Translate this page into:
Evidence of emerging sexually transmitted Mycoplasma genitalium infection among women detected using multiplex and uniplex PCR
Corresponding author: Dr. Deepti Tandon, Department of Clinical Research, ICMR-National Institute for Research in Reproductive and Child Health (NIRRCH), Mumbai, India. gdeepti167@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tandon D, Singh A, Kerkar SC, Sawant S, Tryambhake V, Munne K, et al. Evidence of emerging sexually transmitted Mycoplasma genitalium infection among women detected using multiplex and uniplex PCR. Indian J Dermatol Venereol Leprol. 2024;90:210–4. doi: 10.25259/IJDVL_39_2023
Abstract
Background
The Centre for Disease Control has recognised Mycoplasma genitalium as an emerging sexually transmitted infection. Sparse literature is available in India regarding Mycoplasma genitalium infection.
Aims
To evaluate the prevalence of Mycoplasma genitalium, its detection from samples obtained from various sites, evaluate co-infections and follow up after treatment.
Methods
A prospective study was conducted among 341 sexually active women presenting with the complaints of lower genital tract infection to the Municipal STD clinic and ART Centre. Endocervical swabs, vaginal swabs and urine samples were tested for Mycoplasma genitalium using uniplex and multiplex real-time PCR kits. Gram stain was used for diagnosing bacterial vaginosis and candidiasis. Data on HIV, RPR, TPHA, Hepatitis C and HBsAg were also collected.
Results
The mean age of the participants was 33.4 ± 5.7 years. Mycoplasma genitalium was found in 23 (6.7%) patients, while Neisseria gonorrhoeae and Chlamydia trachomatis were detected in 8 (2.3%) of the participants. The highest Mycoplasma genitalium positivity was in the endocervical swab sample at 6 (26%), followed by the urine sample at 4 (17.3%). The most common coinfection was HCV (33.3%), followed by syphilis (14.3%). The uniplex and multiplex kits showed 47.8% concordance for Mycoplasma genitalium in endocervical swab samples. Tobacco addiction was a significant risk factor for the Mycoplasma genitalium infection. Out of the 6 women who attended the follow up visit at the end of three months, a positive test for cure was seen in 4 (66.6%).
Limitations
Significant numbers of patients were lost to follow up. Also, the presence of anti-microbial resistance was not evaluated.
Conclusion
Mycoplasma genitalium is prevalent among women with high-risk behaviours, highlighting the need for further studies are needed among other high-risk populations.
Keywords
Mycoplasma genitalium
mycoplasma genitalium & Co-infections
STI clinic
RTI/STI
sexually transmitted infections
Plain Language Summary
Mycoplasma genitalium (MG) is an emerging sexually transmitted infection that has been increasingly reported worldwide. However, the prevalence and clinical dimension of this pathogen in India remain understudied. To address this gap, a clinic-based study was conducted among 341 sexually active women presenting with lower genital tract infections at a Municipal STD clinic and ART Centre. The study aimed to evaluate the prevalence of MG, its detection from various anatomical sites, associated co-infections, and treatment outcome.
The majority of the participants (88.3%; n = 301) were sex workers, and the overall prevalence of MG was found to be 6.7% (23/341). The highest positivity rate for MG was observed in endocervical swab samples 6 (26%). The most common co-infection was with hepatitis C virus (33.3%). Additionally, tobacco use was identified as a significant risk factor for MG infection. Of the women who received treatment, 4 (66.6%) were cured after three months.
The findings of this study suggest that MG has a high prevalence among women engaging in high-risk sexual behaviour, such as sex workers hence there is need to focus on this organism among other high risk population.
Introduction
Mycoplasma genitalium (MG) is considered an emerging sexually transmitted organism by the Centre for Disease Control (CDC) and is associated with various female reproductive morbidities.1 Active sexual behaviour and multiple sexual partners are important risk factors, and emerging antimicrobial resistance is becoming a major concern for MG infection. Though a few studies have reported on prevalence, there is still very sparse literature available in India regarding its prevalence, detection through various samples and kits, co-infections and tests of cure.2,3
Material and Methods
A clinic-based prospective study was carried out among 341 women who reported to the Municipal STD Clinic and ART Centre, Mumbai, from February 2020 to June 2022 with complaints of lower genital tract infection. Ethical approval for the study was obtained from the human ethics committee. After taking written informed consent, detailed clinical history was recorded as per a predesigned case record form. Three samples were collected per woman including an endocervical swab, a two-hour urine sample and a vaginal swab, thus a total of 1023 samples were collected. These were tested for MG using the Uniplex real-time PCR kit, an in-vitro diagnostics (IVD) approved MG FRT PCR kit (Curie Diagnostics, Artesia, CA).4 In addition, another endocervical swab was collected, on which multiplex testing was done using a fast track diagnostic urethritis plus multiplex real-time PCR kit to detect Chlamydia trachomatis (CT), Neisserria gonorrhoea (NG), Mycoplasma hominis (MH), Ureaplasma urealyticum (UU), Ureaplasma parvum (UP), Trichomonas vaginalis (TV) and MG. Gram stained vaginal smears were also examined for Nugent scores and budding yeast cells. The flowchart showing recruitment, sample collection and laboratory investigations of the women attending the sexually transmitted infections (STI) Clinic is shown in Figure 1.

