Translate this page into:
Epidermal nevus syndrome associated with unusual neurological, ocular, and skeletal features
2 Department of Ophthalmology, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, Delhi, India
3 Department of Pathology, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, Delhi, India
Correspondence Address:
Archana Singal
B-14, Law Apartments, Karkardooma, Delhi-110092
India
| How to cite this article: Sharma R, Singal A, Verma P, Rohatgi J, Sharma S. Epidermal nevus syndrome associated with unusual neurological, ocular, and skeletal features. Indian J Dermatol Venereol Leprol 2012;78:480-483 |
Abstract
Epidermal nevus syndrome (ENS) is a rare disease, the pathogenesis of which is largely elusive. We, hereby, report an exclusive case of a 20-year-old man with verrucous ENS presented with dark colored papules and plaques along the Blaschko's lines present over the head and neck area along with fleshy growth in both eyes since birth. Limb length discrepancy and kyphoscoliosis were remarkable. Skin biopsy was compatible with verrucous epidermal nevus while the biopsy of the ocular lesion confirmed complex choristoma. MRI brain revealed calcification in the right temporal lobe. Bilateral arachnoid cyst in the middle cranial fossa, scleral osteoma in the posterior part of the right eyeball, and deformed calvarium were evident on CECT skull and orbit. The present illustration emphasizes the importance of a punctilious work up of the case.Introduction
Epidermal nevus syndrome (ENS), the Solomon syndrome, is a congenital syndrome characterized by the presence of epidermal nevi in association with various developmental abnormalities of the skin, eye, nervous, skeletal, cardiovascular, and urogenital systems. [1] Complex ocular choristomas (epibulbar tumors), characterized by the presence of two or more ectopic tissues, have been described occasionally in association with sebaceous ENS. [2] Unilateral arachnoid cyst, scleral osteoma, intracranial calcification, and calvarial deformity have been rarely described previously in association with sebaceous nevus syndrome. However, to the best of our knowledge, certain unusual skeletal and neurological features present in our case such as bilateral involvement of arachnoid cyst and temporal lobe calcification in association with verrucous ENS have not been reported previously.
Case Report
A 20-year-old man presented to the dermatology outpatient department with complaints of dark-colored raised lesions over head and neck area along with fleshy growth in both eyes since birth. There was history of progressive diminution of vision along with generalized tonic-clonic seizures since early childhood. He was well controlled on anti-epileptics. There was no evidence of mental retardation in the patient. Consanguinity among the parents was denied.
Examination revealed a moderately built man with kyphoscoliosis and lengthening of the right lower limb. Review of the systems was negative. Dermatological examination revealed erythematous to hyperpigmented verrucous plaques arranged along the lines of Blaschko with areas of alopecia over the bilateral temporal aspect of scalp extending anteriorly to involve the forehead and lateral aspect of cheek and posteriorly to involve the nape of the neck [Figure - 1].
 |
| Figure 1: Verrucous epidermal nevus with bilateral complex ocular choristomas |
Examination of right eye revealed firm erythematous multinodular subconjunctival mass in the superior part of eye ball encroaching on superior limbus and cornea. The left eye had a widened aperture along with large nodular subconjunctival mass on the left supero-temporal and temporal aspect encroaching two-thirds of cornea. Rest of the cornea and pupil were normal. Visual acuity was 6/60 improving to 6/18 with pinhole in the right eye and finger counting at 1.5 m in the left eye. Fundus examination of the right eye was conspicuous by the presence of a large optic disk along with partial coloboma in the right eye. Left fundus was normal.
Histopathology of the skin revealed hyperkeratosis, papillomatosis, and irregular acanthosis consistent with verrucous epidermal nevus [Figure - 2]. Microscopic examination of the sections of an incisional biopsy of the ocular lesion depicted stroma composed of dense connective tissue within which were lobules of the lacrimal gland, mature adipose tissue, and cartilage compatible with complex ocular choristoma [Figure - 3]. Calcification suggestive of osteoma in the supero-posterior coat of the right eyeball along with a bilateral arachnoid cyst in middle cranial fossa was evident on contrast-enhanced computed tomography (CECT) of the orbit [Figure - 4]. MRI brain revealed evidence of nodular hypointense focus on all pulse sequences in the right postero-medial temporal lobe with no perifocal edema/gliosis, suggestive of calcification. Bony calvarium appeared mildly deformed [Figure - 5]. X-ray dorso-lumbar spine depicted kyphoscoliosis. Rest of the investigations including hematological, biochemical including serum calcium and phosphorus, were within normal limits. Based on the aforesaid examination findings and investigations, a diagnosis of verrucous ENS was made, with bilateral complex ocular choristoma, osteoma in the posterior part of the right eyeball, deformed calvarium, kyphoscoliosis, right lower limb lengthening along with calcification in the temporal lobe of brain, and bilateral arachnoid cyst in middle cranial fossa.
