Translate this page into:
Evaluation of the effect of Block Level Awareness Campaign on performance indicators of National Leprosy Elimination Program in Vadodara district, Gujarat, India
2 Department of District Nucleus Medical Officer, District Leprosy Office, Vadodara, Gujarat, India
Correspondence Address:
Lipy K Shukla
'Dev-Darpan', 01, Bombay Housing Society, University Road, Rajkot - 360 005, Gujarat
India
| How to cite this article: Shukla LK, Patel RN, Patel SV, Baxi RK. Evaluation of the effect of Block Level Awareness Campaign on performance indicators of National Leprosy Elimination Program in Vadodara district, Gujarat, India. Indian J Dermatol Venereol Leprol 2015;81:257-262 |
Abstract
Background: Leprosy is probably the oldest disease afflicting mankind and a public health problem for centuries. Many cases are hidden or undiagnosed, especially due to social stigma, and neglect of painless patches. Between years 2001 and 2005, during which time active surveillance for detection of leprosy was in practice, a steep fall in the prevalence rate (PR) of leprosy was observed. However, during later years, leprosy program discontinued active surveillance for detection of leprosy cases. Presently block level awareness campaign (BLAC) is a special measure undertaken in a campaign mode during September-November in priority areas, (PR > 1/10000 population), during which information, education and communication (IEC) activities and active surveillance of leprosy cases is done. Aims: To evaluate the effect of Block Level Awareness Campaign on performance indicators of national leprosy elimination program (NLEP) in Vadodara district. Methods: The campaign was carried out for 6 days in 12 talukas of Vadodara district by the district leprosy office, Vadodara. Trained teams of health workers carried out information, education and communication (IEC) activity and active surveillance by undertaking house to house survey in each primary health centre (PHC) area. Suspected cases were identified by the team and confirmed clinically by medical officers in the primary health centre of the corresponding areas. A district nucleus team (DNT) validated these confirmed cases. These data were compared with the district's national leprosy eradication programme (NLEP) data for the same year, 2012 and the previous year, 2011. Results: A total of 1,574,586 persons, comprising 76%of the population surveyed, were screened for leprosy, which resulted in detection of 358 clinically confirmed new cases of leprosy, out of which 225 (62.8%) were paucibacillary (PB) and 133 (37.2%) were multibacillary (MB) leprosy. Of these cases, 14 (4%) had deformities, and 37 (10.3%) were children. Limitations: Only 76% of the population could be covered. Histopathological confirmation of the diagnosis was not undertaken. Because of the large number of health workers invovled, variations in their skills may have influenced the diagnosis of suspected cases. Conclusions: Active surveillance linked to focused block level campaigns can be useful tools to detect new hidden leprosy cases.INTRODUCTION
Leprosy is a chronic disease with acute exacerbations involving skin and peripheral nerves. This disease impacts the individual and the community producing disability and deformity and social stigma and discrimination. These are preventable but often permanent and progressive even after treating the patient with multidrug therapy (MDT). [1] The world health assembly declared a goal of global elimination of leprosy with a prevalence rate (PR) of <1/10,000 population in May 1991. [2] In India, a sharp 80% reduction in prevalence was observed from 2001 to 2005. India achieved elimination in December 2005 with a prevalence rate of 0.89/10000. [3] The current prevalence of leprosy in India is 0.68/10,000 population as of April 1, 2012 [4] but in Gujarat it was 0.82/10,000 as on April 1, 2012 and 1.14/10,000 as on December 2012. [5] World Health Organization global strategy (Plan 2006-2010) mentions "discontinue campaign approach" as one of the main elements of strategy. [6] A block level awareness campaign (BLAC) [7] was carried out to seek out undetected leprosy cases in rural Vadodara through active surveillance to evaluate the effect of such a campaign on all performance indicators of the national leprosy elimination program (NLEP).
METHODS
A cross-sectional study was carried out between October 2012 and December 2012 in all 12 rural and tribal talukas of Vadodara district, Gujarat. A 6-day block level awareness campaign, was carried out between October 29, 2012 and November 3, 2012 in each primary health centre area of Vadodara district, which has a population of 2,074,174 (1,161,853 in rural talukas, 912,321 in tribal talukas).
