Translate this page into:
Epidermal inclusion cyst or giant milium of the nipple
2 Department of Pathology, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India
Correspondence Address:
Rashmi Sarkar
Department of Dermatology, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi - 110 002
India
| How to cite this article: Jain S, Sarkar R, Garg VK, Khurana N. Epidermal inclusion cyst or giant milium of the nipple. Indian J Dermatol Venereol Leprol 2012;78:103-105 |
Sir,
Epidermal inclusion cysts (EICs) are the common keratin-containing benign cysts lined by the epidermis. They arise from sequestered epidermal cells in the dermis, either congenitally or from traumatic implantation. Post-traumatic EICs are rare and are found mainly on the fingers, toes, palms, and soles, the frequently traumatized sites of the body. [1] Breast is an uncommon site for post-traumatic EIC, and only few cases have been reported to develop following the penetrating injuries in adult patients. [2],[3] Here, we report a case of EIC arising from nipple in a child following blunt trauma.
A 15-month-old girl presented with a painless, white, soft tissue growth from the right nipple for the past 2 months. To begin with, the lesion was lentil sized and continued to enlarge gradually until her presentation. The gradual increase in the size was the only concern of the mother. She did not report any discomfort, itching, or discharge from the growth. There was no history of similar complaints in the left breast. Mother did not give history of any kind of trauma to the breast prior to the onset of the growth. However, on detailed questioning, the mother informed that she used to squeeze the breast of child during the neonatal period to express the witch′s milk.
General physical examination was unremarkable. Cutaneous examination revealed a single well-circumscribed, pearly white, dome-shaped lesion measuring about 0.8 x 0.8 cm arising from the right nipple. The surface of the lesion appeared smooth with no umbilication [Figure - 1]. On palpation, the lesion was soft, cystic, and non-tender. There was no underlying mass in the breast tissue. The contour of the areola was maintained. The left breast was completely normal. An EIC or giant milium was suspected on the basis of clinical findings. Cyst was excised under local anesthesia with complete cosmetic recovery and the specimen was sent for histopathological examination. Sectioning revealed a cystic structure containing soft foul-smelling cheesy material. Microscopic examination showed a cyst lined by stratified squamous epithelium with lamellated keratinous material in the lumen with no adnexal structure [Figure - 2] and [Figure - 3]. A final diagnosis of EIC was made on the basis of relatively large size (8 mm) and soft consistency of the lesion containing cheesy material with corroborative histopathological finding.
 |
| Figure 1: Well-defined, pearly white, dome-shaped cystic lesion arising from the right nipple |
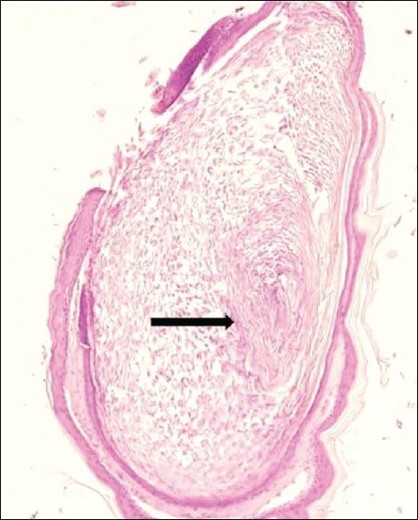 |
| Figure 2: Histological section shows the cyst containing keratinous material arranged in laminated layers (black arrow) and is lined by stratified squamous epithelium (H and E, ×100) |
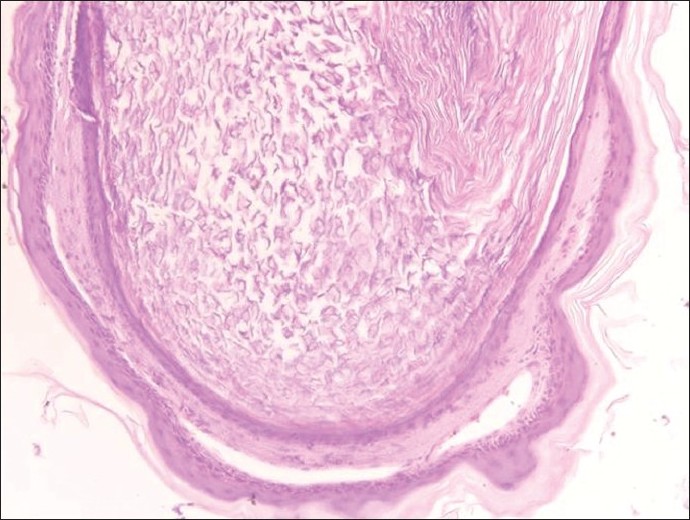 |
