Translate this page into:
Epidermolytic hyperkeratosis with rickets
2 Departments of Pathology, M.K.C.G. Medical College, Berhampur, Orissa, India
3 Departments of Plastic Surgery, M.K.C.G. Medical College, Berhampur, Orissa, India
Correspondence Address:
Surajit Nayak
Lane 3, Gajapati Nagar, Berhampur 760 004, Orissa
India
| How to cite this article: Nayak S, Behera SK, Acharjya B, Sahu A, Mishra D. Epidermolytic hyperkeratosis with rickets. Indian J Dermatol Venereol Leprol 2006;72:139-142 |
Abstract
A 6-year-old child presented with generalized hyperkeratosis, most marked over the flexures; windswept deformity of the legs; and limping since 3 years. On the basis of the clinical, histopathologic and biochemical findings, he was diagnosed as a case of epidermolytic hyperkeratosis with rickets. He was treated with parenteral vitamin D3 and calcium supplements orally. Nutritional rickets has been reported in children with various types of ichthyosis like lamellar and X-linked types. We report this case of epidermolytic hyperkeratosis with rickets for its rarity.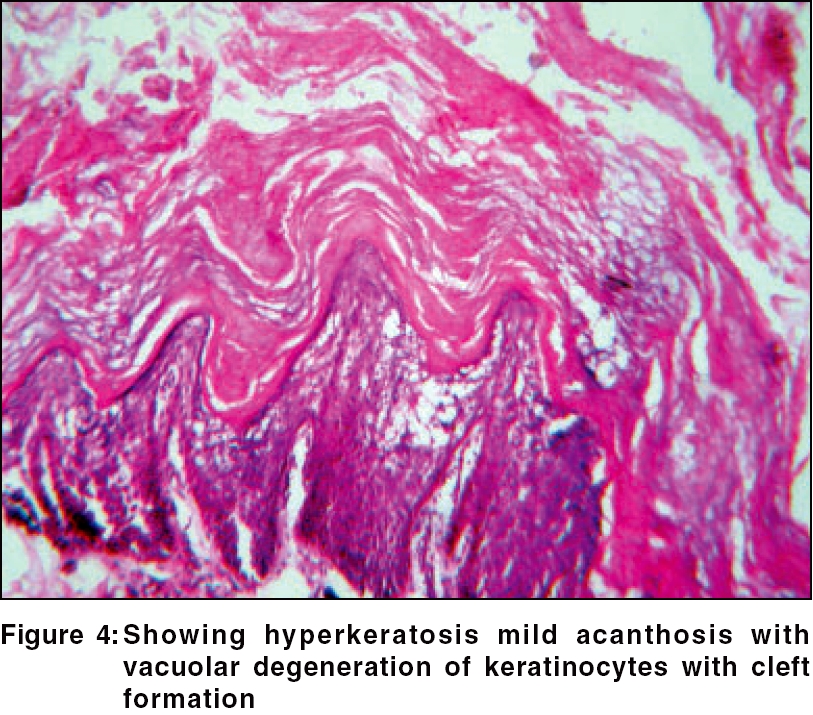 |
 |
 |
 |
 |
 |
 |
 |
Introduction
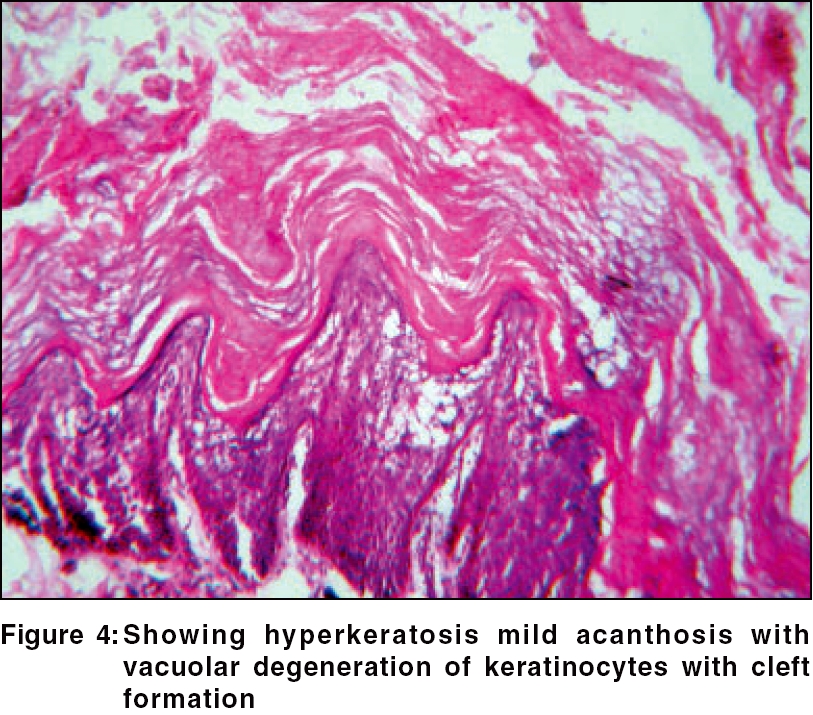
Epidermolytic hyperkeratosis (EHK), also knows as bullous congenital ichthyosiform erythroderma, is an autosomal dominant trait with a prevalence of approximately 1 in 200,000 to 300,000 persons. The disease is named for the distinctive histopathologic feature of vacuolar degeneration and associated hyperkeratosis of the epidermis. It usually presents at birth with blistering and redness. Although many cases of epidermolytic hyperkeratosis have been reported with isolated skin pathology, we report a case of epidermolytic hyperkeratosis with rickets, a rare association.