Training was conducted prior to campaign activity. All medical officers in the primary health centre (MO PHCs) were trained at district level by the district nucleus team (DNT) of district leprosy officer (DLO), Vadodara. Paramedical field staffs were trained by the nucleus team at taluka level. Accredited social health activist (ASHA) workers were trained for ′identification of suspects′ by medical officers and leprosy supervisors at primary health centres. The teams were provided with photographs and information, education and communication material to be shown to the public during the campaign.
Active surveillance for leprosy cases was done by house to house survey and screening of people for leprosy, after taking their informed verbal consent, by a team of four members, which consisted either of two paramedical staff of the primary health centre and two ASHA workers, or one paramedical staff and three ASHA workers.
Each team was trained to survey a maximum of 150 houses in a day. In this way, in 6 days the whole population of 700-900 households in each sub-centre of rural areas, and 500-600 households in tribal areas was covered.
To cover the population of the whole district, it was estimated that approximately 624 teams of four members each (259 teams to cover rural population and 365 teams to cover tribal population) would be required. We had the services of 2040 trained ASHA, 743 male and female health workers and 27 leprosy assistants across the district, making a total workforce of 2810 allocated to form 702 teams of four members each, recognizing that some of these workers could go on leave during the days of survey.
Information, education and communication (IEC) activity was carried out by the teams before and during the campaign. Out of a total population of 2,074,174 in the rural and tribal talukas of Vadodara, 1,574,586 (76%) people were covered by the teams.
Team members looked for and registered suspected leprosy cases from households. Suspected cases were examined by the medical officer of the primary health centre, the diagnosis was confirmed clinically and cases were classified (based on WHO operational classification of leprosy) into multibacillary (MB) or paucibacillary (PB). These confirmed cases were validated by the district nucleus team and then put on treatment.
The supportive supervision, monitoring, and technical guidance was provided by members of the district nucleus team for leprosy which consisted of the following: 1 District leprosy officer, 3 district nucleus medical officers, 1 senior leprosy supervisor, 3 district leprosy supervisors, and 1 physiotherapist.
Data collection and consolidation was done by daily report at the end of the day submitted by all the teams to the medical officer of the primary health centre who prepared a final report at the end of the 6-day activity. The report of the talukas was generated by the taluka health officer (THO) by compiling the primary health centres reports and were submitted to the district leprosy officer, Vadodara.
This data of campaign activity was analyzed and added to the district′s monthly performance report (MPR). Some important indicators of the national leprosy elimination programme (NLEP) such as prevalence rate, annual new case detection rate (ANCDR), multibacillary (MB) disease proportion, child proportion, and deformity proportion were derived from this data. These indicators were compared with the monthly performance report of the period from April 1, 2012 to December 31, 2012, and also compared with programme indicators for the same period in 2011.
RESULTS
A total population of 2.08 million from 12 talukas of Vadodara district was covered by household surveys. Of this, 76% (1,574,586) was screened for leprosy by trained team members. All the persons available in the household were screened for hypo-pigmented anaesthetic patches anywhere on the body.
Three thousand four hundred and ninety eight (0.2%) individuals out of the total screened population were suspected to have leprosy by the teams. Of these, 3441 (98.6%) could be examined by the medical officer of the primary health centre either by a home visit or by asking the patient to come to the nearest centre. If the suspected case could not be examined at the first attempt by the doctor, then either the health worker of the sub-centre concerned or the ASHA worker reminded the patient to go to the primary health centre and consult the medical officer. However, there was a provision made for the patient′s benefit, whereby, if a suspected case presented even after the 6 days of campaign activity, that patient was examined and treated. This, however, was not reflected in the report of campaign activity but was included in monthly performance report of the month, if confirmed as a case.
Out of the 3441 individuals examined by the medical officers, campaign activity yielded 358 (10.4%) confirmed leprosy cases, which were classified into paucibacillary (PB) or multibacillary (MB) leprosy. These cases were validated by the district nucleus team and then put on treatment according to their category.