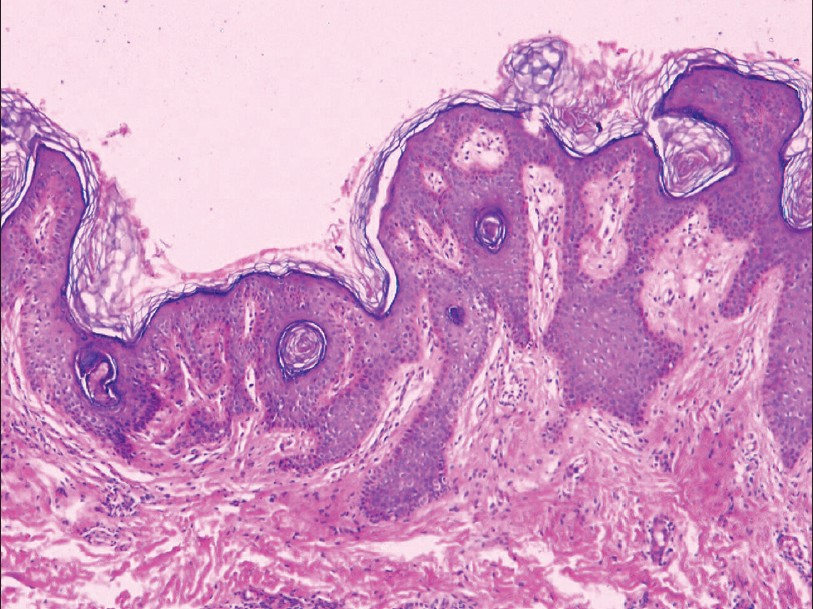 |
| Figure 2: Section from a cutaneous lesion depicting hyperkeratosis, irregular acanthosis, and papillomatosis (H and E, ×400) |
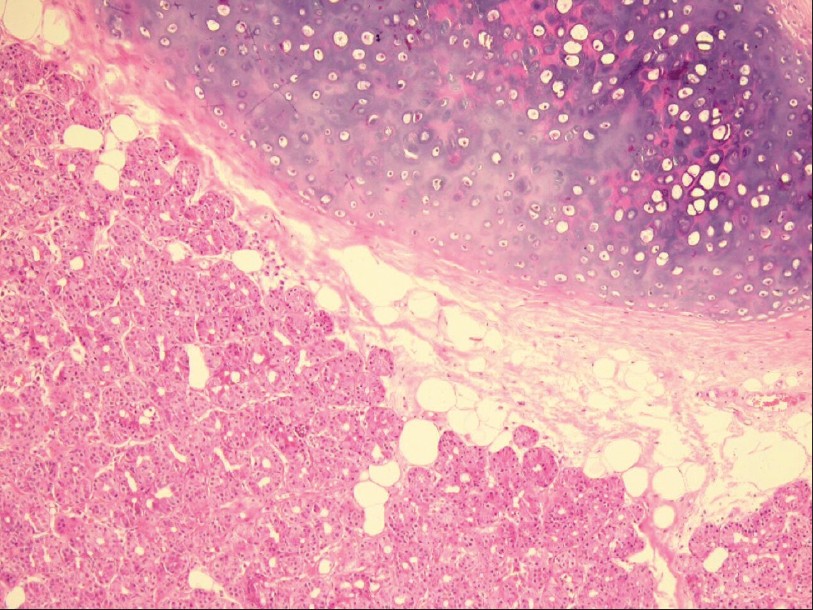 |
| Figure 3: Complex choristoma showing lacrimal tissue, mature adipose tissue, and hyaline cartilage (H and E, ×400) |
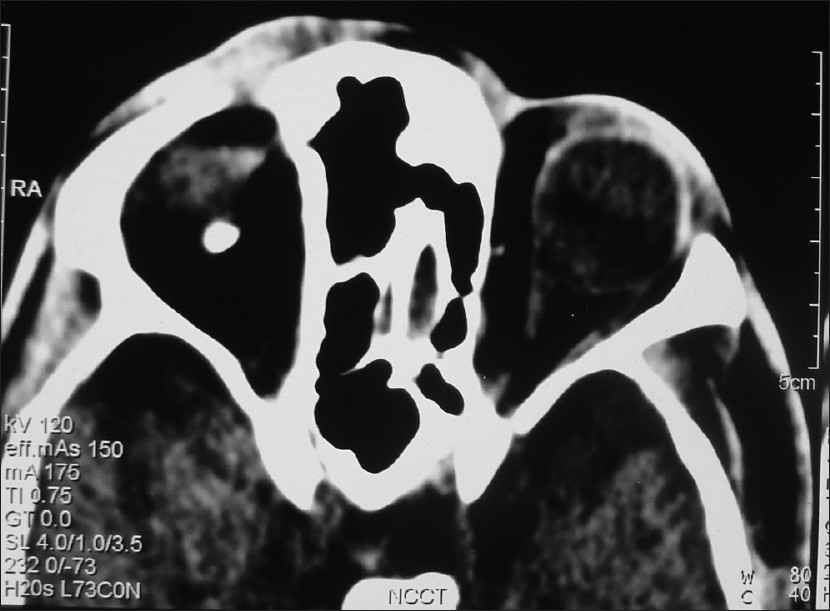 |
| Figure 4: CECT orbit showing osteoma in the supero-posterior coat of the right eyeball and bilateral arachnoid cyst |
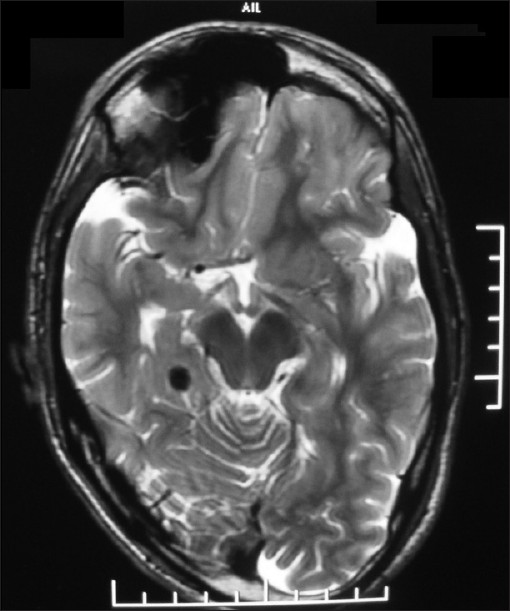 |
| Figure 5: MRI brain showing nodular hypointense focus in the right posteromedial temporal lobe with no perifocal edema/gliosis suggestive of calcification and mildly deformed calvarium |
Discussion
ENS denotes the presence of epidermal nevi (nevus sebaceous, verrucous epidermal nevus, inflammatory verrucous epidermal nevus, nevus comedonicus) in association with various developmental abnormalities of the skin, eye, nervous, skeletal, cardiovascular, and urogenital systems. [1] Ocular abnormalities have been described in as many as 50% of the patients with ENS and include choristomas, epibulbar dermoids, and coloboma of the uvea, optic disk, and lids. Choristomas represent congenital overgrowth of normal tissue in an abnormal location. Histologically, they may be divided into dermoids, lipodermoids, and simple and complex choristomas. [2] Simple choristomas have ectopic tissue of only one type (dermis-like tissue, lacrimal gland, bone, etc.), while complex choristomas have ectopic tissue of ectodermal and mesodermal origin, and may be comprised of lacrimal gland, bone, cartilage, adipose tissue, neural tissue, and/or smooth muscle interspersed in dermis-like connective tissue. Unilateral complex choristomas are relatively more common. To the best of our knowledge, there are only five reports of bilateral complex ocular choristoma occurring in association with linear nevus sebaceous syndrome (LNSS). [1],[2],[3],[4] In a meticulous English literature search, the occurrence of choristoma in association with verrucous epidermal nevus could not be found. In addition, the occurrence of sclera osteoma in association with ENS is sparingly described. [1],[2],[5]