| Figure 3: Higher magnification showing that the cyst wall is composed of several layers of stratified squamous epithelium including the granular layer (H and E, ×250) |
EICs are the benign keratinous cysts. They present as a smooth, soft to firm, flesh-colored, freely movable, dome-shaped dermal or subcutaneous lesion. Cysts near the surface, as in ear lobe or scrotum, appear yellowish or white. They vary in size from a few millimeters to 5 cm. Histologically, they are indistinguishable from milia, being lined by stratified squamous epithelium several layers thick with a granular cell layer and contain concentric lamellae of keratin. However, EIC do have several clinical features that differ slightly from milium. Milia are superficial, firm, pearly white, dome-shaped lesions, rarely more than 1 to 2 mm in diameter. On incision and evacuation, milium reveals typical round keratinous content, while EIC shows soft cheesy keratinous material. Thus, relatively large size, soft consistency, foul smelling cheesy keratinous contents on sectioning, and gradual continued slow growth may be helpful findings to differentiate EIC from milium. Although four pediatric cases of primary milium of the areola have been reported in the literature, [4],[5] we consider that our patient had EIC as the lesion was large (8 mm), soft, cystic containing cheesy contents.
On reviewing the literature, most cases of the implantation cyst have occurred following the penetrating injuries or surgery; only in few instances, blunt trauma is held responsible. [2],[3] In our case, the cyst developed following a blunt trauma to the breast, nature of blunt trauma (mechanical trauma due to squeezing of the breast) sustained by our patient is uncommon, and has not been described earlier in the literature. The time period between trauma and appearance of cyst may vary from a few months to as long as 22 years. [6] In our case, the cyst developed about one year following the blunt trauma.
Although a few cases of post-traumatic EIC of the breast have been described in the literature, all of them are reported in adult patients following penetrating injuries such as reduction mammoplasty, needle aspiration biopsy, etc. To the best of our knowledge, ours is the first case of EIC arising from the nipple following the blunt trauma in a child. It is also to emphasize that both EIC and giant milium should be considered in the differential diagnosis on coming across a painless white lesion on the areola in a child.
| 1. |
Epstein WL, Kligman AM. Epithelial cysts in buried human skin. Arch Derm 1957;76:437-45.
[Google Scholar]
|
| 2. |
Fajardo LL, Bessen SC. Epidermal inclusion cyst after reduction mammoplasty. Radiology 1993;186:103-6.
[Google Scholar]
|
| 3. |
Davies JD, Nonni A, D'Costa HF. Mammary epidermoid inclusion cysts after wide-core needle biopsies. Histopathology 1997;31:549-51.
[Google Scholar]
|
| 4. |
Berk DR, Bayliss SJ. Milium of the areola: A novel regional variant of primary milia. Pediatr Dermatol 2009;26:485-6.
[Google Scholar]
|
| 5. |
Mishra DK, Singh AK. Persistent congenital milia with naevus spilus. Indian J Dermatol Venereol Leprol 1995;61:356.
[Google Scholar]
|
| 6. |
Shetty CM, Rai PK, Jain VK. Post traumatic epidermoid inclusion cyst of the orbit. Indian J Radiol Imaging 2006;16:135-7.
[Google Scholar]
|
Fulltext Views
22,827
PDF downloads
5,167