Out of this yield of 358 new leprosy cases from the campaign, 185 (51.7%) were females; 133 (37.2%) were multibacillary and 225 (62.9%) were paucibacillary cases. A total of 37 (10.3%) were children. Out of the new cases found, 344 (96%) did not have deformities.Of the 14 cases with deformity, 8 (57.2%) had grade I and 6 (42.9%) had grade II deformities [Table - 1].
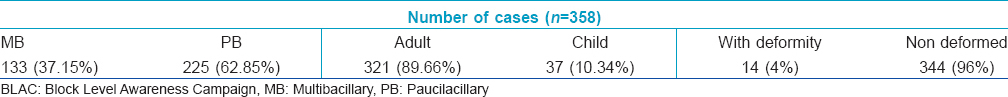
On comparing data of the campaign activity period with that of the rest of the year (2012) and the corresponding period of the previous year (2011), the following results were observed: approximately 38% of total cases of the year 2012 from April to December (3 quarters) were detected during the campaign, while the remaining 62% cases were found in the remaining period [Figure - 1]. Rise in the annual new case detection rate (ANCDR) was noted in the month of November 2012 from an average of 21.3 to 28.9/100000 population [Figure - 2].The prevalence rate increased in the month of November 2012 after active surveillance activity.
 |
| Figure 1: Total number of new cases detected per month under NLEP – District Vadodara |
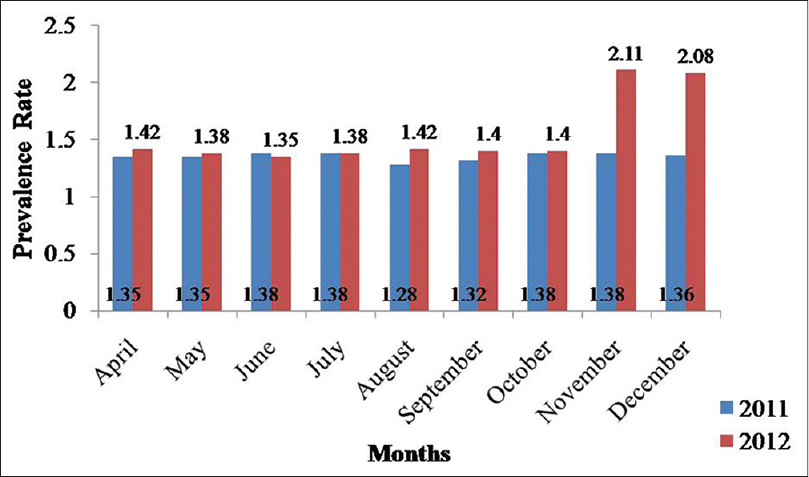 |
| Figure 2: Month wise prevalence rate of leprosy – District Vadodara |
The percentage of multibacillary (MB) and paucibacillary (PB) cases was 51.5% and 48.5%, respectively in the year 2011, and 51.9% and 48.1%, respectively in the year 2012, while during campaign activity it was 62.9% and 37.2%, respectively.
Child cases were 5.3% of the total number in the year 2011, 8.4% in the year 2012, and 10.4% during campaign activity. Cases with deformity comprised 15.7% of the total number in the year 2011, 7% in the year 2012, and only 4% during campaign activity.
DISCUSSION
Despite the world health assembly′s enthusiastic adoption in 1991 of a resolution to "eliminate leprosy as a public health problem by the year 2000" [3] ; it remains an important cause of global chronic neurological disability and one of the main causes of crippling and deformities. India was one among the twelve countries that failed to reach the elimination target set by the WHO of less than one case of leprosy per 10,000 population by 2000. However, India achieved elimination in December 2005, with a prevalence rate of 0.89/10,000 population. [4],[8] Despite this achievement, seven years later, we still have districts with a prevalence rate of not just >1/10,000 but even >2 or 3/10,000 population in a state like Gujarat. [4],[9] It thus becomes imperative to seek evidence to verify the state of elimination. Some important questions must be answered concerning effectiveness of interventions to reduce transmission and the source of infection and strategies under the national leprosy elimination programme (NLEP). [10],[11] National leprosy programs now encourage people to come forward for treatment by information, education, communication (IEC) activities, and recommend limiting leprosy services to general health facilities. [8] Low levels of awareness, high social stigma, ignorance of a painless patch, long incubation period and late neurological manifestations are hindrances to the patient seeking health care in the early stages.
