Translate this page into:
Erythromelanosis follicularis faciei et colli: Relationship with keratosis pilaris
Correspondence Address:
M Augustine
Department of Dermatology, St. John's Medical College Hospital, Sarjapur Road, Bangalore - 560 034, Karnataka
India
| How to cite this article: Augustine M, Jayaseelan E. Erythromelanosis follicularis faciei et colli: Relationship with keratosis pilaris. Indian J Dermatol Venereol Leprol 2008;74:47-49 |
Abstract
Erythromelanosis follicularis faciei et colli (EFF) is an unusual condition characterized by the triad of hyperpigmentation, follicular plugging and erythema of face and neck. This is less common in women and familial case reports are few. We report EFF in three siblings in an Indian family, two of whom are females. The possibility of this condition being genetically related to keratosis pilaris as well as being a variant of keratosis rubra pilaris is also discussed.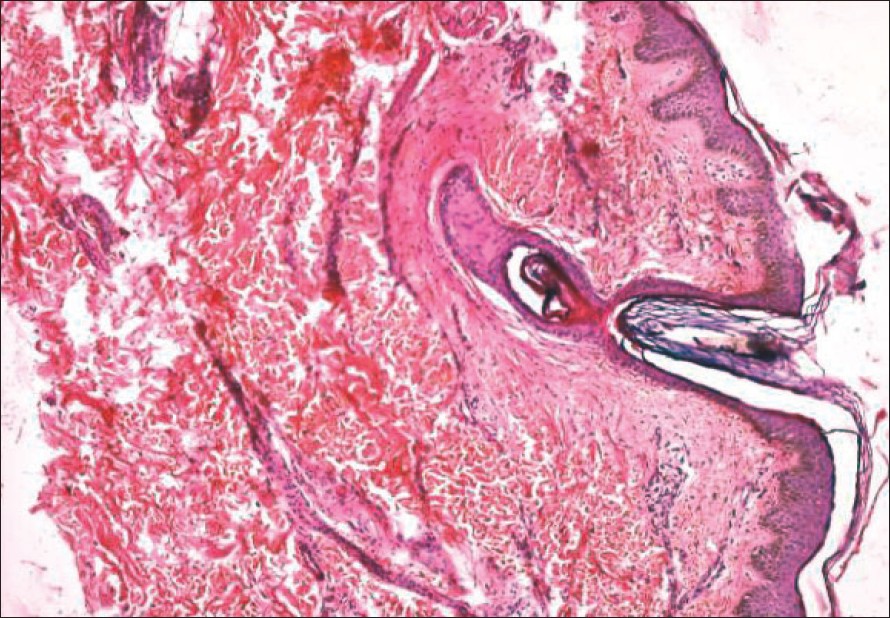 |
| Figure 2: Hyperkeratosis, follicular plugging and variable hyperpigmentation in EFF (H and E stain, X100) |
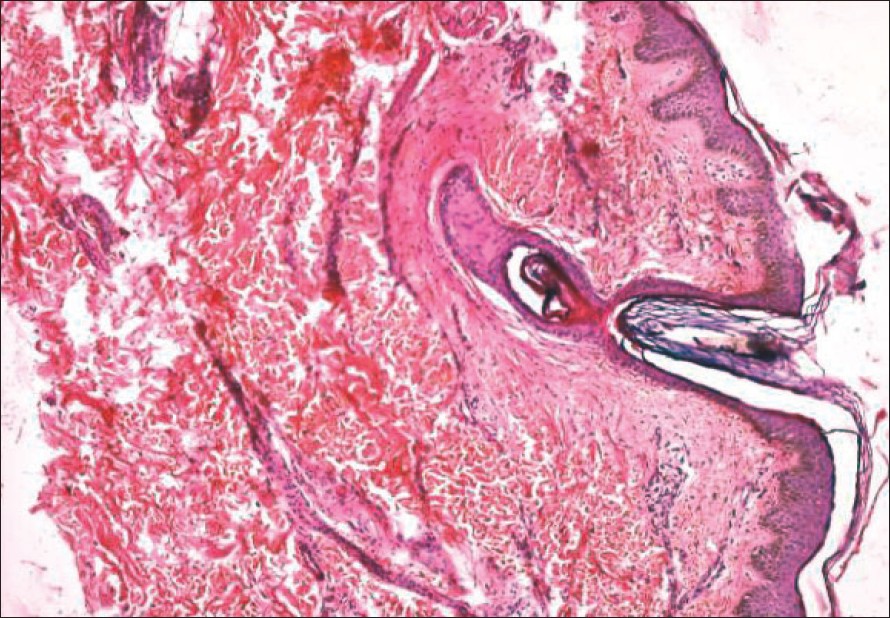 |
| Figure 2: Hyperkeratosis, follicular plugging and variable hyperpigmentation in EFF (H and E stain, X100) |
 |
| Figure 1: Erythematous patches with telangiectasia and papules in Case 1 |
 |
| Figure 1: Erythematous patches with telangiectasia and papules in Case 1 |
Introduction
Erythromelanosis follicularis faciei et colli (EFF) was originally described by Kitamura et al. [1] This condition is characterized by well-demarcated erythema, pigmentation and follicular papules, involving mainly the pre-auricular areas, with extension to the sides of the neck. Although initially reported only in men, there have been many reports of EFF in women since 1980. [1],[2],[3] The possibility of a genetic transmission in an autosomal recessive pattern has been considered earlier. [2],[4] We report three cases of EFF, including a familial case. This is the first report of familial EFF from India.