- chart showing of recruitment, sample collection and laboratory investigations of the women attending STI Clinic
For real-time PCR test results, the samples showing an exponential florescence trace and CT value were considered positive. All MG positive women were called for follow up after three months, and retesting was done on endocervical, vaginal and two-hour urine samples using a real-time PCR to evaluate microbiological response to treatment. HIV testing (Combo AIDS kit) and rapid plasma reagin (RPR) are routinely done at the Municipal STD clinic and ART Centre. Other investigations, namely, HBsAg (ELISA, Meril Diagnostics), Hepatitis C (HCV) (ELISA, Meril Diagnostics) and TPHA (Treponema pallidum haemagglutination) (Passive haemagglutination, Omega Diagnostic) were done at the Regional RTI/STI Reference Laboratory of the Microbiology Department in Mumbai. The results of these investigations were noted. All women were treated as per syndromic protocol.
Results
The mean age of participants was 33.4 ± 5.7 years. The vast majority, 301 (88.3%), were commercial sex workers, and the rest 40 (11.7%) were in other occupations. Most of them (324, 95%) belonged to the upper lower socioeconomic class. About two-thirds of them (221, 64.8%) used public toilets, while the remainder (120, 35.2%) accessed private toilet facilities. Smoking and alcohol were reported by 33 (9.7%) and 94 (27.6%) participants, respectively, and 174 (51%) had addictions to smokeless tobacco. An overwhelming majority (301, 88.3%) had exposure to multiple sexual partners in the preceding 6 months and condom use was reported by 292 (85.6%). These women reported multiple symptoms including vaginal discharge in 213 (62.4%), vaginal itching in 139 (40.8%), urinary complaints in 86 (25.2%) and dyspareunia in 101 (29.6%). Clinically, 292 (85.6%) had cervicovaginitis and 45 (13.1%) had cervicitis.
MG was found in samples from 23 (6.3%) women. Out of these individually, maximum positive samples were detected in only 6 (26.08%) endocervical samples, followed by 4 (17.3%) urine samples. A combination of endocervical, vaginal and two-hour urine samples was positive for 6 (26.08%). Figure 2 represents the Venn diagram of percentage positivity for MG in samples from various sites.
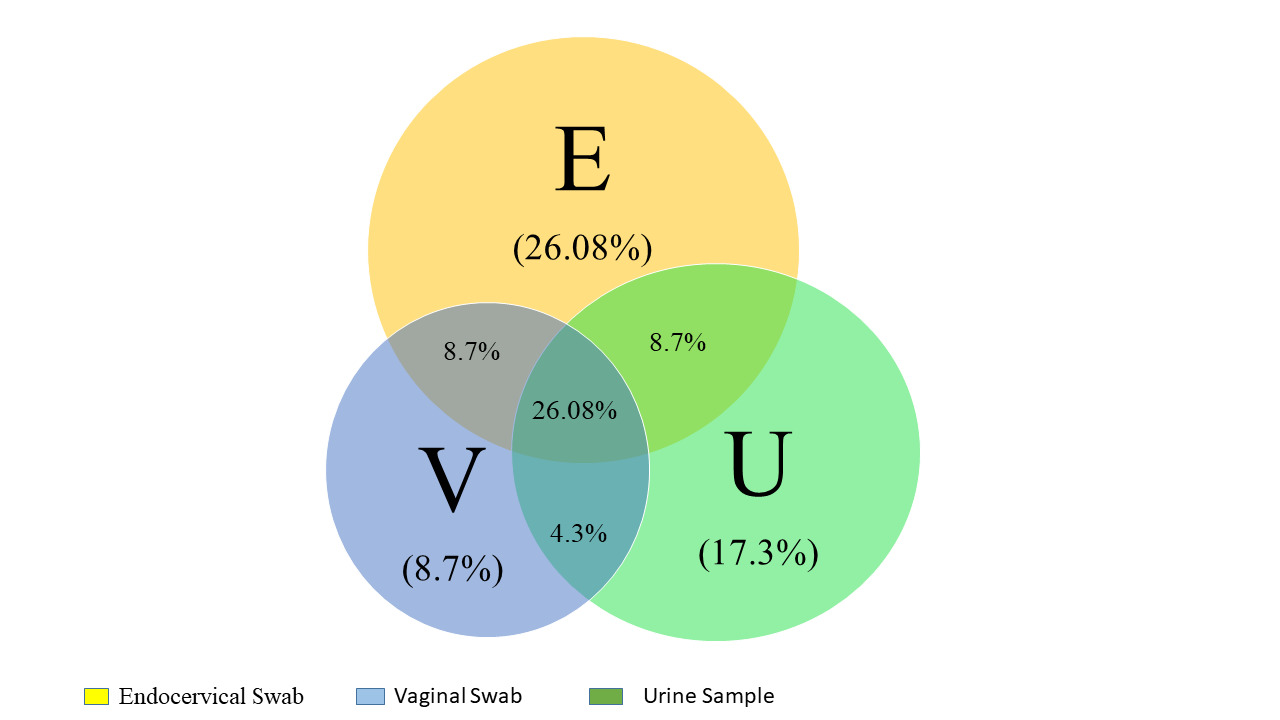
- Diagram of percentage positivity for MG in samples from various sites
There was a concordance of 47.8% among uniplex and multiplex kits, as 11 endocervical samples tested positive for MG with both kits.