Case Report
A 6-year-old boy presented with progressive windswept deformity of the legs since 3 years and scaling of the skin since 4 years. His mother reported that the child was an active, joyful baby, the product of a full-term normal vaginal delivery. Parental consanguinity was present. As narrated by the mother, the boy was born with a bright red color and a few blisters over the trunk. In subsequent days, the redness and blisters subsided, but after 2 years thick dry scales started appearing all over the body. There was no history of factors, including sun exposure that aggravated scaling of the skin.
On examination, generalized dryness and hyperkeratotic plaques were seen, most prominently around flexures like the neck, elbow, ankle and wrist [Figure - 1]. The plaques had a cobble-stone/hystrix pattern with a pungent odor. Relative sparing of the skin between the joints was observed. An important observation was, complete sparing of palm and sole. A few superficial flaccid blisters and peeling of skin were present over the trunk and lower limbs [Figure - 2]. The mucosae, teeth and hair were normal on examination. The boy had a windswept deformity of the legs, rib beading and widening of the wrists and ankles. None of his older siblings or parents had any history of bone or skin disease.
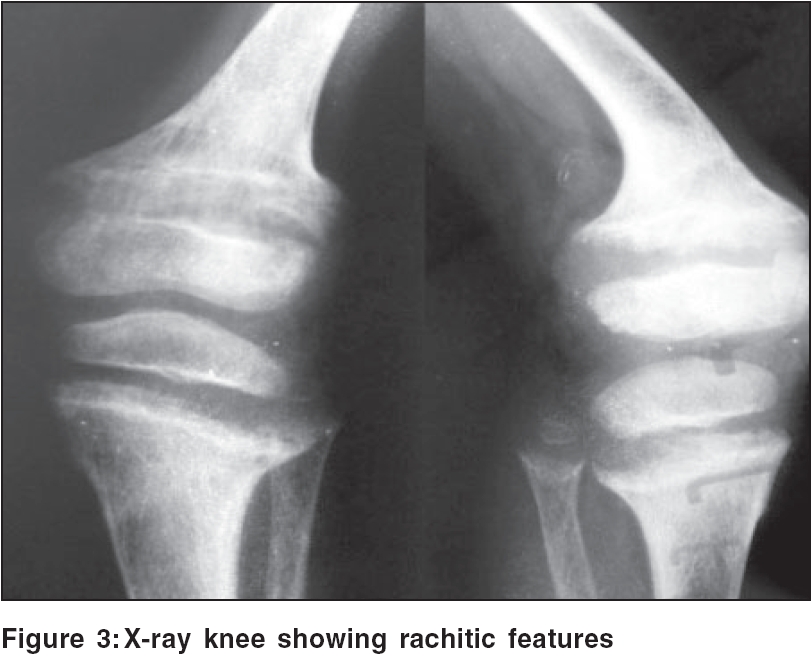
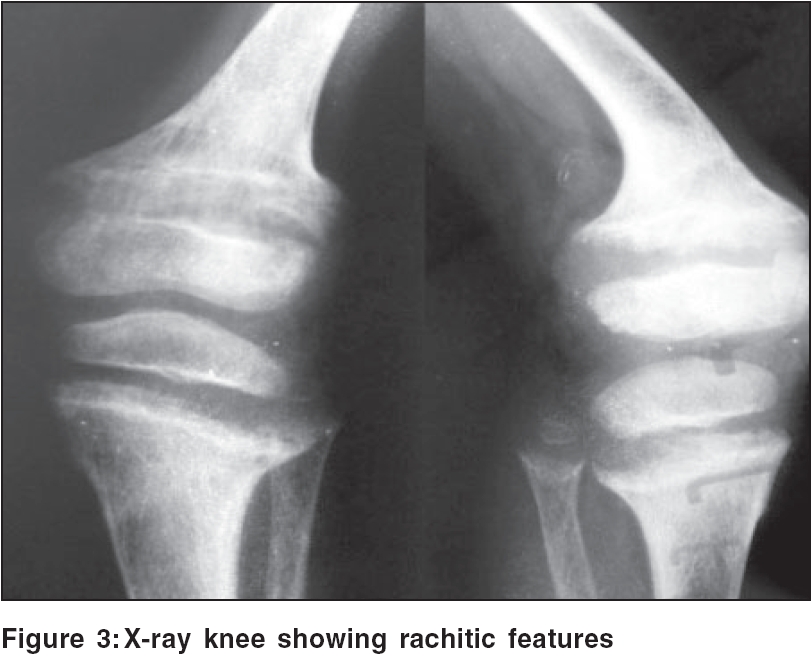
Routine investigations of the blood, urine and stool were noncontributory. Ultrasonography of abdomen and pelvis revealed no abnormality, organomegaly or any space-occupying lesion. The serum calcium, phosphate and 25-hydroxy-vitamin D levels were low, but the serum alkaline phosphatase and parathormone levels were high. X-rays of the knee and wrist showed marked splaying and cupping of the distal metaphyses and widening of the growth plate of the upper end of tibia and fibula. Bowing of the lower end of both femurs with buttressing of the medial cortex was seen [Figure - 3]. Skin biopsy revealed marked hyperkeratosis, acanthosis and vacuolar degeneration involving the upper epidermis with cleft formation [Figure - 4]. The underlying dermis showed a scanty perivascular lymphoid infiltrate.
On the basis of these findings, a diagnosis of epidermolytic hyperkeratosis with active nutritional rickets was made and the child was treated with parenteral vitamin D3 (6 lakh units, intramuscular) and oral calcium supplements (1000 mg in two divided doses) for 6 months. Topically, 10% urea in aqueous cream as an ointment and white soft paraffin were advised. Regular sun exposure was counseled. In a follow-up of 4 months, we found radiological improvement in rickets and almost normal serum calcium, phosphate and alkaline phosphatase levels. However, the skin condition did not improve. Oral retinoids or topical calcipotriene could not be used because the patient′s family could not afford them.
Discussion