Case Reports
Case 1
A 19-year-old girl presented with history of redness and roughness of the cheeks from three to four years of age, which was gradually spreading on to the neck and ears. She complained of burning sensation and increased redness over these areas, on exposure to sunlight. There was no history of any topical applications except emollients. Examination revealed well-defined but irregular areas of erythema with telangiectasia and hyperpigmentation, involving the pre-auricular area of the cheeks, chin, pinnae of the ears and the submandibular areas of the neck [Figure - 1],[Figure - 2]. Patches of brownish pigmentation persisted on diascopy, over the cheeks and chin. The skin texture was granular, with many, pale, follicular papules. There was no evidence of atrophy or scarring although vellus hair appeared to be less over these areas. Prominent keratosis pilaris was seen on the upper back, shoulders and the arms, with mild erythema around the papules. There was no diffuse erythema or pigmentation over these areas. Patient′s younger sister and brother also had similar skin lesions, which started around the age of four to six. Her mother had extensive keratosis pilaris on the upper extremities; but no erythema or pigmentation was observed. Histopathology from the submandibular area of the patient showed hyperkeratosis, follicular plugging, increased pigmentation in the basal layer and mild perivascular lymphocytic infiltrate. Calcium stains were not contributory.
Case 2
A 10-year-old girl came to us with well-demarcated patches of erythema and pigmentation over the pre-auricular areas of the cheeks as well as the chin, since the last three to four years. The surface of these patches was rough, with tiny whitish papules. Telangiectasia was minimal, although the pigmentation was more prominent than in Case 1. She gave history of increased erythema on sun exposure but had no burning sensation. Both the patient and her mother had keratosis pilaris, which was less in extent and severity than the previous case.
Case 3
A 13-year-old boy presented with irregular, well-defined erythematous patches involving the cheeks, with brownish pigmentation and follicular papules on these patches starting at about the age of eight or nine. He too observed erythema over these areas, as well as increased pigmentation on sun exposure. His father had keratosis pilaris although the patient had only a few scattered papules over the shoulders.
Discussion
Erythromelanosis follicularis faciei et colli is being increasingly described both in men and women. It appears that EFF is not as rare as it was thought to be. Although an autosomal recessive pattern of inheritance has been proposed, familial case reports are few. The possibility of a spontaneous mutation has also been mentioned. [5] Erythromelanosis follicularis faciei et colli has recently been considered to be a poly-etiological disorder with the possibility of a chromosomal instability syndrome. [6]
Keratosis pilaris is known to be frequently associated with EFF, both in the patient as well as in the family. [2],[7] Three siblings in Case 1 had EFF with keratosis pilaris, while their mother had significant keratosis pilaris. The other two patients also had one parent having keratosis pilaris. This observation suggests that these two conditions may be genetically related.
Erythromelanosis follicularis faciei et colli has been considered to be a variant of keratosis pilaris rouge [8] in view of the follicular papules, blotchy erythema and associated keratosis pilaris; although EFF is distinguished by the extension on to the neck and the presence of pigmentation. That EFF is a variant of keratosis pilaris appears likely, as our patient (Case 1) had erythema around the keratosis pilaris papules on the back and upper arms, whereas the facial lesions showed typical features of EFF i.e. diffuse erythema, telangiectasias and pigmentation in the interfollicular areas. It is possible that the areas exposed to sunlight develop pigmentation and telangiectasias on the interfollicular skin, over the years, in the predisposed skin.
