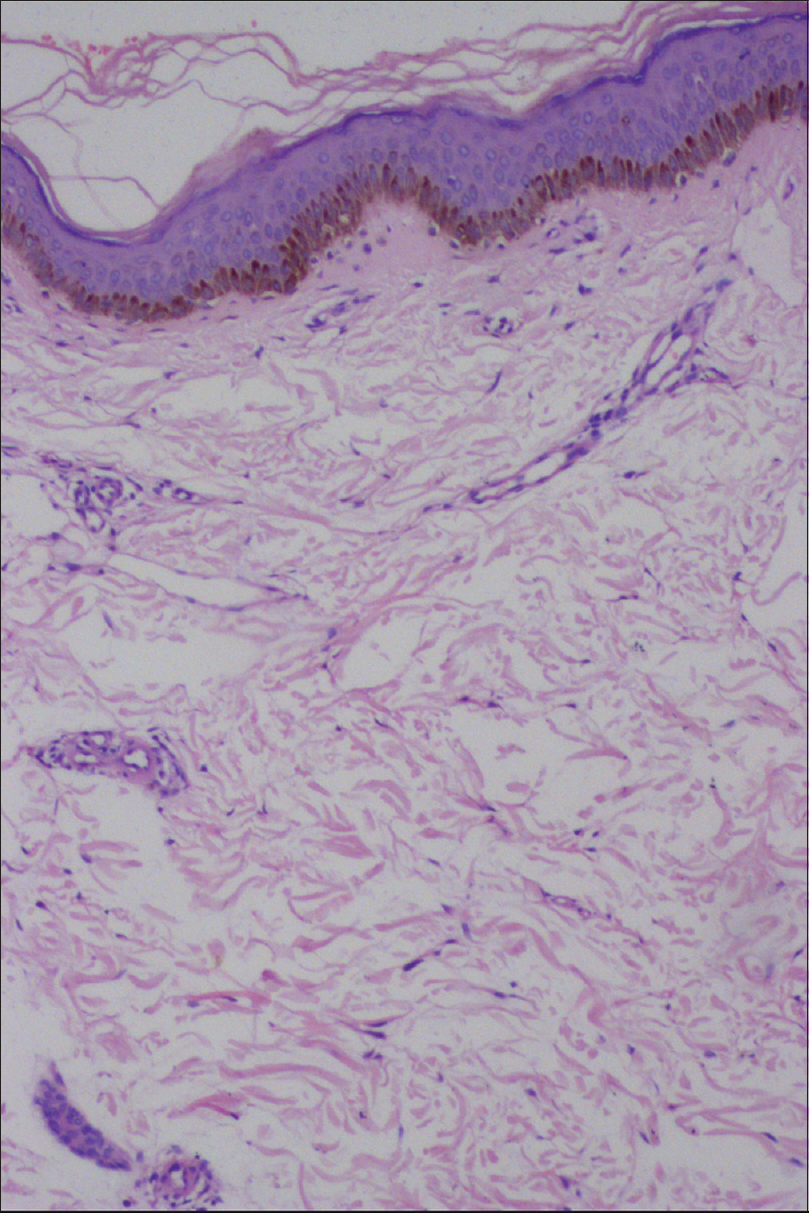 |
| Figure 3a: Epidermis and dermis looking apparently normal (H and E, ×100) |
 |
| Figure 3b: Thickened subcutaneous tissue septa showing eosinophilic infiltration (H and E, ×100) |
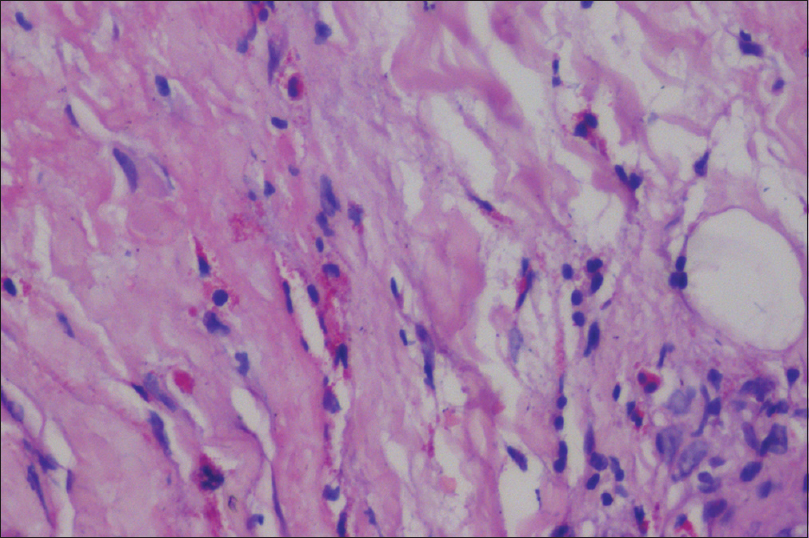 |
| Figure 3c: Thickened fascia showing infiltration by eosinophils (H and E, ×400) |
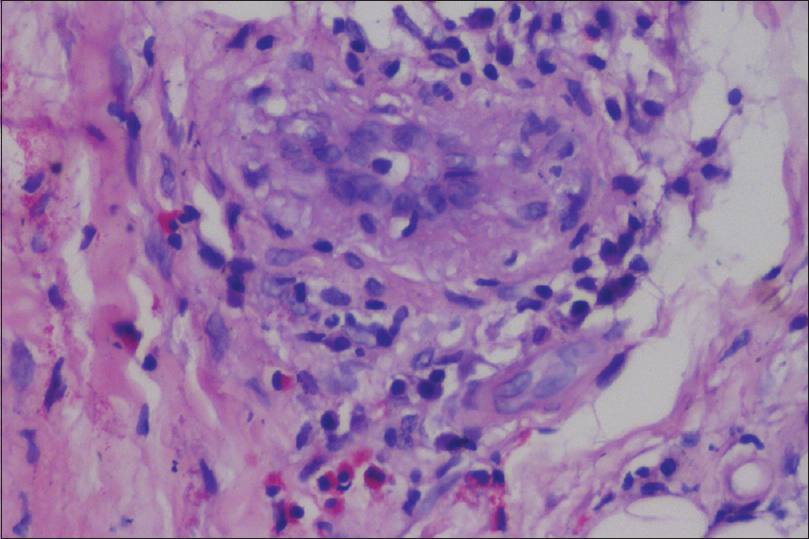 |
| Figure 3d: Perivascular infiltration of lymphocytes, plasma cells, and eosinophils in the fascia (H and E, ×400) |
Eosinophilic fasciitis or Shulman syndrome was first described in 1974.[1] Approximately 30–46% of the patients have a preceding history of trauma or physical exertion, as in our case.[2]
It is characterized by early edematous and erythematous extremities, followed by woody skin induration.[2] Sometimes the initial presentation can be bilateral pitting edema of extremities with nonspecific features such as fever, malaise, weakness, and weight loss.[3] Skin induration with a “peau d'orange” appearance and venous furrowing or “groove sign” or “river bed sign” can be demonstrated, as in our patient. Joint and muscle pain, joint contracture, as well as asthenia are frequent. Raynaud's phenomenon is unusual and involvement of internal organ is rare; however, our patient had Raynaud's phenomenon and esophageal dysmotility. A characteristic feature of eosinophilic fasciitis is peripheral eosinophilia, but it may be absent at the chronic stage or after treatment and is not essential for diagnosis.[2] ANA can be detected in low titers in 25% cases, and anti-neutrophil cytoplasmic antibody positivity has been described earlier in one case, but rheumatoid factor is usually negative.[1],[2] In our case, rheumatoid factor was negative, and both ANA and c-ANCA were positive.[1]