This study shows that active case search brings the patient to the health care facility earlier, and may thus reduce the progression towards disability and deformity and also break the chain of transmission in the community.
The study also reveals the presence of a large number of undetected leprosy cases in the community in Vadodara district and highlights the wide gap between prevalence of leprosy as detected by routine passive case finding methods and the estimated prevalence after active surveillance activity [Figure - 1]. It definitely does not mean that suddenly new cases of leprosy have emerged or that an epidemic of leprosy has occurred, but because of leprosy having a long and variable incubation period, and for many of the other reasons mentioned earlier, a large number of patients are not seeking health care. This is a limitation of the present strategy and confining leprosy patient services to facility-based care results in a number of patients remaining undetected in the community for a long period of time.
Only 76% of the total rural and tribal population could be surveyed during the six days of campaign activity. Considerable manpower is required for such an activity. Considering the constraints of available resources in the public health system, it may not be possible to carry out such activities routinely. Active participation of the target population is also crucial to this exercise.
While 358 confirmed cases of leprosy from a surveyed population of 2.1 million may appear to be a tiny number, this number is huge when we are claiming elimination of the disease and progress towards eradication. [12] Identification of these previously undetected 358 cases has shifted the status of prevalence in Vadodara district from >1/10,000 to >2/10,000 populations and with an increase in the annual new case detection rate from 21.3 to 28.9/100,000 population. This is a warning sign, and an indication that there should be an active thrust to identify new cases. It is important to identify any hidden infective source cases, trace, and treat them.
A study in rural and urban areas of Maharashtra, western India by Shetty et al. threw up similar findings of previously undetected leprosy cases, with a prevalence of 5.04 in rural and 2.13 per 100,000 population in urban areas. [13] Moura et al., in a study from Brazil, found that, based on dermatologic and neurologic examination, there were 62 (9.7%) suspected Hansen′s disease cases out of 637 people without a previous history of the disease. Clinical and histopathological examination by a specialist confirmed the diagnosis in 15 people, which corresponded to a detection rate of 2.4 cases per 100 examinations. [14] Histopathological confirmation was not done in the present study because it is no longer mandatory for confirmation of diagnosis according to the Indian national leprosy elimination programme guidelines.
In the NLEP report of 2008, a total of 137,685 new leprosy cases were detected in the year 2007-2008. About half (47.2%) of these cases were multibacillary. [15] In this study, a higher percentage of paucibacillary cases (62.9%) were found. This suggests that it is possible to detect cases in the early stage of the disease if proactive efforts are employed. As untreated multibacillary cases are a major source of infection, they will continue to spread infection unless put on treatment early, [16] this can also be prevented by active surveillance.
The number of children acquiring leprosy remains high, accounting for 9.7% of the total new case load according to the national leprosy elimination programme (NLEP) report 2011-2012. In this study also, 10.4% of cases were children. [5] This indicates that there is active transmission in the community, even when we are claiming elimination of the disease for the past 7-8 years. [4],[5],[8]
Although multidrug therapy alone is not effective in the control of nerve damage, early initiation of therapy helps reduce the chances for development of deformities. [16] Since 96% of the cases found during the campaign were cases without deformity, early treatment, and periodic observation, is likely to prevent deformities. Appropriate and timely treatment is of paramount importance in leprosy cases with deformity and crucial in prevention and treatment of early nerve function impairment. Proper case management and adherence to treatment remains another challenge, discussion of which is beyond the scope of this paper.