Erythromelanosis follicularis faciei et colli has also been thought to be very similar or identical to keratosis rubra pilaris atrophicans faciei (Brocq). Overlap with this condition as well as with ulerythema ophryogenes has been considered earlier in view of atypical distribution such as the auricles and the eyebrows. [5],[9] Although our patient (Case 1) had lesions on the auricles, she had no evidence of scarring, atrophy or loss of the eyebrow hair.
The clinical presentations of most reported cases are similar. However, there are variations in symptoms and seasonal influences. [1],[2],[10] Exacerbation by sunlight has been observed only in a few of the earlier reported cases. All the three siblings in Case 1 had history of burning sensation and increased redness over the EFF lesions, while Cases 2 and 3 noticed increased erythema, on sun exposure.
Histopathology of our patient correlated well with the previous reports. Calcium stains were not contributory as has been concluded earlier. [5]
Differential diagnosis of EFF includes atrophoderma vermiculatum, ulerythema ophryogenes, poikiloderma of Civatte and keratosis pilaris. Atrophoderma vermiculatum is characterized by honeycombed atrophy, primarily affecting the cheeks. Ulerythema ophryogenes presents with erythema that results in alopecia, scarring and atrophy, predominantly involving the eyebrows, forehead and cheeks. Both these conditions are differentiated from EFF by the presence of atrophy and scarring. Poikiloderma of Civatte is seen in middle-aged women, as a reticulate pigmentation associated with telangiectasias and atrophy. It is distributed over the sun-exposed areas of the cheeks and sides of neck, sparing the shaded areas. [11] Absence of follicular papules along with the age of onset and distribution, differentiate this from EFF. Keratosis pilaris of the face is not associated with well-defined patches of erythema and pigmentation although erythema may be seen around the papules.
Erythromelanosis follicularis faciei et colli appears to be more common than previously believed and familial cases are increasingly being reported. This condition is probably genetically related to keratosis pilaris. The exact nature of genetic transmission needs to be clarified.
| 1. |
Anderson BL. Erythromelanosis follicularis faciei et colli: Case reports. Br J Dermatol 1980;102:323-5.
[Google Scholar]
|
| 2. |
Warren M, Davis LS. Erythromelanosis follicularis faciei in women. J Am Acad Dermatol 1995;32:863-6.
[Google Scholar]
|
| 3. |
Hodak E, Ingber A, Alcalay J, David M. Erythromelanosis follicularis faciei in women. J Am Acad Dermatol 1996;34:714.
[Google Scholar]
|
| 4. |
Acay MC. Erythromelanosis follicularis faciei et colli: A genetic disorder? Int J Dermatol 1993;32:542.
[Google Scholar]
|
| 5. |
Griffiths WA, Judge MR, Leigh IM. Disorders of keratinization. In : Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Rook Textbook of Dermatology. 6 th ed. Oxford: Blackwell; 1998. p. 1537-8
[Google Scholar]
|
| 6. |
Tuzun Y, Wolf R, Tuzun B, Ozdemir M, Demirkesen C, Deviren A, et al. Erythromelanosis follicularis and chromosomal instability. J Eur Acad Dermatol Venereol 2001;15:150-2.
[Google Scholar]
|
| 7. |
Ermertcan AT, Ozt�rkcan S, Sahin MT, T�rkdogan P, Saηar T. Erythromelanosis follicularis faciei et colli associated with keratosis pilaris in two brothers. Pediatr Dermatol 2006;23:31-4.
[Google Scholar]
|
| 8. |
Watt TL, Kaiser JS. Erythromelanosis follicularis faciei et colli. J Am Acad Dermatol 1981;5:533-4.
[Google Scholar]
|
| 9. |
Seki T, Tkahashi S, Morohashi M. A case of Erythromelanosis follicularis faciei with a unique distribution. J Dermatol 1991;18:167-70.
[Google Scholar]
|
| 10. |
Sodaify M, Baghestani S, Handjani F, Sotoodeh M. Erythromelanosis follicularis facie et colli. Int J Dermatol 1994;33:643-4.
[Google Scholar]
|
| 11. |
Bleehen SS. Disorders of skin color. In : Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Rook Textbook of Dermatology. 6 th ed. Oxford: Blackwell; 1998. p. 1790.
[Google Scholar]
|
Fulltext Views
12,630
PDF downloads
2,206