Various disorders that can mimic with eosinophilic fasciitis are eosinophilia-myalgia syndrome, idiopathic hypereosinophilic syndrome, systemic sclerosis, nephrogenic systemic fibrosis, morphea, scleredema of Buschke, carcinoid-associated scleroderma, and scleromyxedema.[1] In contrast to systemic sclerosis, a positive history of prior trauma or strenuous exercise, fascial thickening, peripheral and tissue eosinophilia, lack of internal organs involvement, negative nail fold capillaroscopy, and anti-topoisomerase antibody favors the diagnosis of eosinophilic fasciitis. The proposed criteria for the diagnosis of patients with eosinophilic fasciitis include two major criteria [symmetrical or nonsymmetrical swelling, induration, and thickening of skin and subcutaneous tissue that can be diffuse (extremities, trunk and abdomen) or localized (extremities) and thickened fascia with infiltration of lymphocytes and histiocytes with or without eosinophils] and five minor criteria (eosinophil count more than 0.5 × 109/L, hypergammaglobulinemia with gammaglobulin level more than 1.5 g/L, elevated muscle enzymes and/or aldolase levels, presence of groove sign and/or peau d'orange appearance, and hyperintense fascia on magnetic resonance T2-weighted images). Presence of two major criteria or one major and two minor criteria in the absence of features of systemic sclerosis is required for the diagnosis of eosinophilic fasciitis. Morphea-like lesions have been described in association with eosinophilic fasciitis in 25–30% of the cases. These patients need long-term follow-up as they can develop generalized morphea and systemic sclerosis in future.[4]
Systemic corticosteroids given in moderate-to-high doses early in the course of the disease can induce a complete remission in one-third of the cases.[1] Methotrexate in a dose of 15–25 mg once weekly is probably the most favored second line treatment, especially in patients with morphea-like skin lesions.[1] In a French cohort, 69% patients showed remission following methotrexate therapy.[5] In a study, about 60% of the patient had complete remission following methotrexate therapy; although 70% had a recurrence, all patients responded well to re-treatment with methotrexate.