Unilateral arachnoid cyst in the middle cranial fossa has been reported infrequently in ENSs. [6],[7],[8] Of these three cases, one has been reported in association with phacomatosis pigmentokeratotica while the remaining two with sebaceous nevi. Holden et al. [6] reported an arachnoid cyst on examination of biopsy material while others demonstrated this finding on imaging. [7],[8] Interestingly, arachnoid cyst in the present case was bilateral and its association with verrucous epidermal nevus has not been reported previously. Skeletal manifestations in ENS are often hemicorporeal and may either be primary or secondary. Skull asymmetry (deformed bony calvarium), a rare primay change, [9],[10] was evident in the present case. Intracerebral calcification in ENS has scarcely been documented in the literature. [11],[12],[13]
It is worthwhile at this point in time to recapitulate the pathogenesis of ENS. Endeavor to comprehend the pathogenesis of ENS by taking clues from bony defects has been made. Focal skeletal disease may be a source of fibroblast growth factor (FGF)-23, a possible pathogenic factor, in ENS. [14] FGF receptor (FGFR)-3 is involved in the development of the central nervous system. A widespread mosaicism of the FGFR3 mutation was suggested in a 5-year-old girl with a mosaic phenotype of ENS. [15] A case of discordant monozygotic (MZ) twins with severe ENS, supporting the concept of a postzygotic mutation, is on record. [16] Henceforth, activating FGFR3 mutations in the human epidermis, secondary to a postzygotic mutation in early embryonic development, may be the key event in the pathogenesis of ENS and needs further exploration.