EHK, also called bullous congenital ichthyosiform erythroderma, was first described by Brocq in 1902 to distinguish the entity from nonblistering congenital icthyotic erythroderma.[1] It is an autosomal dominant disorder of keratinization. The disease is named for the distinctive histopathological features of vacuolar degeneration of the epidermis (i.e., epidermolysis) and associated hyperkeratosis. There is a high frequency of spontaneous mutations and as many as half the cases have no family history and they represent new mutational events.[2] The disease usually presents at birth with blistering, redness and peeling. With time, generalized hyperkeratosis may develop, which may or may not be associated with erythroderma.
An underlying genetic defect of keratin synthesis or degradation involving keratin K1 and/or keratin 10 has been suggested.[3] Family studies have confirmed an autosomal dominant inheritance and linked it to keratin gene clusters on chromosome 12q and 17q.[4],[5],[6]
Six clinical phenotypes of EHK have been distinguished depending on the presence of severe palmar/plantar hyperkeratosis: three subgroups with palm/sole (PS type) hyperkeratosis and the other three subgroups with no palm/sole (NPS type) hyperkeratosis. In our patient, sparing of the palms/soles, presence of a hystrix pattern of scaling, generalized distribution, blistering, absence of any digital contracture or erythroderma and a histopathological finding made us reach the diagnosis of epidermolytic hyperkeratosis (NPS-1 type). The NPS-2 type of EHK clinically simulates NPS-1 type but lacks the peculiar hystrix pattern scales.
The presence of nutritional rickets in our patient was confirmed by radiological and biochemical studies. As reported by Milstone et al .[7] elevated parathyroid hormone and low to normal 25-hydroxy vitamin D levels are observed in patients with various disorders of keratinization. This is due to a defective synthesis of vitamin D in diseased epidermis or excessive loss of calcium through skin, which stimulates parathyroid hormone secretion, which in turn puts children with ichthyosis at a risk of rickets.[7] Though rickets has been reported in association with lamellar ichthyosis and X-linked ichthyosis,[15] cutaneous hyperproliferative disorders like ichthyosiform dermatoses are uncommon causes of rickets in children.[8],[9] In a series of 41 children with nutritional rickets, only 3 had ichthyosis.[9] Contributing factors may be alteration in cholesterol metabolism involving vitamin D3 receptors,[10] increased keratinocyte proliferation resulting in poor or no penetration of skin by sunlight,[10] associated vitamin D dependent rickets[11] and limited sun exposure as patients avoid sun in summer.[10]
Another problem is its clinical differentiation from ichthyosis bullosa of Siemens and ichthyosis hystrix of Curth and Macklin, two autosomal dominant conditions with almost identical clinical features. However, in ichthyosis bullosa of Siemens, epidermal fragility, though present, is very superficial. Secondly, hyperkeratosis and vacuolization, though present as in EHK, are restricted to the granular layer. In ichthyosis hystrix of Curth and Macklin, hyperkeratosis is widespread, patchy, thick, gray-brown and mostly marked over the extensor aspects of the arms and legs. Absence of blistering in icthyosis hystrix of Curth and Macklin is another distinguishing feature.