[6] In contrast to the prior report of relapse of eosinophilic fasciitis while on methotrexate in a c-ANCA positive patient,[1] our patient responded well to the combination of prednisolone and methotrexate and had not relapsed 9 months after cessation of therapy. Physical therapy is also extremely important as it improves joint and myofascial mobility and prevents joint contractures.[7] We are reporting this case of eosinophilic fasciitis to share its rare association with Raynaud's phenomenon, esophageal dysmotility, c-ANCA positivity and its favorable response to the combination of prednisolone and methotrexate.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Haiduc VF, Erkan D, Kirou K, Birchansky S, Park J, Danon MJ, et al. Anti-neutrophil cytoplasmic antibody (c-ANCA) positive recurrent eosinophilic fasciitis responsive to cyclophosphamide: a clinical pathology conference held by the division of rheumatology at hospital for special surgery. HSS J 2008;4:81-6.
[Google Scholar]
|
| 2. |
Pinal-Fernandez I, Selva-O' Callaghan A, Grau JM. Diagnosis and classification of eosinophilic fasciitis. Autoimmun Rev 2014;13:379-82.
[Google Scholar]
|
| 3. |
Lee HS, Chang SJ, Kang MS, Yoon CS, Kim KW, Sohn MH, et al. A case of eosinophilic fasciitis presenting as pitting edema of the lower extremities. Allergy Asthma Immunol Res 2014;6:179-82.
[Google Scholar]
|
| 4. |
Vasani RJ, Medhekar SV. Generalized morphea developing in a patient previously affected with eosinophilic fasciitis. Indian J Dermatol Venereol Leprol 2012;78:654-6.
[Google Scholar]
|
| 5. |
Lebeaux D, Francès C, Barete S, Wechsler B, Dubourg O, Renoux J, et al. Eosinophilic fasciitis (Shulman disease): new insights into the therapeutic management from a series of 34 patients. Rheumatology (Oxford) 2012;51:557-61.
[Google Scholar]
|
| 6. |
Berianu F, Cohen MD, Abril A, Ginsburg WW. Eosinophilic fasciitis: clinical characteristics and response to methotrexate. Int J Rheum Dis 2015;18:91-8.
[Google Scholar]
|
| 7. |
Lakhanpal S, Ginsburg WW, Michet CJ, Doyle JA, Moore SB. Eosinophilic fasciitis: clinical spectrum and therapeutic response in 52 cases. Semin Arthritis Rheum 1988;17:221-31.
[Google Scholar]
|
Fulltext Views
3,563
PDF downloads
1,748