Neisseria gonorrheae (NG) and Chlamydia trachomatis (CT) were detected in 8 (2.3%) each, out of which 3 (0.87%) were detected with both. Trichomonas vaginalis (TV) 5 (1.5%), Ureaplasma urealyticum (UU) 59 (17.3%), Ureaplasma parvum (UP) 74 (21.7%) and Mycoplasma hominis (MH) 204 (59.8%) were also detected. All three genital mycoplasma, UU, UP and MH, belong to mycoplasma species and were detected in 4 (1.17%) women. Seropositivity for HIV was seen in 50 (14.7%) women, 7 (2.1%) women were positive for syphilis by RPR and 24 (7.03%) women were positive for TPHA. Nine (2.6%) women were seropositive for HBsAg and 3 (0.9%) were seropositive for HCV. Bacterial vaginosis was detected in 76 (22.3%) women, whereas vaginal candidiasis was seen in 11 (3.2%) participants.
Co-infections with MG were found in the women who were also positive for HCV, RPR, TPHA, NG, CT, MH and HIV. Table 1 represents the co-infections among MG-infected women.
Addiction in the form of tobacco was found to be significantly associated with MG. A higher proportion of female sex workers have MG compared to women in other occupations. Women with HIV, HCV and RPR had higher prevalence of MG infection, though statistically significant results were obtained only in RPR-positive women. Condom use provided protection against MG infection, though statistically significant results were not obtained. Table 2 represents the associated risk factors for MG. Out of 23 women, 6 (26.08%) came for follow-up and 17 (73.9%) were lost to follow-up. Out of these six, four (66.6%) were negative for MG, and two (33.3%) were positive for MG at the end of three months.
| Coinfection | MG positive (n = 23) | MG negative (n = 317) | p value |
|---|---|---|---|
| n (%) | n (%) | ||
| Mycoplama hominis (n = 204) | 17 (8.3) | 187 (91.6) | 0.36 |
| Ureaplama Urealyticum (n = 74) | 2 (2.7) | 72 (97.2) | 0.187 |
| Ureaplasma parvum (n = 59) | 2 (3.3) | 57 (96.6) | 0.39 |
| Neisseria gonorrhoea (n = 8) | 1 (12.5) | 7 (87.5) | 0.43 |
| Chlamydia trachomatis (n = 8) | 1 (12.5) | 7 (87.5) | 0.43 |
| Trichomonas vaginalis (n = 5) | 0 (0) | 5 (100) | - |
| HIV (n = 50) | 4 (8) | 46 (92) | 0.75 |
| Hepatitis B (n = 9) | 0 (0) | 9 (100) | 0.41 |
| HCV (n = 3) | 1 (33.3) | 2 (66.7) | 0.19 |
| RPR (n = 7) | 1 (14.3) | 6 (85.7) | 0.07 |
| TPHA (n = 24) | 3 (12.5) | 21 (87.5) | 0.21 |
| BV (n = 109) | 8 (7.3) | 101 (92.7) | 0.76 |
HIV: Human immunodeficiency virus, HCV: Hepatitis C virus, RPR: Rapid plasma reagin, TPHA: Treponema pallidum haemaglutination test, BV: Bacterial vaginosis, STI: Sexually transmitted infection
| Risk factor | MG positive (Total 23) n (%) | p |
|---|---|---|
| Age | ||
| <29 | 5 (6.8) | 0.96 |
| ≥30 | 18 (6.7) | |
| Occupation | ||
| FSW | 21 (6.9) | 0.69 |
| Others | 2 (5.3) | |
| Toilet facility | ||
| Private | 8 (6.7) | 0.96 |
| Common | 15 (6.8) | |
| Addictions | ||
| Smoking | 6 (18.2) | 0.006* |
| Not smoking | 17 (5.5) | |
| Smokeless tobacco | 17 (9.8) | 0.04* |
| Non smokeless tobacco | 5 (3) | |
| Alcohol | ||
| Yes | 15 (6.1) | 0.42 |
| No | 8 (8.5) | |
| Condom use | ||
| Yes | 19 (6.5) | 0.67 |
| No | 4 (8.2) | |
| HIV | ||
| Reactive | 4 (8) | 0.70 |
| Non-reactive | 19 (6.5) | |
| RPR | ||
| Positive | 2 (28.6) | 0.02* |
| Negative | 21 (6.3) | |
| HBsAg | ||
| Reactive | 0 (0) | 0.4 |
| Non-reactive | 23 (6.9) | |
| HCV | ||
| Reactive | 1 (33.3) | 0.06 |
| Non-reactive | 22 (6.5) |
FSW: Female sex workers, HIV: Human immunodeficiency virus, RPR: Rapid plasma reagin, HCV: Hepatitis C Virus, STI: Sexually transmitted infection
Discussion
In the present study, we found a higher prevalence of MG as compared to other previous studies, which reported a prevalence of 1.2% and 0.5%, among men with urethral discharge and women with vaginal discharge respectively.2,3 Ours is probably the first study among high-risk women reporting MG as a highly prevalent organism, in contrast to previous findings from our community-based study in Mumbai showing no evidence of MG among women with low risk behaviour.5
