Translate this page into:
Erythema elevatum diutinum
Correspondence Address:
Vikram K Mahajan
Department of Dermatology, Venereology and Leprosy, Dr. R. P. Govt. Medical College, Kangra (Tanda) - 176 001, Himachal Pradesh
India
| How to cite this article: Sharma V, Mahajan VK, Mehta KS, Chauhan PS, Chander B. Erythema elevatum diutinum. Indian J Dermatol Venereol Leprol 2013;79:238-239 |
A 54-year-old HIV-negative man presented with multiple firm, nodules, and plaques of variable size and shapes, having smooth surface and dusky plum-colored erythema. They were distributed predominantly over extensor aspects of both extremities particularly dorsal hands, elbows, buttocks, knees, dorsal feet, and over Achilles tendon [Figure - 1], and occasional one over face for the last about 18 months. These were progressive in size and mostly asymptomatic except for occasional feeling of numbness, paraesthesias and mild pain in acral lesions on exposure to cold. Some of them were eroded and others showed resolution with hyperpigmentation. He had no arthralgia or arthritis but felt some restriction of joint movements due to overlying skin lesions. He had no eye complaints, sore throat, or constitutional symptoms. Systemic examination and laboratory investigations including blood counts, serum biochemistry, urinalysis, C-reactive protein, rheumatoid factor, ASO titers, VDRL, slit-skin smear examination, and chest X-ray showed no abnormality. Histology of an erythematous plaque showed leukocytoclastic vasculitis and fibrinoid degeneration and neutrophilic infiltrate and fibrosis in the dermis [Figure - 2]. With the diagnosis of erythema elevatum diutinum he was prescribed dapsone 100 mg/d after G6PD estimation was normal. A recent follow-up revealed that except for fibrotic lesions most of the lesions had resolved within 2 months′ of treatment.
 |
| Figure 1: Typical smooth surfaced red-purplish erythematous noduloplaques of erythema elevatum diutinum over - (a) dorsal hands, knuckles, (b) buttocks, (c) dorsal feet, lateral borders, and small joints, (d) heels, Achilles tendons, and lower legs. Note the lesions over heels are hyperkeratotic and hyperpigmentation left by the resolved lesions |
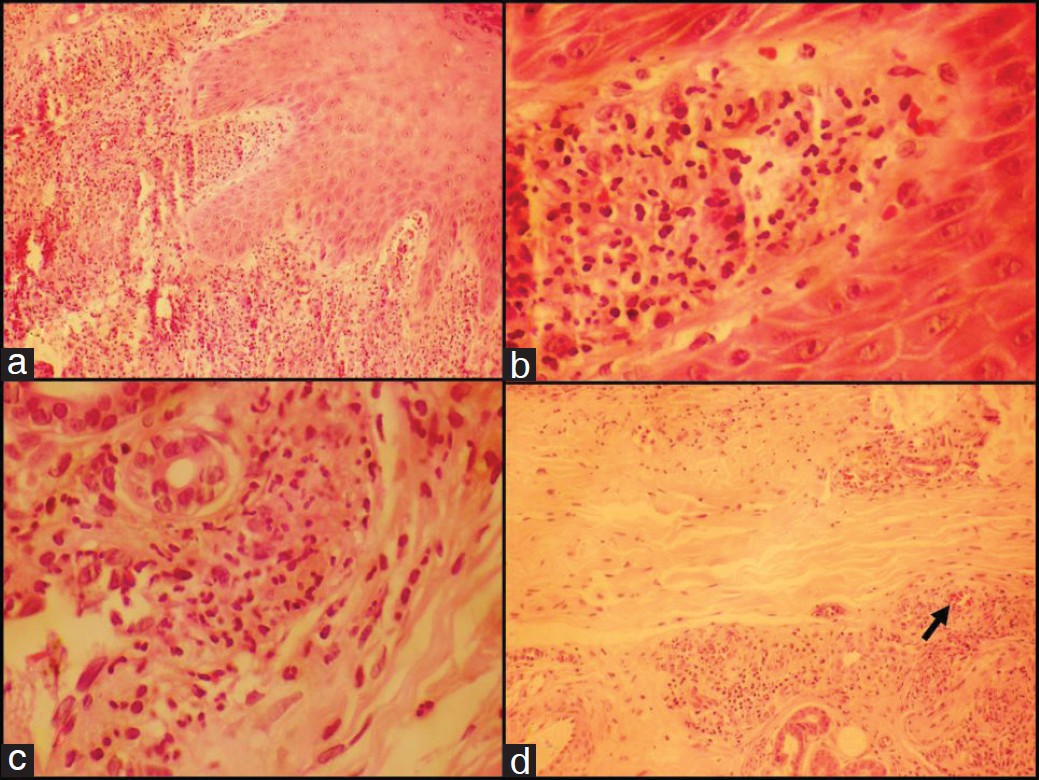 |
| Figure 2: Histology of an erythematous plaque (a) Superficial dermal inflammatory cell infiltrate, (b) in the papillary dermis, (c) leukocytoclastic vasculitis, fibrinoid degeneration, neutrophilic infiltrate, and (d) fibrosis in the dermis, Arrows indicate extravasations of red blood cells and active leukocytoclastic vasculitis. [H and E Stain, x10 (A), x 40 (A,B,C)] |