The present case report has several unusual interesting components of ENS namely bilateral complex ocular choristoma, osteoma in the posterior part of the right eyeball, deformed calvarium, and temporal lobe calcification. The occurrence of bilateral involvement of arachnoid cyst in the middle cranial fossa in association with ENS is being reported for the first time.
Acknowledgements
The author would like to thank the patient for providing consent to use his photograph in this article.
| 1. |
Mansour AM, Laibson PD, Reinecke RD, Henkind P, Mikati M. Bilateral total corneal and conjunctival choristomas associated with epidermal nevus. Arch Ophthalmol 1986;104:245-8.
[Google Scholar]
|
| 2. |
Singal A, Dhaliwal U, Bhattacharya SN, Rohatgi J, Singh N. Complex ocular choristomas in linear nevus sebaceous syndrome: A case report of two cases. J Dermatol 2001;28:259- 64.
[Google Scholar]
|
| 3. |
Monahan RH, Hill CW, Venters HD. Multiple choristomas, convulsions and mental retardation as a new neuro-cutaneous syndrome. Am J Ophthalmol 1967;64:529-32.
[Google Scholar]
|
| 4. |
Duncan JL, Golabi M, Fredrick DR, Hoyt CS, Hwang DG, Kramer SG, et al. Complex limbal choristomas in linear sebaceous syndrome. Ophthalmology 1998;105:1459-65.
[Google Scholar]
|
| 5. |
Wilkes SR, Campbell RJ, Waller RR. Ocular malformation in association with ipsilateral facial nevus of Jadassohn. Am J Ophthalmol 1981;92:344-52.
[Google Scholar]
|
| 6. |
Holden KR, Dekaban AS. Neurological involvement in nevus lateris and nevus linearis sebaceous. Neurology 1972;22:879- 87.
[Google Scholar]
|
| 7. |
Prayson RA, Kotagal P, Wyllie E, Bingaman W. Linear epidermal nevus and nevus sebaceous syndromes: A clinicopathological study of 3 patients. Arch Pathol Lab Med 1999;123:301-5.
[Google Scholar]
|
| 8. |
Okada E, Tamura A, Ishikawa O. Phacomatosis pigmentokeratotica complicated with juvenile onset hypertension. Acta Derm Venereol 2004;84:397-8.
[Google Scholar]
|
| 9. |
Solomon LM. Epidermal nevus syndrome. Mod Probl Paediatr 1975;17:27-30.
[Google Scholar]
|
| 10. |
Lansky LL, Funderburk S, Cuppage FE, Schimke RN, Diehl AM. Linear sebaceous nevus syndrome. A hamartoma variant. Am J Dis Child 1972;123:587-90.
[Google Scholar]
|
| 11. |
Küçüködük S, Ozsan H, Turanli AY, Dinç H, Selçuk M. A new neurocutaneous syndrome: Nevus sebaceus syndrome. Cutis 1993;51:437-41.
[Google Scholar]
|
| 12. |
Lazzeri S, Mascalchi M, Cellerini M, Martinetti MG, Dal Pozzo G. Epidermal nevus syndrome: MR of intracranial involvement. AJNR Am J Neuroradiol 1993;14:1255-7.
[Google Scholar]
|
| 13. |
David P, Elia M, Garcovich A, Colosimo C Jr, Tagliaferri G, Macchi G. A case of epidermal nevus syndrome with carotid malformation. Ital J Neurol Sci 1990;11:293-6.
[Google Scholar]
|
| 14. |
Heike CL, Cunningham ML, Steiner RD, Wenkert D, Hornung RL, Gruss JS, et al. Skeletal changes in epidermal nevus syndrome: Does focal bone disease harbor clues concerning pathogenesis? Am J Med Genet A 2005;139A:67-77.
[Google Scholar]
|
| 15. |
García-Vargas A, Hafner C, Pérez-Rodríguez AG, Rodríguez- Rojas LX, González-Esqueda P, Stoehr R, et al. An epidermal nevus syndrome with cerebral involvement caused by a mosaic FGFR3 mutation. Am J Med Genet A 2008;146A:2275-9.
[Google Scholar]
|
| 16. |
Rijntjes-Jacobs EG, Lopriore E, Steggerda SJ, Kant SG, Walther FJ. Discordance for Schimmelpenning-Feuerstein-Mims syndrome in monochorionic twins supports the concept of a postzygotic mutation. Am J Med Genet A 2010;152A:2816- 9.
[Google Scholar]
|
Fulltext Views
6,804
PDF downloads
1,859