The British Association for Sexual Health and HIV National guideline for the management of infection with MG (2018) recommends vaginal samples followed by endocervical swabs as the most sensitive for MG detection.6 However, our study reports that the majority of samples are positive in the endocervical swab, and we recommend using a combination of endocervical, vaginal and urine samples for better detection of MG. In our study, we found discordance in detection of MG by uniplex and multiplex kits. The weak performance of these multiplex kits for the detection of MG has also been reported in recent studies.7 The disparity in the detection rate can probably be attributed to the variation in the analytic sensitivity of the kits, as uniplex kits are known to detect 1 × 10 ≥ GE/mL.7 However, the advantage of multiplex kits to diagnose multiple pathogens in low-resource settings always exists.
MG has been reported as a common sexually transmitted infection among women with HIV infection. Co-infections with CT and NG are reported to be common among MG infected women similar to our study in which these organisms were reported in 12.5%, along with HCV also being the most common coinfection in 33.5%. Multiple sexual partners and sex without condoms are known risk factors for MG infection, and this is also evident from this study.
Though we had a significant proportion of lost-to-follow-up cases, we report a negative test of cure in 33.3%, which could be primarily due to reinfection, but the possibility of antimicrobial resistance cannot be ruled out.
An important finding is the high prevalence of MG as compared to CT and NG, suggesting a need to focus on this sexually transmitted infection among groups with high-risk behaviour. Syndromic management continues to play a pivotal role in the management of RTI/STI; however, periodically there is a need for etiological testing to generate evidence to detect non-classical sexually transmitted infection.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
ICMR Intramural grant.
Conflicts of interest
There are no conflicts of interest.
References
- Sexually transmitted infection treatment guidelines. Mycoplasma genitalium; 2021. [Last accessed on 2022 Oct 12]. Available from: https://www.cdc.gov/std/treatment-guidelines/mycoplasmagenitalium.htm
- Comparative analysis of syndromic case management and polymerase chain reaction based diagnostic assays for treatment of Neisseria gonorrhoeae, Chlamydia trachomatis and genital mycoplasmas in patients of genitourinary discharge. Indian J Med Microbiol. 2017;35:286-9.
- [CrossRef] [PubMed] [Google Scholar]
- Genital Mycoplasma and Chlamydia trachomatis infections in patients with genital tract infections attending a tertiary care hospital of North India. Indian J Pathol Microbiol. 2016;59:194.
- [CrossRef] [PubMed] [Google Scholar]
- [Last accessed 2022 Oct 12]. Available from: http://www.curiediagnostics.com/mycoplasma-genitalium/
- Cross sectional study to evaluate microbiological spectrum of RTI/STI and co-infections among women with cervicitis or cervico-vaginitis from a community clinic in Mumbai. Indian J Med Microbiol. 2022;40:144-6.
- [CrossRef] [PubMed] [Google Scholar]
- British association for sexual health and HIV national guideline for the management of infection with Mycoplasma genitalium . Int J STD AIDS. 2019;30:938-50.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical performance of four multiplex real-time PCR kits detecting urogenital and sexually transmitted pathogens. Clin Microbiol Infect. 2022;28:733e7-13.
- [CrossRef] [PubMed] [Google Scholar]