Erythema elevatum diutinum (EED) is a rare chronic dermatosis and majority comprises adult patients. Characteristic skin lesions are asymptomatic (pain is occasional), plum colored erythemtous nodules, and plaques of variable size distributed symmetrically over extensors of extremities particularly over the joints, dorsal hands and feet, knees and elbows, buttocks and Achilles tendon, and occasionally face and ear pinnae. The initial soft lesions eventuate to become fibrotic and develop atrophic scarring. Characteristic histologic features of leukocytoclastic vasculitis with some fibrin deposition and eosinophilic infiltrate in the upper and mid dermis are seen in early lesions while capillary proliferation, inflammatory infiltrate of macrophages, plasma cells, and lymphocytes, and perivascular eosinophilic fibrosis are hallmark features of chronic lesions. Clinicopathologic correlation is important for the diagnosis as EED lesions may sometimes mimic cutaneous sarcoidosis, leprosy, discoid lupus erythematosus or psoriasis. Histologically it may be difficult to differentiate other forms of small vessel vasculits and Sweet′s syndrome. The etiopathogenesis of EED remains obscure and has been attributed to Arthus-like immune complex reaction and ensuing fibrin deposition. It has been reportedly associated with a number of autoimmune diseases (rheumatoid arthritis, celiac and inflammatory bowl disease, diabetes mellitus), infections (syphilis, streptococcus, hepatitis, HIV infection), malignancies (multiple myeloma, B-cell lymphoma, breast carcinoma, myelodysplasia), monoclonal gammopathies, hypergammaglobulinemia, pyoderma gangrenosum, and relapsing polychondritis. IgA monoclonal gammopathy is found in a significant number of EED patients and some workers even advocate routine immunoelectrophoresis testing for it. However, the high cost and limited availability in most resource poor centers often precludes routine immunoelectrophoresis testing as has been the case in our patient. Dapsone has remarkable therapeutic effect and remains mainstay of the treatment. However, resurgence is common on its discontinuation. Sulfpyridine, colchicine or cyclophosphamide are other alternative treatments. Potent topical or intralesional corticosteroids are useful for the limited disease and niacinamide may be of value in some patients. Systemic corticosteroids generally are not effective. Treatment of associated disease may resolve EED. Dapsone may need to be combined with strict gluten-free diet for resolution of EED associated with celiac disease. Intermittent plasma exchange is useful in IgA paraproteinemia associated and refractory to treatment EED. HIV-associated EED responds to addition of antiretroviral treatment.
Fulltext Views
6,622
PDF downloads
2,144