EHK is a life-long condition and the most refractory form of ichthyosis. All patients need lifelong ′rickets prophylaxis′ with vitamin D supplements (400 IU/day), as dietary intake alone cannot be relied upon to prevent this condition.[11]
Treatment of skin disorder of EHK is not usually very satisfactory and includes keratolytics, antiseptic washes, topical calcipotriol, alpha hydroxy acids and oral retinoids. Lacour et al. showed that treatment with acitretin is safe and effective for such patients.[12] A multicenter study by Baden et al. showed a good response with isotretinoin.[13] In topical therapy, the skin condition responds well to calcipotriene but the vitamin D deficiency is not reversed.[14] Although our patient′s rickets improved, his skin condition did not, a finding consistent with reports made by many authors.[14],[15] Devidayal et al. had a similar observation in a case of nonbullous icthyosiform erythtroderma with nutritional rickets, where rachitic features responded nicely to oral and parenteral vitamin D3 .16
| 1. |
DiGiovanna JJ, Bale SJ. Clinical heterogeneity in epidermolytic hyperkeratosis. Arch Dermatol 1994;130:1026-35.
[Google Scholar]
|
| 2. |
Simpson JR. Congenital ichthyosiform erythroderma. Trans St John's Hosp Derm Soc 1964;50:93.
[Google Scholar]
|
| 3. |
Di Giovanna JJ, Bale SJ. Epidermolytic hyperkeratosis: Applied molecular genetics. J Invest Dermatol 1994;102:390.
[Google Scholar]
|
| 4. |
Bonifas JM, Bare JW, Chen MA, Lee MK, Slater CA, Goldsmith LA, et al . Linkage of epidermolytic hyperkeratosis, phenotype and region of type II keratin cluster on chromosome 12. J Invest Dermatol 1992;99:524-7.
[Google Scholar]
|
| 5. |
Compton JG, Di Giovanna JJ, Santucci SK. Linkage of epidermolytic hyperkeratosis to type II keratin gene cluster on chromosome 12q. Nature Genet 1992;1:301.
[Google Scholar]
|
| 6. |
Rothangel JA, Dominey AM, Dempsey MD. Mutation in rod domains of keratins 1 and 10 in epidermolytic hyprkeratosis. Science 1992;257:1128-30.
[Google Scholar]
|
| 7. |
Milestone LM, Ellison AF, Insogna KL. Serum parathyroid hormone level is elevated in some patients with disorder of keratinization. Arch Dermatol 1992;128:926-30.
[Google Scholar]
|
| 8. |
Scott CI. X-linked ichthyosis vulgaris. Birth Defects Orig Artic Ser 1971;7:243-4.
[Google Scholar]
|
| 9. |
el Hag Al, Karrar ZA. Nutritional vitamin D deficiency rickets in Sudanese children. Ann Trop Pediatr 1995;15:69-76.
[Google Scholar]
|
| 10. |
Griffiths WAD, Judge MR, Liegh IM. Disorders of keratinization. In: Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Rook/ Wilkinson/ Ebling Textbook of Dermatology. 6th ed. Blackwell Science: Oxford; 1998. p. 1483-588.
[Google Scholar]
|
| 11. |
Holm AL, Goldsmith LA. Impetigo herpetiformis associated with hypocalcemia of congenital rickets. Arch Dermatol 1991;127:1587-8.
[Google Scholar]
|
| 12. |
Lacour M, Mehta-Nikhar B, Artherton DJ, Harper JI. An appraisal of acitretin therapy in children with inherited disorder of keratinization. Br J Dermatol 1996;134:1023-9.
[Google Scholar]
|
| 13. |
Baden HP, Buxman MM, Weinstein GD, Yoder FW. Treatment of icthyosis with isotretinoin. J Am Acad Dermatol 1982;6:716-20.
[Google Scholar]
|
| 14. |
Thacher TD, Fischer PR, Pettifor JM, Darmstadt GL. Nutritional rickets in Ichthyosis and response to calcipotriene. Pediatrics 2004;114:e119-23.
[Google Scholar]
|
| 15. |
Okano M, Kitano Y, Yoshikawa K. A trial of oral 1 alpha-hydroxyvitamine D3 for Icthyosis. Dermatologica 1988;177:23.
[Google Scholar]
|
Fulltext Views
5,865
PDF downloads
2,468