Although it was an attempt to screen 2.1 million population of rural and tribal Vadodara, even after careful planning only 76% of total population could be covered during 6 days of campaign. The remaining 24% of population numbered 4,99,588 approximately and we have no information on the presence of hypopigmented, painless, anesthetic patches in those individuals. Another limitation was the lack of uniformity in skills of the large number of health workers involved in the study. Even though they were trained, supportively supervised and monitored there are chances that ASHAs and paramedical workers in the surveying team may have missed some suspected cases because of variation in their skills and understanding.
In conclusion, a proactive strategy can still be useful to detect hidden cases in the community. Though it is not possible and practical for our public health system to carry out active surveillance routinely, campaign mode can be adopted at least once or twice yearly, especially for districts with high prevalence.
ACKNOWLEDGEMENT
Dr. R. R. Finavkar, District Leprosy Officer, Vadodara, Gujarat, India.
| 1. |
Training module for medical officer. NLEP, Directorate general of health services, MOHFW, NirmanBhavan, New Delhi; 2/01/2009.
[Google Scholar]
|
| 2. |
Leprosy elimination: World Health Assembly (WHA) resolution to eliminate leprosy, 1991. World Health Organization; Available from: http://www.who.int/lep/strategy/wha/en/;[07/01/2013].
[Google Scholar]
|
| 3. |
Dhillon GPS, Barkakaty BN. National leprosy eradication in India, Achievements and Deficiencies.XVII (2):4-7.
[Google Scholar]
|
| 4. |
NLEP - Progress Report for the year 2011-12. Central Leprosy Division, Directorate General of Health Services, New Delhi, India, 2012.
[Google Scholar]
|
| 5. |
Prevalence of leprosy. 2013; Available from: www.gujhealth.gov.in [30/06/2014].
[Google Scholar]
|
| 6. |
World Health Organization. Global Strategy for Further Reducing the Leprosy Burden and Sustaining Leprosy Control Activities (Plan period: 2006-2010), WHO/CDS/CPE/CEE/2005.53, Geneva; 2005.
[Google Scholar]
|
| 7. |
Daumerie D. Active case finding for leprosy elimination, scoping meeting TB. World health organization, Geneva; 31/05/2011.
[Google Scholar]
|
| 8. |
Rao PS. Current epidemiology of leprosy in India. Lepr Rev 2006;77:292-4.
[Google Scholar]
|
| 9. |
De Souza MC, Dias GH, Nobre ML. The use of Geographical Information System (GIS) to improve active leprosy case finding campaigns in the municipality of Mossoro, Rio Grande doesNorte State, Brazil. Lepr Rev 2007;78:261-9.
[Google Scholar]
|
| 10. |
Lockwood DN. Leprosy elimination - a virtual phenomenon or a reality? BMJ 2002;324:1516-8.
[Google Scholar]
|
| 11. |
Desikan KV. Elimination of leprosy and possibility of eradication-the Indian scenario. Indian J Med Res 2012;135:3-5.
[Google Scholar]
|
| 12. |
Shetty VP, Thakar UH, D′souza E, Ghate SD, Arora S, Doshi RP, et al. Detection of previously undetected leprosy cases in a defined rural and urban area of Maharashtra, Western India. Lepr Rev 2009;80:22-33.
[Google Scholar]
|
| 13. |
Moura ML, Dupnik KM, Sampaio GA, Nóbrega PF, Jeronimo AK, do Nascimento-Filho JM, et al. Active surveillance of Hansen′s Disease (leprosy): Importance for case finding among extra-domiciliary contacts. PLoS Negl Trop Dis2013;7:e2093.
[Google Scholar]
|
| 14. |
Shetty VP, Doshi RP. Detection and classification of leprosy: Future needs and strategies. Indian J Lepr 2008;80:139-47.
[Google Scholar]
|
| 15. |
International Leprosy Association (ILA), International (Commanditaire). Epidemiology and control-Leprosy. Leprosy Review. 2002;73(Jun):S45-S52.
[Google Scholar]
|
| 16. |
Shetty VP. Challenges facing the control of leprosy in the Indian context. Ann Acad Med Singapore 2010; 39:1-3.
[Google Scholar]
|
Fulltext Views
3,710
PDF downloads
2,568





